FGDS is used not only for research, but also for the treatment of stomach diseases. In this way, for example, polyps, foreign bodies or early neoplastic changes are removed. With this test it is also possible to stop bleeding or widen a pathological narrowing (for example, of the esophagus). The indication for gastroscopy is suspicion of diseases of the upper digestive system. Symptoms that may indicate upper gastrointestinal disease include, for example, gastroesophageal reflux disease, heartburn, nausea, vomiting and belching.
Preparing for gastroscopy does not require much effort. The patient must come for examination on an empty stomach. Even drinking water and other liquids is prohibited. At least six hours must pass from the last meal to the examination. If the examination is carried out in the morning, then you should not have dinner in the evening.
During a gastroscopy, the doctor will definitely ask what medications the patient is taking. It is also necessary to mention any diseases or operations performed. If a person is already taking any medications, then he should take them with a small amount of water. Before gastroscopy, local anesthesia of the throat is usually used. It happens that it is necessary to use general anesthesia (especially in cases where gastroscopy is used as a therapeutic method). The endoscope tube is inserted through the mouth and throat into the esophagus. This method does not cause pain, but rather discomfort. A tube in the throat may cause vomiting, burping, or coughing. The procedure usually takes from five minutes to half an hour. After gastroscopy, the patient is under the supervision of specialists for several hours. If no complications arise, he is discharged from the hospital.
Complications after gastroscopy occur extremely rarely. Most often, their cause is the patient's reaction to general anesthesia. People with serious heart disease are more susceptible to complications after gastroscopy. A higher risk of complications occurs when the procedure is repeated more than once, as a treatment study.
X-ray examination
X-ray examination of the stomach received this name due to the use of an X-ray machine. The patient is injected with contrast - a special suspension that absorbs X-rays. The specialist then takes “pictures” showing the condition of the stomach - its position in relation to other organs and various abnormalities (for example, tumors or ulcers). X-ray examination is performed less frequently than gastroscopy, since the latter is much more effective and accurate.
An X-ray of the stomach is performed if diseases of the upper gastrointestinal tract are suspected. It is used to diagnose chronic diseases as well as medical emergencies such as gastric or duodenal perforation. Preparing for an x-ray of the stomach is quite simple. The patient comes for examination on an empty stomach, having not eaten since the evening before the hospital visit. Smoking is prohibited on the day of the examination. X-rays are prohibited for pregnant women due to the risk to the fetus. The entire examination process is painless and non-invasive. After drinking the contrast, the patient turns around its axis in a lying position so that the contrast spreads well along the walls of the digestive system. In order for photographs to be taken correctly, the subject must remove outer clothing and assume a vertical position. The examination process itself takes only a few minutes. After this, the patient can safely go home.
Diagnostic methods
Any diagnostic examination begins with a history taking. Patients come to see a gastroenterologist with obvious signs of organ pathology. Their complaints may be associated with painful sensations behind the sternum and in the chest. There may be dysphagia of varying severity, difficulty swallowing, a feeling of a lump in the throat and other symptoms indicating problems with the esophagus. The question arises: how to examine the esophagus, what research methods to choose?
Methods for studying the esophagus
For most, the relevant question is how to examine the esophagus. For this purpose the following is carried out:
- Examination of the patient, which includes a general examination of the esophagus and larynx. Particular attention is paid to the condition of the larynx. The doctor also performs palpation of the lymph nodes in the neck, palpation of the epigastrium and other forms of general examination.
- Instrumental methods: radiography , 24-hour pH monitoring , CT and spiral tomography , esophagofibroscopy , FGS , chromoscopy , biopsy , etc.
Since instrumental methods in examining the esophagus are of primary importance, it is worthwhile to dwell on them in more detail.
Esophagofibroscopy
This highly informative research method allows you to find out the condition of the mucous membrane of the esophagus along its entire length. And also - to identify the cause of pain, dysphagia, determine varicose veins, the presence of tumors and bleeding.
The manipulation is carried out for both diagnostic and therapeutic purposes. An endoscope with an ultrasound sensor is inserted through the patient's larynx into the esophagus, which examines the walls of the esophagus and collects biological material for histological examination.
