Ultrasound examination is one of the most accessible and widespread methods for diagnosing many diseases. It is based on the principle of echolocation, i.e. the ability of tissues to reflect ultrasound rays. The main parameter characterizing the composition and properties of tissues and liquids on ultrasound is echogenicity.
Comprehensive ultrasound of the abdominal cavity - 1000 rubles. Comprehensive pelvic ultrasound - 1000 rubles. Consultation with a doctor based on test results, ultrasound - 500 rubles. (optional) See all prices in the “PRICES” section
MAKE AN APPOINTMENT, TEST OR ULTRASOUND
What is echogenicity
The content of the article
An inverted black and white image is what the sonographer sees during the examination. All human organs reflect ultrasound in their own way. The color depends on the density of the organ: the denser it is, the whiter the picture. For example, liquid is depicted in black. The ability of organ tissue to reflect ultrasound is called echogenicity.
Main ultrasonic parameters
When performing an ultrasound, the doctor evaluates several parameters, the main ones being echogenicity, structure and contours of the organ.
The image on the monitor of an ultrasound machine consists of dots - pixels, each of which is colored in one of 1024 shades of gray. The degree of color intensity will directly depend on the volume of the reflected ultrasound beams. Denser organs reflect waves very well because they absorb environmental vibrations and become intense secondary sources of sound. Therefore, the ultrasound returns to the sensor in almost its original state.
This phenomenon is very similar to the echo in the mountains. So, a strong reflection will color the image light gray or white, and a weak reflection will give a dark gray tint, close to black. Based on the color of the resulting image, the doctor determines the condition of organs and tissues.
Types of tissue echogenicity
There are several types of echogenicity:
- isoechoicity – normal (tissues and organs appear gray on ultrasound);
- hypoechogenicity – reduced (objects of dark color, closer to black);
- hyperechogenicity – increased (pixels are colored white or light gray);
- anechoicity – echonegativity, i.e. lack of echogenicity (black structures).
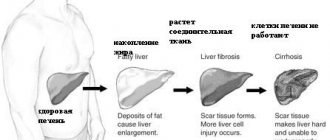
Based on the nature of the color of an organ, a distinction is made between homogeneity (uniform color) and heterogeneity (inhomogeneous coloring of the organ). So, for example, on an ultrasound of the liver, the ultrasound image of a healthy liver will be homogeneous, and the image of a liver affected by cirrhosis will be heterogeneous. That is, color uniformity is an indicator of the normal state of the organ.
The structure of a healthy organ is usually homogeneous. If there are any inclusions or heterogeneity in the structure, the doctor carefully examines these changes. In some cases, a heterogeneous structure is revealed by alternating hypo- and hyperechoic areas, in which a peculiar “motley” pattern is observed.
An important ultrasound parameter is the contours of organs and formations. Normally, the silhouette should be smooth and clear. In the case of an organ, a deviation from the norm may indicate an inflammatory process in it, and with formation - its malignancy. A cancerous tumor will have curved edges, while a benign tumor will have smooth edges.
Normal gland structure
The liver is the largest gland in the human body, with an average weight of 1500 g in adults.
This is a multifunctional organ that takes part in carbohydrate and protein metabolism and neutralization of dangerous compounds.
The gland produces vitamins and hormones.
Liver tissue in a normal state is homogeneous, there are no tubercles or inclusions, the organ is penetrated by many blood vessels and bile ducts.
The echogenic structure is uniform over the entire area of the organ. The color is dark red. The contours are smooth and clear, the edges are sharp.
Hyperechogenicity of tissues - white spots on an ultrasound image
Dense organs and tissues reflect ultrasonic waves at high speed. This means that they are hyperechoic. Increased echogenicity is characteristic of bones, deposits of calcium salts (stones, sand), inflamed tissues, scars or accumulation of fat in tissue.
