When food enters the gastrointestinal tract, the pancreas secretes into the small intestine not only pancreatic enzymes, but also bicarbonates, which neutralize hydrochloric acid and maintain an alkaline environment in the duodenum, necessary for the normal functioning of enzymes. Under physiological conditions, the pancreas (depending on age) produces from 50 to 1500 ml of secretion per day. Pancreatic juice is a colorless liquid with an alkaline reaction (pH = 7.8–8.4). It contains organic substances (proteins) and inorganic components (bicarbonates, electrolytes, trace elements), as well as mucus of the excretory ducts. The enzymatic part of the secretion is formed in acinar cells, and the liquid (water-electrolyte) part - mucin and bicarbonates - in the epithelium of the ducts. With the help of pancreatic enzymes (lipase, amylase and proteases), which play a key role in the exocrine function of the pancreas, nutrients are broken down (Table 1). Most enzymes are in an inactive form as proenzymes, which are activated in the duodenum by enterokinase (Fig. 1). Lipase, amylase and ribonuclease are secreted in active form.
Amylase is secreted not only by the pancreas, but also by the salivary glands. Both of its forms have approximately the same activity and are involved in the breakdown of starch and glycogen. Salivary gland amylase can digest starch before it enters the small intestine and comes into contact with pancreatic amylase. Amylase hydrolyzes the α1,4 glycosidic bonds of starch and glycogen, but is unable to cleave the α1,6 bonds, which are hydrolyzed by intestinal brush border enzymes.
Pancreatic lipase catalyzes the breakdown of dietary triglycerides into two fatty acids and a monoglyceride. It acts together with bile acids and pancreatic colipase.
Proteases are synthesized by the gland as precursors, which are activated in the duodenum. As a result of the action of all peptidases (trypsin, chymotrypsin, elastase, carboxypeptidases), oligopeptides are formed, which are further broken down by brush border enzymes, as well as free amino acids.
The proteolytic activity of the digestive juice of the pancreas is at a fairly high level already from the first months of life, reaching a maximum by 4–6 years. Lipolytic activity increases during the child's first year. The activity of pancreatic amylase by the end of the first year of life increases 4 times, reaching maximum values by 9 years.
The activity of pancreatic enzymes depends on the living conditions of the organism and is adaptive in nature [2]. So, according to R.M. Kharkova (1976), with natural feeding the concentration of pancreatic enzymes in duodenal juice is low, with mixed feeding it increases by 1.5–2 times, and with artificial feeding it increases by 4–5 times [3].
Regulation of pancreatic juice secretion is a complex process in which neurohumoral mechanisms are involved, with an important role played by humoral factors - gastrointestinal hormones (secretin, cholecystokinin-pancreozymin), activated by the action of releasing peptides secreted in the mucous membrane of the duodenum. Secretin enhances the production of the liquid part of the juice, and cholecystokinin-pancreozymin stimulates the enzymatic activity of the pancreas. Insulin, gastrin, bombensin, bile salts, serotonin also enhance the secretory activity of the latter. The secretion of pancreatic juice is inhibited by glucagon, calcitonin, somatostatin, etc.
Exocrine pancreatic dysfunction occurs in various diseases and may be the result of a general or isolated decrease in its enzymatic activity. Often, enzyme deficiency is caused by a violation of their activation in the small intestine. Due to pancreatic dysfunction, accompanied by enzyme deficiency (maldigestion), malabsorption of nutrients (malabsorption) often develops (Table 2).
It is known that the pancreas has great compensatory capabilities and a violation of pancreatic secretion manifests itself only when it is severely damaged. Steatorrhea and creatorrhea in adults develop when the secretion of pancreatic lipase and trypsin decreases by more than 90% [4].
Clinical signs of exocrine pancreatic insufficiency: - diarrhea; - flatulence; - stomach ache; - steatorrhea; - nausea; - recurrent vomiting; - loss of appetite; - general weakness; - weight loss; — decrease in physical activity; - growth retardation (with severe forms of maldigestion).
Exocrine pancreatic insufficiency is based on the following mechanisms (5 modifications): - immaturity of the pancreas; — destruction of acinar cells (decreased enzyme synthesis); - obstruction of the pancreatic duct, interfering with the flow of pancreatic juice into the duodenum; - a decrease in the secretion of bicarbonates by the epithelium of the pancreatic ducts, leading to acidification of the contents of the duodenum to pH 4.0 and below, resulting in denaturation of pancreatic enzymes and precipitation of bile acids; — insufficiency of enzyme activation due to deficiency of enterokinase and bile; — dyskinesia of the duodenum and small intestine, as a result of which there is a violation of the mixing of enzymes with food chyme; — disruption of intestinal microbiocenosis (inactivation and destruction of enzymes); - hypoalbuminemia due to protein deficiency in food (impaired enzyme synthesis).
Depending on the mechanism underlying the development of exocrine pancreatic insufficiency, absolute pancreatic insufficiency is distinguished, which develops with a decrease in the volume of functioning pancreatic parenchyma, and relative, caused by reasons not directly related to the pancreas: a decrease in the intraduodenal pH level less than 5.5; motor dysfunction of the duodenum; rapid transit of intestinal contents; bacterial overgrowth in the small intestine; deficiency of bile and enterokinase (Table 3).