The device has high performance in detecting the slightest deviations from the norm in the condition of the organ, therefore it is considered one of the most informative diagnostic methods used for examining the esophagus . The procedure is performed under anesthesia - local or general. First of all, this is a thorough anesthesia of the pharynx.
There are practically no contraindications for this method, with the exception of the patient having burns of the esophagus, severe diseases of the larynx, and an aortic aneurysm. Complications during the procedure may include contact bleeding and perforation of the esophageal wall.
Daily pH-metry
Based on the results of measuring the pH level in the esophagus, the nature and severity of reflux of the organ can be determined. The manipulation boils down to installing a probe with a sensor in the lower part of the esophagus. This device remains in the organ for 24 hours. What can be revealed based on the pH results:
- the state of the acid formation process during the day under natural conditions of organ functioning;
- the effect of medications on the level of acidity in the esophagus;
- level of resistance to taking antisecretory drugs;
- functional state of the esophagus and stomach before and after surgery.
Fecal occult blood test
Blood in the stool can indicate many serious diseases - not only polyps or ulcers, but also cancer (for example, colorectal cancer). Suspicion of these diseases may prompt your doctor to recommend a stool occult blood test. Stool samples are analyzed using a microscope and chemical and bacteriological tests.
Most often, a stool occult blood test is prescribed for suspected diseases of the digestive system. In people over 50 years of age, it is used as a screening test for colorectal cancer. It is also recommended for suspected diseases such as polyps, ulcers, adenomas or hemorrhoids.
Special preparation is required before taking this test. Three days before the examination, you should not eat meat or green vegetables. It is better to replace them with more fiber. You should also avoid taking oral medications such as vitamin C, iron, and aspirin. You should also not use laxatives. They will interfere with analyzing the condition of stool.
The accuracy of the test results depends on the type of test, whether it is the guaiacol gFOBT method, the iFOBT immunochemical method or the porphyrin test. In most cases, stool samples are collected three days in a row. The test is completely non-invasive. The normal fecal occult blood test result is 0.5 to 1.5 ml/day.
Esophagoscopy
Esophagoscopy of the esophagus is one of the main and most informative ways to check the esophagus and larynx for various pathologies. It is carried out using an optical instrument - an esophagoscope . Its design consists of a lighting fixture, a set of tubes of various diameters and lengths and auxiliary tools.
Depending on the purpose, esophagoscopy is performed either for therapeutic purposes or for diagnostic purposes. Carrying out the procedure requires caution from the specialist, since vital organs are located near the esophagus, and the esophagus itself, in various pathologies, has a very traumatic mucosa. What does esophagoscopy provide:
- functional state of the esophagus;
- its anatomical changes - narrowing, the presence of neoplasms;
- condition of the mucosa, the presence of atrophic or ulcerative processes.
The procedure is carried out on an empty stomach, and half an hour before it begins, the patient is injected subcutaneously with atropine and promedol to relieve unpleasant pain.
Serological study
To carry out a serological test, it is enough to donate blood. The collected sample is analyzed for the presence of antibodies or antigens. In the case of the stomach, specialists look for antibodies in the blood against the bacterium Helicobacter pylori, which causes numerous gastric diseases. It also provokes stomach ulcers. In very advanced cases, lack of treatment can lead to cancer.
There is no need to prepare for a serological test. There are also no contraindications to it. If treatment for the gastrointestinal tract has already been completed, and the text shows a positive result, do not be alarmed. Antibodies can remain in the body for a long time. That is why serological testing of the stomach cannot be the only method for diagnosing gastrointestinal diseases.
How to check your stomach using Gastropanel
Indicators determined using Gastropanel
The test panel provides a simple and reliable way to obtain information about the structure and function of the gastric mucosa. The following parameters are determined in the blood on an empty stomach:
- Pepsinogen I, Pepsinogen II and their ratio,
- Gastrin-17 and stimulated Gastrin-17,
- antibodies to gastric parietal cells,
- antibodies to Helicobacter pylori IgG and IgA.