High echogenicity can also be detected when there is a change in the tissue parenchyma - the main tissue of non-hollow organs. Its hyperechogenicity indicates a decrease in cell saturation with fluid, which occurs as a result of:
- imbalance of hormones in the body (for the mammary, thyroid, prostate glands are detected by ultrasound of the mammary glands, ultrasound of the prostate, ultrasound of the thyroid gland);
- failure of metabolic processes (metabolism);
- improper nutrition (especially for the pancreas - clearly visible on ultrasound of the pancreas);
- smoking, drinking alcohol or using drugs;
- pathological process in the parenchyma;
- inflammatory or traumatic swelling of the tissue.
Prevention
A properly designed menu and a balanced diet help reduce the risk of developing liver pathologies. To maintain the functioning of the digestive system, you should eat only natural foods without dyes or preservatives.
Alcohol and medications pose a particular danger to liver cells.
In addition, it is advisable to regularly clean the organ and arrange fasting days. In folk medicine there are several simple but effective recipes that will help reduce the load on the gland.
What does increased echo density mean: norms and pathology
The concept of “increased echo density” is often encountered on ultrasound. This can be explained this way. Hyperechogenicity of different organs looks different on ultrasound and has a variable meaning:
| Organ | Features of the ultrasound image | What could it indicate? |
Uterus | Diffuse increase in echogenicity, increased organ size | Inflammatory process |
| A hyperechoic round object with sound enhancement is visible | Myoma (fibroma) | |
| Tumor (malignant or benign) | ||
| Blurred contours and heterogeneous echo structure, an echogenic round formation is visible | Endometriosis | |
Endometrium | Uniform thickening of the layer, uniform echogenicity, smooth contours | Hyperplasia |
| Uneven and unclear contours, heterogeneous echo structure | Endometrial cancer | |
Ovaries | An area of increased echo density is visible | Calcium salt deposition |
| Neoplasms of a malignant or benign nature | ||
Pancreas | Hyperdensity of parenchyma | Inflammatory process |
| Swelling | ||
| Increased gas formation | ||
| Malignant tumor | ||
| Increased pressure in the portal vein system | ||
| Stone or calcium deposits in tissue and ducts | ||
| Diffuse increase in echo density, decrease in gland size | Replacement of normal tissue with scar tissue. Occurs as a result of exacerbation of chronic pancreatitis | |
| Diffuse increase in echo density, the size of the gland is not changed | Replacement of normal tissue with adipose tissue. The phenomenon often occurs in diabetes mellitus or old age | |
| High echo density as a transient phenomenon | Poor nutrition (abuse of fatty foods) | |
| General disease – reactive pancreatitis | ||
| Irregular bowel movements | ||
| Wrong lifestyle | ||
Gallbladder | A hyperechoic object is detected | Deposition of stones in the organ |
| Diffuse increase in permeability, thickening of organ walls | Chronic inflammatory process | |
Thyroid | Increased echogenicity of the organ | Endemic goiter (lack of iodine in the body) |
| Toxic goiter (organ damage by poison) | ||
| Autoimmune thyroiditis | ||
| Subacute thyroiditis | ||
| An echogenic formation is visible | Oncology | |
| Areas of sclerosis | ||
Mammary gland | Increased echogenicity of the gland (except for pre-, post- and menopause periods) | Post-inflammatory changes in organ tissues |
| Hyperechoic formations detected | Abnormal cyst | |
| Calcification | ||
| Fibrous area | ||
Kidneys | Hyperechoic structure of the kidneys, their size is increased, the pyramids have reduced echogenicity | Diabetic nephropathy |
| Diffuse increased echogenicity of the parenchyma, organ layers are not differentiated, hypoechoic pyramids | Glomerulonephritis (severe) | |
| Hyperdense area visible | Malignant formation | |
| Myelomas | ||
| Kidney infarction | ||
| Parenchyma calcifications | ||
| Increased echogenicity of the renal sinus | Inflammatory, metabolic or endocrine disorders | |
Spleen | Increased echo density of the organ (excluding age factor) | Increased portal pressure |
| Konovalov-Wilson syndrome | ||
| Glycogenosis | ||
| Amyloidosis | ||
| Increased iron levels in the blood | ||
During pregnancy | Fetal intestinal hyperdensity (after 16 weeks) | Intrauterine TORCH infections |
| Intestinal ischemia | ||
| Cystic fibrosis | ||
| Fetal growth restriction | ||
| Intestinal perforation | ||
| Hyperechogenicity of the placenta | Infarction (hemorrhage) of the placenta | |
| Placental abruption | ||
| Presence of calcifications |
Increased echogenicity can be both normal and pathological, so the diagnosis must be clarified using other examination methods.