If symptoms indicating exocrine pancreatic insufficiency are identified, it is necessary to begin pancreatic enzyme replacement therapy early, before the development of malabsorption [6].
Pancreatic insufficiency can occur with a general decrease in the production of all enzymes by the pancreas, or with an isolated decrease in one of them. Below are the groups of main diseases accompanied by exocrine pancreatic insufficiency: - chronic pancreatitis; - acute pancreatitis; - cystic fibrosis; — congenital pathology of the pancreas; - primary sclerosing cholangitis; - pancreas injury; - pancreatic tumor.
With all the variety of diseases accompanied by pancreatic insufficiency, the doctor’s task is to, after conducting a differential diagnosis, establish its cause and carry out timely correction. To clarify the diagnosis and identify exocrine pancreatic insufficiency, various research methods are used.
Laboratory research methods include determining the content of pancreatic enzymes in the blood and urine.
The following indicators are of greatest importance: - in acute pancreatitis, an increase in the level of amylase in the blood and urine by 5–10 times, and this is especially true for amylase isoenzymes in the blood; - levels of amylase and lipase in the blood during exacerbation of chronic pancreatitis can be normal or briefly increased by 1–2 times; - “hyperamylasemia” after provocation with proserin, pancreozymin, glucose indicates an outflow disorder or inflammation of the pancreas; — the appearance of elastase-1 in the blood plasma and its increase reflect the severity of inflammation in pancreatitis; - an increase in the level of trypsin in the blood serum, a decrease in its inhibitor and a decrease in the inhibitor/trypsin ratio indicate an exacerbation of pancreatitis [3]; — with the progressive course of chronic pancreatitis, the level of immunoreactive trypsin decreases, and the trypsin/insulin ratio indicates the phase of the disease.
Diseases that may be accompanied by increased levels of pancreatic enzymes are presented in table. 4 [7].
In recent years, data have emerged on the greater diagnostic value of serum concentrations of inflammatory mediators - tumor necrosis factor (TNF) and interleukin (IL-6) in predicting the outcome of pancreatic diseases occurring with severe exocrine insufficiency in the acute period, compared to C-reactive protein (SRB). AC de Beaux et al. It was shown that in patients with acute pancreatitis, already on the first day of the disease, there is a progressive and significant increase in the average concentrations of TNF and IL-6, while an increase in the level of CRP was noted only on the 3rd day of the disease. In addition, the researchers noted that serum inflammatory markers were higher in patients who subsequently developed organ damage.
Scatological research
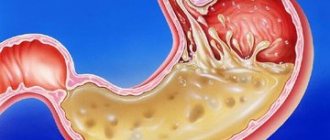
It should be recognized that coprological research has not lost its relevance to this day and is the most accessible method that can confirm the presence of exocrine pancreatic insufficiency. With functional pancreatic insufficiency, accompanied by a deficiency or decrease in the activity of pancreatic enzymes, the process of breakdown and absorption of nutrients in the intestine is disrupted. This is primarily reflected in the appearance of feces: - the stool becomes bulky, “polyfecal matter” appears; - feces acquire a grayish tint and have a “greasy” appearance; - excrement develops a fetid, putrid odor.
A scatological examination should be carried out before prescribing pancreatic enzymes. In this case, the following pathological signs are revealed: - steatorrhea
— determination of neutral fat in feces (type 1 steatorrhea);
fatty acids, soaps (type 2 steatorrhea); both together (type 3 steatorrhea); - creativeorrhea
- a large number of muscle fibers (++ or +++), of which there are normally very few in feces;
- amilorrhea
- the appearance in the feces of many starch grains, indicating a violation of the breakdown of carbohydrates, which is rare in patients with pancreatic insufficiency due to the high activity of intestinal amylase.
In case of mild disorders of the exocrine function of the pancreas, scatological examination, unfortunately, is not always informative.
The earliest sign of exocrine pancreatic insufficiency is steatorrhea; creatorrhea appears much later; amilorrhea is rarely observed.
The study of the content of pancreatic enzymes in duodenal secretions (basal, when stimulated with secretin (1 unit/kg), 0.5% hydrochloric acid, pancreozymin (1 unit/kg)) allows us to determine the types of secretion [8–10]:
A. Hypersecretory type,
observed with mild inflammatory-dystrophic changes in the pancreas. It is characterized by a high concentration of enzymes with normal or increased secretion volume and bicarbonate levels.
B. Hyposecretory type,
characteristic of pancreatic fibrosis. In this type, there is normal or reduced juice volume and bicarbonate levels with decreased enzyme activity.
B. Obstructive type,
detected when the duct is obstructed due to papillitis, duodenitis, spasm of the sphincter of Oddi. In this case, there is a reduced volume of juice with a normal content of enzymes and bicarbonates.
Quantitative determination of fat in feces
The fat content in stool is assessed qualitatively (adding Sudan dye to the stool) and quantitatively, the most informative method [1]. It allows you to summarize the total amount of fat in feces, taking into account fat of exogenous (food) origin. Normally, no more than 10% of the fat introduced with food is excreted in feces. In diseases of the pancreas, its amount sometimes increases to 60% [11].