Blood Test Panel Helps Answer Questions
- does the patient suffer from gastritis caused by Helicobacter pylori,
- Is gastritis atrophic and in which part of the stomach are these changes localized?
- whether the patient is at risk of developing peptic ulcers or stomach cancer,
- Is it necessary to do a mandatory esophagogastroduodenoscopy with biopsy,
- whether there is autoimmune atrophic gastritis with damage to the body of the stomach, which determines a high risk of disorders associated with vitamin B12.
Ultrasound
Ultrasound examination makes it possible to determine anatomical and histological changes in the esophageal tube. It is prescribed during the study:
- hiatal hernia
- suspicion of the development of neoplasms;
- achalasia of the cardinal sphincter;
- esophagitis;
- developmental anomalies of the esophageal tube;
- diverticulum.
Since pathologies are often combined with pathologies of the stomach, examination of these organs is carried out simultaneously.
To prepare for the study, it is necessary to exclude from the diet foods that cause gas formation in the stomach. The procedure is carried out on an empty stomach, the last meal should be no later than 19 hours on the eve of the ultrasound.
The ultrasound procedure is selected by a specialist individually for the patient, taking into account the data of the clinical study, previously performed diagnostic procedures and the anatomical characteristics of the patient.
This could be an ultrasound:
- percutaneous;
- intraesophageal;
- with water-siphon sample;
- endosonoscopy.
Before the study, the patient is informed about the method, features of its implementation and effectiveness.
Ultrasound establishes:
- erosions and ulcerative lesions of the walls of the esophageal tube;
- the condition of the organ mucosa to confirm or exclude the presence of esophagitis;
- exact location of polyps ;
- presence of gastroduodenitis ;
- degree of effectiveness of the treatment.
Radiography
X-ray examination of the esophagus and stomach is performed on an empty stomach. Before the procedure, the patient drinks a special contrast agent (barium sulfate in solution). When conducting the study, attention is paid to the features of the contours of the organ, its peristalsis, the relief state of the mucous membrane, and the degree of functionality of the sphincters.
The method is informative in diagnosing neoplasms in the esophageal tube and stomach and is actively used in pathologies of these organs.
Read more about this study in this article.
Biopsy
This is a diagnostic procedure that is performed on tissue samples from the affected organ, in this case the esophageal tube. Cytological examination of tissues is performed under a microscope mainly to identify cancer cells. At the same time, specialists not only give an opinion about the presence of cancer cells, but also determine whether they belong to a particular type of tumor.
In addition to oncology, a biopsy of the esophagus makes it possible to diagnose some autoimmune pathologies, infectious diseases, and precancerous conditions . After the biopsy, the patient is not recommended to take hot or traumatic food for the mucous membrane of the organ for 24 hours.
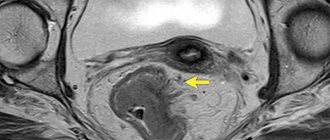
CT scan
This method has recently been used quite widely in the diagnosis of neoplasms and metastases, and in determining the thickness of organ walls. Unlike X-ray examination, CT provides a higher quality image.
A type of X-ray examination, spiral tomography produces highly accurate 3D models that are converted into digital data. These methods are quite informative and are often used in the diagnosis of pathologies of the gastrointestinal tract as additional methods when the previous diagnosis was not effective.
The relevance of timely and high-quality diagnostics
Timely and high-quality diagnosis for diseases of the esophageal tube can reduce the number of severe complications that can lead to resection of this organ.
This operation is prescribed for the following conditions:
- cancer;
- severe organ injury;
- severe forms of esophagitis;
- Barrett's disease;
- chemical burns;
- severe complications after a previous operation.
The operation itself, when it is necessary to remove the esophagus, also has consequences. This is a rather technically complex operation that requires high professionalism from the surgeon. During the operation, complications may occur in the form of bleeding and damage to organs located near the esophageal tube.
But more severe consequences may occur after surgery. The ability of the gastrointestinal tract to digest fats and sugars decreases. This can lead to dumping syndrome, a severe muscle spasm that causes food to be rejected from the body. After organ removal, the patient needs a special diet and small portions of food.