Conservative Treatment Options
Therapy for hyperechogenicity is aimed at eliminating or compensating (achieving stable and long-term remission) of the disease. A diet and medications from the group of hepatoprotectors are prescribed, most often based on essential phospholipids (Essentiale Forte, Hepa-Merz).
The drugs eliminate stagnation of bile and accelerate its discharge. For pain in the liver projection area, antispasmodics are taken. For swelling of any localization, diuretic medications are prescribed. Inflammation is reduced with the help of antibiotics. To restore normal blood flow, antiplatelet medications are required.
Treatment is always carried out comprehensively. The patient must strictly adhere to all doctor's orders. Liver diseases are dangerous because they increase the risk of developing cirrhosis and carcinoma (malignant cancer).
Echogenicity below normal - hypoechogenicity - dark gray spot
Hypoechogenicity does not mean a terrible diagnosis, but a structure with a lower density than other tissues. Depending on the organ, reduced echogenicity can be either normal or indicate pathology.
The reduced acoustic density of the formation paints it in dark gray shades. With this phenomenon, the volume of reflected ultrasound is significantly reduced. This is most common with fluid structures such as cysts. The formation may turn out to be not only a cyst, but also an adenosis, fibroadenoma or tumor. The doctor will not be able to accurately determine its nature only by ultrasound results; additional examinations will be required: biopsy, cystoscopy, laparoscopy, bronchoscopy, etc.
Functions of the liver in the body
This body performs the following functions:
neutralizes toxins that are formed when taking medications, alcohol, etc. breaks down and removes from the body excess hormones and toxins formed as a result of metabolism; accumulates vitamins and microelements; participates in the digestion of food through the formation and secretion of bile, synthesizes digestive enzymes and hormones; participates in carbohydrate metabolism: converts amino acids and other substances into glucose, accumulates glycogen, which supplies energy to cells; synthesizes blood proteins responsible for blood clotting, plasma proteins involved in immune reactions, transport proteins for the transfer of enzymes and hormones; deposits blood: with massive blood loss and a sharp drop in pressure, the hepatic vessels narrow, and the accumulated blood enters the circulatory system to maintain the activity of other important organs; synthesis of heme, which transports oxygen.
What does a decrease in echo density mean: table of pathologies
A hypoechoic node can be found in many organs and does not always turn out to be a pathology. Let's take a closer look at what a formation with reduced echogenicity is in various organs, and what preliminary diagnosis can be made.
| Organ | Features of the ultrasound image | What could it indicate? |
Thyroid | Hypoechoic node | Cyst |
| Fluid formation | ||
| Vascular formation | ||
| Oncology (in 5% of cases) | ||
Uterus | Hypoechoic structure with a fuzzy shape, M-echo indicators are increased, the uterine cavity is expanded, heterogeneous endometrial structure | Carcinoma |
| Hypoechoic zone with internal echo structure | Inflammatory process | |
| An area on the wall of an organ with reduced echogenicity | Myoma | |
| Hypoechoic zone near the fertilized egg | Accumulation of blood under the embryo - an incipient miscarriage | |
Mammary gland | A formation that is heterogeneous in structure with reduced echo density, with a fuzzy and uneven contour, gives a shadow | Carcinoma |
| Hypoechoic formation (often irregular in shape) with unclear contours and boundaries | Adenosis | |
| Round hypoechoic inclusion with unclear contours | Typical cyst | |
| Formation with reduced echo density, thickened walls, internal growths and calcifications | Abnormal cyst | |
| Hypoechoic formation with smooth and clear contours | Fibroadenoma (similar to a malignant tumor) | |
Ovaries | Areas with reduced echo density | Follicle |
| Vascular formation | ||
| Corpus luteum | ||
| Cyst | ||
| Oncology (rather rare) | ||
| Heterogeneous structure of the organ during childbearing age and homogeneous during menopause | Normal, not pathological | |
Kidneys | Hypoechoic area with clear boundaries and homogeneous structure | Cyst |
| A formation of heterogeneous structure with reduced echogenicity and unclear contours | Tumor | |