Determination of elastase-1 in feces
Elastase-1 is a proteolytic enzyme of the pancreas with a molecular weight of about 28 mDa. It is known that human pancreatic elastase does not change its structure as it passes through the gastrointestinal tract. This circumstance suggests that the concentration of elastase-1 in feces reflects the degree of exocrine pancreatic insufficiency [12–14]. These data served as the basis for the development in the 1990s of an enzyme-linked immunosorbent method for determining pancreatic elastase (E-1) in stool, which is highly informative and specific.
According to N.I. Kapranova et al. (2001), the sensitivity of the method for diagnosing cystic fibrosis was 86.6%, and for detecting pancreatic insufficiency in patients with cystic fibrosis - 93% [12].
This method has qualitative advantages over other currently used methods for detecting exocrine pancreatic insufficiency (fecal lipid profile, coprogram, determination of chymotrypsin in feces) due to: - specificity; - its non-invasiveness; — no effect of enzyme replacement therapy on the results of the elastase test.
Range of normal values of the E-1 test: - normal activity of elastase-1 in the stool in children over 1 month. and adults is more than 200 mcg/g of feces; - fluctuations in elastase-1 activity in stool from 100 to 200 mcg/g of feces indicate a moderate degree of exocrine pancreatic insufficiency; — a decrease in elastase-1 activity in stool to less than 100 μg/g of feces reveals a severe degree of pancreatic insufficiency [13].
However, literature data on the use of this technique are contradictory. Thus, a number of authors claim that the determination of fecal elastase-1 is superior in sensitivity to other methods for diagnosing chronic pancreatitis, but the results obtained are unreliable in the case of a mild course of the disease. According to PG Lankisch et al., assessing the level of fecal elastase-1 helps only in determining the severe form of exocrine pancreatic insufficiency. The authors believe that the results do not reliably correlate with the severity of morphological changes that are observed in chronic pancreatitis [15].
Thus, the use of an elastase test makes it possible to determine or exclude exocrine pancreatic insufficiency (in acute and chronic pancreatitis, cystic fibrosis, Shwachman syndrome, isolated lipase deficiency), and also, without canceling enzyme therapy, to monitor the state of the exocrine function of the organ.
Diagnosis of functional pancreatic insufficiency
A complication and diagnostic criterion for chronic pancreatitis is exo- and/or endocrine pancreatic insufficiency. An increase in the number of surgical interventions performed for pancreatic diseases leads to an increase in the life expectancy of patients. At the same time, due to the development of exo- and/or endocrine pancreatic insufficiency, the quality of life of patients often decreases. Timely detection and correction of these conditions are carried out based on the assessment of laboratory indicators of the functional activity of the pancreas. The article discusses various diagnostic methods, their sensitivity, specificity, and diagnostic significance.
The pancreas (P) is an organ that has both an exocrine function, which consists of the production of digestive enzymes and bicarbonates, and an intrasecretory function, which consists of the synthesis of hormones that regulate carbohydrate metabolism.
The exocrine function is performed by most of the pancreas, which is represented by acini and the ductal system. The pancreatic secretion contains various groups of enzymes: proteolytic and nucleolytic enzymes (trypsin, chemotrypsin, carboxypeptidase, elastase, nuclease, aminopeptidase, collagenase, dipeptidase), amylolytic enzymes (amylase, maltase, lactase, invertase) and lipolytic enzymes (lipase, phospholipase, cholinesterase, carboxylesterase, monoglyceride lipase, alkaline phosphatase). Trypsin breaks down proteins into amino acids and is released as inactive trypsinogen, which is activated by enterokinase in the lumen of the small intestine. Chymotrypsin is released in the form of inactive chymotrypsinogen, activated by trypsin and breaks down proteins and polypeptides into amino acids. Elastase acts on connective tissue proteins - elastin and collagen.
The endocrine function is performed by the islets of Langerhans, which include α-cells that produce glucagon, β-cells that produce insulin, and δ-cells that produce somatostatin. β-cells synthesize proinsulin, which is broken down into C-peptide and insulin molecules. Regulation of insulin production occurs through a feedback mechanism depending on blood glucose levels. To a certain extent, glucagon, secretin and somatostatin have this property.
The functional activity of the pancreas is also influenced by humoral mechanisms. When the acidic contents of the stomach enter the duodenum, prosecretin is released in the intestinal cells, from which secretin is formed under the influence of hydrochloric acid. The latter in turn stimulates pancreatic secretion. Under the influence of secretin, a large amount of pancreatic juice is formed, poor in enzymes and rich in alkaline compounds. The amount of enzymes in pancreatic juice is determined by the influence of pancreozymin. Neuropeptides inhibit the secretion of pancreatic juice - gastroinhibitory polypeptide, pancreatic polypeptide and vasoactive intestinal polypeptide.
Exo- and/or endocrine pancreatic insufficiency is most often a complication and criterion for the diagnosis of chronic pancreatitis [1], as well as surgical treatment of pancreatic diseases, during which its normal anatomy and physiology are changed [2]. Exocrine pancreatic insufficiency and pancreatogenic diabetes mellitus require timely diagnosis and correction.
Exocrine pancreatic insufficiency
Despite the large number of existing methods for diagnosing exocrine pancreatic insufficiency (EPI), an ideal method does not currently exist. In clinical practice, the diagnosis of EPI is often based only on clinical manifestations (steatorrhea, flatulence and malabsorption) and response to enzyme replacement therapy (ERT) [3]. However, these parameters may not be reliable enough, and the lack of clear laboratory and instrumental markers can lead to errors in diagnosing EPI, as well as the prescription of incomplete and untimely ERT [4]. Thus, modern clinical tests are needed to detect EPI in patients of varying severity using uniform criteria.
Direct and indirect functional tests have been proposed to diagnose EPI.
The principle of direct invasive testing of pancreatic function is to determine its secretory capacity by analyzing the contents of pancreatic secretions. Since basal pancreatic secretion varies greatly, it is necessary to use physiological (food intake) or hormonal (secretin, cholecystokinin or its analogues) stimulants [5]. Direct functional tests are the most sensitive [6, 7], as they are based on direct measurement of the components of pancreatic secretion (bicarbonate and/or digestive enzymes).
The concept of direct testing of pancreatic function was first described 60 years ago by HO Lagerloef, who used secretin as a stimulator of pancreatic secretion [8]. Subsequently, various modifications of the method were carried out using several hormonal stimulants (secretin or cholecystokinin or a combination of secretin and cholecystokinin). However, attempts to form a unified protocol did not lead to consensus [3].
Secretin test
Measures the ability of the pancreas to produce bicarbonate in response to secretin stimulation. The sensitivity of the test varies from 72 to 94% in patients with established chronic pancreatitis (CP) according to imaging data [9, 10]. Several methods for performing the secretin test have been described.
The one-hour secretin test is a traditional direct test. Under endoscopic control, a double-lumen probe is inserted to separately collect the contents of the duodenum (DU) and stomach. Then fluoroscopic control of the probe placement is performed. After intravenous administration of secretin, the contents of the duodenum are aspirated every 15 minutes for an hour. The bicarbonate concentration in the obtained samples is determined [7]. According to several studies, the sensitivity and specificity of the traditional test, in which pancreatic secretions were collected continuously for an hour, varied in the range of 60–94% and 67–95%, respectively [4, 5]. The traditional test has high sensitivity, but its disadvantage is the complex methodology and the need to attract additional specialized personnel [7]. To simplify it, they began to analyze the aspirate after 30 and 45 minutes, but this led to a decrease in diagnostic accuracy compared to the standard one-hour collection [8].
Due to the laboriousness of the traditional secretin test, an endoscopic secretin test has been developed, which is performed under sedation, thereby improving patient acceptance of the test [11]. It was noted that, in contrast to the traditional test, analysis of duodenal aspirate obtained 30–45 minutes after secretin administration is sufficient for screening EPI, which simplifies its implementation [12]. The results of a retrospective study by S. Albashir et al. showed the sensitivity and specificity of the endoscopic secretin test to be 86 and 67%, respectively, in patients with CP [6]. Standard doses of sedation did not reduce pancreatic secretory capacity, but when more analgesia was required, abnormal results were obtained [13]. In recent years, a number of researchers have used this test to diagnose CP. FL Luis et al. found a positive predictive value of a 20-minute endoscopic test of 87.5% and a negative predictive value of 100% when compared with histological examination of the pancreas in patients with CP [14].
Cholecystokinin test
Based on the quantitative assessment of lipase activity in duodenal contents after stimulation with cholecystokinin. The principle of the test is similar to the secretin test. The standard technique involves the use of a double-lumen gastroduodenal tube and X-ray guidance. L. C. Darwin et al. used the cholecystokinin test to diagnose exocrine insufficiency in CP, the results showed high sensitivity and specificity of the method (92 and 95%, respectively). The endoscopic modification of the test in the study made it less cumbersome and more effective compared with the traditional method of collecting duodenal aspirate [15].
Cholecystokinin-secretin test
Simultaneous stimulation of the pancreas with secretin and cholecystokinin provides an assessment of the secretory capacity of the ducts and acini. The technique is similar to the traditional secretin test, but two hormones were used as stimulants - secretin and cholecystokinin. Several dosing regimens and different routes of administration (bolus injection or continuous infusion simultaneously or sequentially) have been studied for the early diagnosis of exocrine dysfunction or CP. Other studies calculated the secretion rate, that is, the amount of enzyme that was secreted by the gland per minute. This value characterized the voltage, intensity of enzyme secretion or flow rate per minute [16]. However, doubts have been raised whether the use of combined stimulation improves test sensitivity [16]. Several studies have used the cholecystokinin-secretin test to diagnose EPI in patients with CP, but have shown low sensitivity. In the work of H. A. Heij et al. The sensitivity of the secretin-cholecystokinin test was 81% when assessing functional disorders and structural changes in the pancreas in 25 patients with CP [18]. In another study by T. Hayakawa et al. In 108 patients with abdominal pain and suspected CP, the sensitivity of the secretin-cholecystokinin test, compared with histological changes in the pancreas, was 67% [19].
Lund test
The basis of the test is the use of a physiological stimulant (food intake) [20] to determine pancreatic function. A probe is placed into the duodenum to aspirate the contents of the duodenum. The patient takes a 300 ml liquid meal containing 5% protein, 6% fat and 15% carbohydrates. Next, the contents of the duodenum are aspirated for two hours and the activity of trypsin, lipase and amylase in the aspirate is measured [21]. The sensitivity of the Lund test varies from 66 to 94% [19, 22]. Ambiguous indicators of sensitivity and specificity of the Lund test compared to tests that used secretin and cholecystokinin as stimulants led to the abandonment of this method [23].