| Hypoechoic formation, retroperitoneal lymph nodes are enlarged, blood flow is not visualized | Oncology | |
Pancreas | Hypoechoic formation with unclear contours, which does not occupy all the tissue of the organ | Metastases |
| A homogeneous formation with low echo density and a smooth contour, without inclusions | Cyst | |
| Several hypoechoic areas | Fibrolipomatous process | |
| Hemorrhagic pancreatitis | ||
| Hypoechoic formation with thin peripheral outgrowths, increased size of the gland, displacement of its large vessels, blood flow is not visualized | Gland cancer | |
Liver | Hypoechoic formations near the portal vein or gallbladder bed, often have a triangular or oval shape | Residual areas of normal tissue against the background of liver steatosis (accumulation of fat in the cells of the organ) |
| Hypoechoic round nodes, possible tuberosity along the periphery | Cirrhosis | |
| Formation with reduced echo density, smooth contours and internal echo signals | Cyst with hemorrhage | |
| Oval, round or elongated inclusion with a loose echostructure | Thrombosis | |
| Areas of varying echogenicity, presence of gas bubbles (not always), uneven contour, echogenic membrane | Abscesses | |
| The hypoechoic zone is round in shape with smooth contours, the presence of echogenic outgrowths extending to the periphery | Nodular hyperplasia | |
| Homogeneous formation with smooth contours, presence of internal signals (not always) | Adenoma | |
| An area with a heterogeneous structure, the presence of areas of hemorrhage and calcifications (not always), changes in local lymph nodes, possible definition of ascites | Liver cancer | |
| Formations with uneven borders and a hypoechoic contour (sometimes), the organ tissue has not changed | Metastases |
For the most accurate and informative study, the patient must properly prepare for the procedure, taking into account exactly how it will be carried out.
Folk remedies
- Tansy has a choleretic effect and has a beneficial effect on organ cells. Recommended for restoring basic liver functions. The decoction is indicated for use in cases of alcoholism, cirrhosis, hepatitis, and in the treatment of infant jaundice . Pour dried flowers (2 tablespoons) into a liter of water and cook over low heat for 25 minutes. Leave the strained broth for 1 hour. Take 1/2 cup three times a day every 6 hours.
- Liver cleansing . Preparation lasts 5 days, for this you need to include only cereals, vegetables and fruits in your diet. After unloading, you need to do an enema. After 2-3 hours, the liver warms up: to do this, apply a hot heating pad to the liver area under the rib. It is advisable to carry out the procedure in the evening before bedtime.
- Herbal cleansing. Pour 1 tablespoon of immortelle flowers and corn silk into a saucepan, pour boiling water (1 cup) and bring to a boil. Infuse the resulting decoction for an hour, strain and drink warm on an empty stomach. An hour after taking the product, warm the liver with a heating pad.
Any traditional medicine can be used only after consultation with your doctor. Otherwise, complications are likely.
© 2022 – 2022, . All rights reserved.
Anechoicity - a black spot on the health map
Areas that are unable to reflect ultrasound waves are called anechoic, or echo-negative. They are displayed on the monitor of the ultrasound machine in black. Liquids also lack echogenicity, so they are depicted in the same way.
Often detected anechoic areas indicate the presence of cystic formations. Small cysts (up to 5 cm in diameter) regress after a few months. Large formations are tolerant to special therapy.
In patients over 50 years of age, such a “finding” during an ultrasound usually indicates a malignant formation. Its untimely treatment is life-threatening. Immediate treatment is necessary for complications of a tumor in the kidneys: pyelonephritis, urolithiasis or arterial hypertension.
Echo-negative formation is a sign of normality. This is the cyclically formed ovarian gland - the corpus luteum. It is impenetrable to ultrasound, so it is displayed on the monitor in a dark color. After menstruation, the formation can be defined as the corpus luteum. If menstruation is delayed, then it indirectly indicates the onset of pregnancy.
Additional Research
Increased echogenicity is an alarming sign. The diagnostic results taken together will help you understand what disease the patient has.