Thus, despite good sensitivity, direct tests are invasive, time-consuming, expensive, and uninformative for monitoring the effectiveness of ERT. Moreover, they do not have standardized protocols. Reproduction of these techniques is available only in specialized research centers and is not used in clinical practice [7]. In addition, direct tests have a number of contraindications for use, especially in patients with complicated CP and operated patients.
Indirect tests assess the consequences of impaired exocrine pancreatic function, that is, the result of inadequate production of digestive enzymes, bicarbonate or insulin [3].
72-hour fecal fat excretion test
This test is considered the gold standard for diagnosing EPI [24, 25]. The procedure involves following a high-fat diet (100 g per day) for at least two days before stool collection and for three days during collection. The disadvantages of the test are the difficulty of conducting the study for patients and medical personnel [26], as well as the high probability of false negative results if the diet is not followed carefully.
Fecal elastase assessment (E-1)
Elastase is a pancreatic secretion product that remains relatively stable when passing through the gastrointestinal tract; test results do not depend on ERT [27, 28]. The test is easily reproducible and requires a small volume of stool to be subjected to a monoclonal antibody immunoabsorption assay. The method has high sensitivity for diagnosing steatorrhea, but low specificity [29]. JE Dominguez-Munoz et al. proposed to consider the E-1 indicator together with an assessment of the symptoms and nutritional status of patients [30]. RR Vanga et al. [31] found in their study the E-1 test to be a potentially informative diagnostic tool for the diagnosis of EPI compared with the secretin test and fecal fat assessment. However, the need for larger studies was noted to determine the diagnostic value of this biomarker and optimal conditions for use in clinical practice. According to a study by J.-H. Lim et al., whose goal was to evaluate the impact of E-1 levels on the survival of patients with pancreatic cancer (PCa), found that a decrease in E-1 levels is an unfavorable independent prognostic factor for relapse-free survival for patients with PCa after resection [28]. DC Sudipta et al. [32] concluded that E-1 is a sensitive test for the diagnosis of EPI, but has low specificity and does not correlate with fecal fat excretion results at 72 hours, so the E-1 test cannot be used in isolation. However, this test may be useful as a screening test for EPI in patients with CP. However, the E-1 score is commonly used as the standard test for diagnosing EPI in most centers around the world because it is noninvasive, less labor intensive, less expensive, and does not require special diet [33]. The priority of E-1 assessment for determining EPI has been noted by many consensuses [2, 34, 35].
Relatively recently, a rapid elastase-1 test (ScheBo Biotech AG, Giessen, Germany) has appeared for the diagnosis of EPI, which uses test strips with monoclonal antibodies. The appearance of a pink control line (C) ensures that the application of the sample is performed correctly, and the appearance of two lines indicates sufficient exocrine function of the pancreas, and accordingly the concentration of E-1 in the feces is more than 200 μg/g [36]. The rapid test is based on the same immunochemical reaction as the E-1 test (ELISA), but can be performed outside specialized laboratories, and results are available within minutes. The diagnostic accuracy of the rapid test was compared with the E-1 test (ELISA) in 126 patients, predominantly with cystic fibrosis. The results showed high sensitivity and specificity (92.8 and 96.6%, respectively) [35]. In another study, the rapid test showed lower sensitivity (50%) and specificity (84%) when compared with the traditional E-1 assessment in patients with potential EPI after pancreatic surgery, CP, PCa, recurrent acute pancreatitis and autoimmune pancreatitis [31]. Research results show that the new rapid test is inferior to the traditional test, despite the fact that both are based on the same immunochemical reaction [33].
Determination of fecal chymotrypsin
Chymotrypsin is another pancreatic enzyme that has been used for several years as an indirect test for the diagnosis of EPI [37]. The test technique is simple. The analysis requires a small volume of feces; storing the material for several days does not affect the concentration of chymotrypsin. However, chymotrypsin has lower sensitivity and specificity for EPI compared to E-1 [38]. In addition, chymotrypsin is susceptible to enzymatic action when passing through the gastrointestinal tract and, given its presence in pancreatin preparations, ERT should be discontinued 72 hours before testing. Determination of EPI by this method is not widely used due to low sensitivity and the influence of ERT on the test results.
Serum trypsinogen
In clinical practice, the determination of pancreatic enzymes is used to diagnose acute conditions in diseases of the pancreas; in addition, changes in the concentration of serum enzymes can be used to assess its function. In some cases, serum trypsinogen is of diagnostic value, the determination of which is an inexpensive and widely available method [39]. The trypsinogen test, when measured repeatedly in the blood serum, is highly sensitive for progressive EPI and is a valuable tool for monitoring the condition of the pancreas. However, the method has low sensitivity for the primary diagnosis of EPI [40] and is not specific, and the concentration of trypsinogen increases in acute pancreatitis and abdominal non-pancreatogenic pain [41].
The use of other methods (test with 75Se-selenomethionine, determination of the degree of consumption of plasma amino acids, pancreatic lauryl test, NBT-PABA test, Schilling test) did not lead to a clear understanding of the functional state of the pancreas in its diseases. The disadvantage of these tests was the influence of ERT, metabolism in the small intestine and liver, and therefore sensitivity and specificity decreased, and false-positive results were often recorded [42−50].
13C-triglyceride breath test (TDT)
This technique consists of the oral administration of a triglyceride substrate with labeled carbon (13C) and subsequent assessment of metabolic products (13CO2) in exhaled air. It is a safe and simple method for assessing EPI. Studies comparing DDT with a direct endoscopic secretin test and a 72-hour test with quantitative assessment of fecal fat excretion show a sensitivity of 90–100% and a specificity of 90–92% [51]. An additional advantage is that it can be used to assess response to ERT [34]. TDT has high specificity and sensitivity (> 90%) for CP, prostate cancer, and also after pancreatic resection [52]. In a prospective study by V. Gonzalez-Sanchez et al. conducted a direct comparison of TDT and E-1 for the diagnosis of EPI [53]. The authors concluded that SDT has no additional benefit because the diagnostic accuracy of E-1 and SDT is similar, but E-1 is more readily available in clinical practice and less expensive. In addition, several factors influence the results of TDT: time of CO2 measurement, components of the test food, and physical exercise [54]. The test is suitable for diagnosing fat malabsorption and steatorrhea, but is not able to differentiate pancreatogenic steatorrhea from other forms, since its accuracy may be influenced by intestinal absorption, liver metabolism, diseases of the small intestine, liver and lungs [55]. In addition, the test requires strict compliance by patients with certain conditions, which makes its use difficult.
Secretin-stimulated magnetic resonance cholangiopancreatography
Magnetic resonance cholangiopancreatography with intravenous secretin (s-MRCP) records duodenal filling, ductal secretion, and pancreatic blood flow. The test was developed to study both structural and exocrine changes in the pancreas in patients with chronic pancreatic diseases, in particular CP [56]. The volume of pancreatic secretion is measured by the fluid accumulated in the duodenum within 10 minutes after stimulation with secretin. Secretin stimulation also provides clearer visualization of the main pancreatic duct, its side branches and the duct of Santorini compared with MRCP without secretin stimulation [57], which increases the sensitivity of diagnosing CP from 77 to 89% [58]. To suggest the presence of exocrine pancreatic dysfunction, a T1-weighted MR signal is more specific, which has a sensitivity of 77% and a specificity of 83% [59]. However, this method does not allow to determine a quantitative change in the volume of pancreatic secretion.
Endocrine pancreatic insufficiency
Endocrine pancreatic insufficiency, or pancreatogenic diabetes mellitus (DM3c), is a dysfunction of the islet part of the pancreas. Pancreatic diabetes can lead to significant fluctuations in blood sugar levels, which are poorly controlled by insulin therapy [60]. Patients with T3DM have a higher risk of mortality and hospitalization for complications of DM compared to patients with type 2 diabetes (T2DM) [61]. OG Mark et al. studied genomic associations for the differentiation of T2DM and T3c. The results showed that, in terms of genetic variants, T2DM and T3c are similar, therefore, T3c may be a subtype of T2DM [62]. However, patients with pancreatogenic diabetes have higher HbA1c levels and require earlier initiation of insulin therapy than patients with type 2 diabetes. Due to the more frequent (5-6 times) prescription of insulin therapy, patients with T3c diabetes require more careful monitoring than patients with T2DM. The lack of a diagnostic protocol specifically designed for patients with T3c is a significant gap in clinical practice.
There are several methods for assessing pancreatic islet cell function: fasting blood glucose, serum insulin concentrations, oral and intravenous glucose tolerance tests, and arginine stimulation.
Measuring fasting blood glucose levels
The method is generally accepted for screening diabetes. However, the test is not indicative of quantitative assessment of functioning β cells. In a study by DM Kendall et al. Hemipancreatectomy patients had good glucose tolerance, but fasting blood glucose concentrations were elevated and insulin response to oral glucose was impaired [63].
Oral glucose tolerance test
Measuring blood glucose levels at specified times after glucose ingestion has been widely used in epidemiological studies to assess the adequacy of insulin secretion and determine the presence or absence of diabetes or impaired glucose tolerance [64]. The glucose tolerance test (GTT) is considered the gold standard for diagnosing diabetes [65]. An oral glucose tolerance test with a reduced volume of glucose ingested (50 g) and an hourly follow-up blood glucose measurement is more convenient and accurate than other screening methods (fasting glucose; HbA1c level; glucose tolerance test with 75 g glucose) [66]. However, the use of GTT in patients with CP can lead to exacerbation of the disease.
Intravenous glucose tolerance test
Intravenous administration of glucose leads to a rapid increase in blood glucose concentrations to maximum values after 3-5 minutes, followed by an exponential drop to normal. Blood samples are collected to measure the patient's plasma glucose and insulin concentrations, usually over the next three hours [67]. However, insulin secretion in response to high glucose levels usually varies from a few minutes to half an hour [68]. Due to the labor-intensive nature of the technique, the test is not used in clinical practice.
Acute insulin response to glucose or arginine stimulation
The amount of insulin released in the first 10 minutes after intravenous glucose administration (first phase or AIRgluc) is independent of the pre-stimulation blood glucose concentration, if it is
Glycated hemoglobin
The test is mainly used to screen for impaired glucose tolerance and detect diabetes [71]. Glycated hemoglobin (HbA1c) is formed as a result of a non-enzymatic glycosylation reaction between erythrocyte hemoglobin and blood glucose. Red blood cells circulate in the blood for an average of 120-125 days. This is why the HbA1c level reflects the average glycemic level over approximately 3-4 months. An increase in glycemia significantly accelerates the binding of red blood cells and glucose, which leads to an increase in HbA1c levels in patients with diabetes. The higher the level of glycated hemoglobin, the higher the glycemia over the past three months.
To exclude T1DM, it is necessary to evaluate autoimmune markers, which include autoantibodies to pancreatic islets, autoantibodies to glutamate decarboxylase, insulin, tyrosine phosphatase (IA-2 and IA-2b) and zinc transporter antigen [72].
Serum insulin
Fasting serum insulin concentration provides information about a subject's sensitivity to insulin, but not about the decrease in β-cell number or function. To correctly assess insulin secretion, serum insulin and blood glucose levels must be measured simultaneously. For example, many patients with T2DM have higher fasting serum insulin concentrations than normal individuals, suggesting that they oversecrete insulin. However, at the same blood glucose concentration in healthy people and patients with T2DM, the increase in insulin concentration in healthy people is much higher than in patients with diabetes [73]. The degree of insulin resistance must also be taken into account: in obese patients with normal fasting blood glucose concentrations, fasting serum insulin concentrations are several times higher than in lean patients with similar blood glucose concentrations [74]. A disadvantage of the test is the effect of exogenous insulin on serum insulin levels [75]. In addition, endogenous insulin is extensively (approximately 50%) metabolized on first pass in the liver and peripheral insulin clearance also varies, so peripheral insulin levels may not accurately reflect pancreatic insulin secretion [76].
C-peptide
The physiology of C-peptide makes it suitable for assessing insulin secretion. The peptide is formed as a result of the enzymatic breakdown of proinsulin. C-peptide has negligible hepatic metabolism and constant peripheral clearance. Its half-life is longer than that of insulin (20–30 versus 3–5 minutes) and therefore circulates in concentrations approximately five times higher than insulin [77, 78]. In addition, determination of the level of C-peptide can be used when it is necessary to administer exogenous insulin.
Glucagon
Glucagon −
This is a pancreatic α-cell hormone that promotes the production of glucose in the liver, thereby preventing hypoglycemia. In patients with diabetes, glucagon secretion may be dysregulated, contributing to impaired glucose homeostasis. In T2DM, glucagon levels remain higher in the basal state and increase with increasing glucose load. In T3c, glucagon levels remain low at baseline and do not increase after a glucose load, which distinguishes it from other types of diabetes [79].
Pancreatic peptide
This polypeptide, secreted by the PP cells of the islets of Langerhans in the pancreas, suppresses pancreatic secretion and gastric juice secretion. In addition to low insulin levels and decreased glucagon α secretion —
pancreatic cells in patients with T3c diabetes show lower levels of pancreatic polypeptide [80, 81]. Moreover, in T3c, there is no response of the pancreatic polypeptide to a mixed meal, which is a specific indicator [81, 82]. A decrease in the level of pancreatic polypeptide helps to reduce the sensitivity of the liver to insulin and reduce the production of glucose in the liver. Together, these factors lead to difficult-to-control diabetes with erratic fluctuations in blood glucose levels from hypoglycemia to hyperglycemia [83].
In the regulation of the exocrine function of the pancreas, there is an integral interaction between a number of gastrointestinal hormones, which affect the function of β-cells during the digestion process [84]. The most representative of these are glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP). They are produced in the intestinal wall in response to food intake and are destroyed within a few minutes by the enzyme dipeptidyl peptidase 4. The role of incretins is to regulate the secretion of insulin (stimulation) and glucagon (suppression) when the preprandial glycemic level is exceeded. There have been suggestions about the presence of an enteroinsular axis, demonstrating the relationship between disorders of the exocrine and intrasecretory functions of the pancreas in CP [83]. Unlike T2DM, in which GLP-1 secretion is reduced and there is resistance to the action of GIP [85], in T3c, sensitivity to GLP-1 is preserved, but GIP-induced insulin secretion in the late phase is impaired, as in T2DM [86].
Conclusion
As pancreatic diseases progress, exocrine and endocrine insufficiency develops, which negatively affects the quality of life of patients and its duration. From a practical point of view, this problem has two possible aspects: diagnosis of functional pancreatic failure in the early stages of the disease and timely adequate replacement therapy to prevent metabolic complications.
Insufficient absorption of nutrients due to the presence of EPI, concomitant alcohol consumption, poor adherence to diet and/or drug therapy, accelerated intestinal transit prevent adequate glycemic therapy, which indicates an endocrine-exocrine relationship between pancreatic function and is confirmed by the results of the study by G. Ipsita et al. , where the level of E-1 had a positive correlation with the level of C-peptide and GLP-1 after glucose administration in the general group [79].
Thus, to prevent metabolic complications of functional pancreatic failure, it is necessary to ensure its diagnosis in the early stages.
Considering various methods for diagnosing pancreatic dysfunction, we can come to the conclusion that there is no ideal way to determine the functional activity of the pancreas. Some tests have high sensitivity but are difficult to obtain for clinical use (eg, direct testing of pancreatic function using secretin), while others are widely available but are less sensitive (eg, fecal elastase, serum trypsin) or are expensive. However, E-1 remains stable during intestinal transit [87] and does not require burdensome stool collection or a special high-fat diet.
Information about the characteristics of the course of T3c in pancreatic diseases is still not enough for practicing physicians, which leads to erroneous diagnosis of T1DM or, more often, T2DM. In this regard, it is necessary to carry out several diagnostic tests of carbohydrate metabolism [88].
Future research should focus on developing a rapid diagnostic tool based on understanding potential biomarkers of pancreatic disease to better monitor pancreatic functional failure.
Instrumental methods
Ultrasound examination of the pancreas reveals: - an increase in its size; — change in echo density (swelling, compaction); — presence of echo-dense inclusions; — assess the condition of the Wirsung duct.
This method is used to monitor the course of the disease, as well as to identify complications.
S.I. Polyakova et al. have developed a method for ultrasound examination of the pancreas using a food load, which makes it possible to identify pancreatic pathology with greater accuracy (23%) than traditional examination, as well as conduct ultrasound monitoring of the effectiveness of therapy. A standard ultrasound examination is performed on an empty stomach, repeated 90–120 minutes after a physiological breakfast. Then, based on the level of the “working hyperemia” coefficient of the organ, reactive or chronic pancreatitis is diagnosed [16].
The X-ray method allows us to identify indirect (displacement, deformation of the stomach; duodenal dyskinesia; reversal of the duodenal loop, etc.) and direct signs of pancreatic disease (detection of stones along the pancreatic ducts, calcification of the parenchyma, enlargement of the pancreas).
Currently, combined methods of X-ray examination are increasingly used, including in combination with relaxation probe duodenography.
Endoscopic retrograde cholangiopancreatography
Using this technique, it is possible to detect expansion and deformation of the main pancreatic duct, detect strictures and calcium deposits on the walls of the ducts, and calcification of the pancreatic parenchyma. The study also reveals changes in the biliary system: stenosing papillitis, choledocholithiasis, anomalies in the development of the bile ducts and gallbladder, etc.
Indications for endoscopic retrograde cholangiopancreatography: - recurrent chronic pancreatitis; - blunt abdominal trauma with severe pain; - duodenostasis; - jaundice of unknown etiology; — chronic calculous cholecystitis; — preoperative examination of patients.
Computed tomography and magnetic resonance cholangiopancreatography
The main indications for conducting these studies in children are: - complicated course of acute and chronic pancreatitis; - suspicion of a mass process in the pancreas and adjacent organs.
Functional methods
Assessments of endocrine pancreatic function include: - determination of fasting blood sugar levels; — glucose tolerance test (determining the reserve capacity of the pancreatic insular apparatus).
Thus, to diagnose pancreatic pathology, various instrumental methods, laboratory and functional tests are used, the sensitivity and specificity of which are different (Table 5).
Enzyme deficiency
Pain is one of the symptoms of pancreatic insufficiency
The pancreas performs a number of specific functions, and any one of them can trigger the development of insufficiency. One of the most common pancreatic insufficiencies is enzyme deficiency. Enzymes are found in gastric juice and help food digest. If it happens that at least one enzyme is present in insufficient quantities, the digestion process will be disrupted.
Causes
Among the reasons for the development of enzyme deficiency are:
- Cell damage caused by certain drugs
- Infections
- Damage to the duct
- Pathologies in the structure of the organ (congenital)
- Dysbacteriosis
Symptoms
Among the symptoms that are characteristic of enzyme deficiency are the following:
- Abnormal bowel movements, particularly loose stools
- General weakness
- Appetite disturbance
- Increased gas formation
- Reducing weight and physical activity of a person
- Nausea
- Severe abdominal pain
One of the most important symptoms of enzyme deficiency is a change in stool. This disease is characterized by fatty stools with a very unpleasant and foul odor.
Diagnosis and treatment
In order to make an accurate diagnosis, the patient needs to undergo some tests. These include:
Methods for correcting disorders of the endocrine functions of the pancreas
Currently, there is a large selection of pancreatic enzyme preparations, which provides a real opportunity to help patients with exocrine insufficiency. The priority drugs for the correction of pancreatic insufficiency in children, especially young children, should be microdosed acid-resistant enzymes. Due to the rapid (simultaneous with food) entry of microtablets or microspheres into the duodenum and the release of enzymes from them, as well as the high lipase content in these preparations, they have the most significant therapeutic effect. These enzyme preparations are available in gelatin capsules containing acid-resistant microtablets or microspheres.
The advantages of the microtablet (microsphere) form of pancreatic enzymes are: - uniform distribution in food; — quick and homogeneous mixing with chyme (unlike tablet preparations); — synchronous entry into the small intestine along with the food bolus; — speed of action (at pH > 6.0, 97% of enzymes are released within 30 minutes); — high intestinal bioavailability of the drug (100%).
Preparations containing pancreatic enzymes in the form of microgranules or microtablets can be used either continuously, as replacement therapy, or once, during a food load. The dose is selected individually and depends on the severity of clinical and laboratory parameters of exocrine pancreatic function. The sufficiency of the dose is judged by clinical (normalization of the frequency and character of stool) and laboratory indicators (disappearance of steatorrhea and creatorrhoea in the coprogram, normalization of triglycerides in the stool lipid profile) [12].
Methods
A systematic review and meta-analysis was performed including prospective observational studies or randomized clinical trials. Studies have focused on the use of enzyme replacement therapy for exocrine pancreatic insufficiency after acute pancreatitis in adults.
The diagnosis of pancreatic insufficiency was confirmed by laboratory tests.