A biochemical blood test is performed. It is used to determine the concentration of sugar, bile pigment, and liver enzymes (ALP, AST, ALT). Tests for markers of hepatitis, HIV infection.
CT or MRI, elastography or elastometry are recommended as instrumental diagnostics if a medical specialist suspects fibrosis.
If a tumor is present, a biopsy is recommended.
What does anechoic formation mean: dangerous symptoms
Table of norms and pathologies when detecting anechoicity::
| Organ | Features of the ultrasound image | What could it indicate? |
Ovaries | Round anechoic formation (or several) up to 2.5 - 3 cm (the rest up to 0.7 - 1.2 cm) | It is not a pathology. These formations are growing follicles |
| An echo-negative round formation more than 3 cm in diameter with a homogeneous structure and surrounded by a thin capsule. Found in the second half of the cycle | Follicular cyst (as a rule, spontaneously disappears in 1 – 3 cycles) | |
| Anechoic inclusion from 3 cm. Formed after ovulation | Corpus luteum cyst (resolves spontaneously after several cycles) | |
| Two-chamber or multi-chamber echo-negative formation with heterogeneous contents, sometimes with various echo-positive inclusions or growths on the walls | Dermoid cyst | |
| Endometrioid cyst | ||
| Cysts that can develop into malignant ones | ||
| Anechoic structure next to the ovary | Luteal cyst | |
Mammary gland | Echo-negative structure (a cavity containing transparent contents) | Cyst |
| Galactocele is a cavity containing breast milk (during lactation) | ||
| Homogeneous anechoic formation | Simple cyst | |
| Anechoic structure with hyperechoic inclusions | Complex cyst | |
| Anechoic formation with uneven contours, various inclusions and deformations | Malignant tumor | |
Thyroid | Echo-negative formation of a round shape with smooth contours and a dorsal enhancement effect | True cyst |
| An anechoic inclusion with a flocculent structure, the walls of which are formed by glandular tissue | Pseudocyst | |
| Anechoic or hyperechoic formation (depending on internal composition) | Adenoma | |
| Avascular inclusion with extremely low density for ultrasound | Colloid cyst | |
Uterus | An echo-negative formation detected during ovulation or 1–2 days after it | Not a pathology. The formation is fluid from a ruptured follicle |
| Anechoic structure in the uterus | Leiomyoma | |
| Degenerative changes in myomatous nodes | ||
| Pregnancy or approaching menstruation | ||
| Echo-negative formation in the suture area | Hematoma formation | |
Cervix | Anechoic formation up to 5 mm | “Normal” occurrence in postpartum women |
| Anechoic formation more than 5 mm | Endocervical cyst | |
| Nabothian cyst (the result of self-healing of ectopia) | ||
| Echo-negative structure with a fine suspension inside or a thickened wall | Endometrial cyst | |
| Thickening and deformation of the organ, several structures with different echogenicity differing in their heterogeneity | Cervical cancer | |
During pregnancy | Anechoic formations are detected in the fetus | Cyst (usually not detected after childbirth) |
| Anechoic formation in the upper third of the uterus with a hyperechoic rim (at 5–6 weeks) | Fertilized egg (pregnancy) | |
| Echo-negative structures | Luteal or follicular cyst (if the inclusions are located in the ovaries) | |
| Paraovarian cysts or serosoceles | ||
Kidneys | Anechoic round inclusion with smooth contours and thin walls | Simple cyst |
| Multiple echo-negative formations in both kidneys | Polycystic | |
| Echo-negative non-round formation with heterogeneous echogenicity, localization - near scar tissue | Secondary cyst | |
| The contours of the kidney are not changed; an anechoic formation is visible near them, next to which there is usually an area of hypoechoic parenchyma | Perirenal hematoma | |
| Echo-negative structure with unclear contours and various inclusions | Cancer | |
| Inclusions of an anechoic nature with unclear contours, vessels are not visualized, the wall of the pelvis is more than 2 mm | Kidney abscesses | |
Liver | Round or oval anechoic formation with partitions (not always), gives a shadow | Simple cyst |
| Echo-negative formations communicating with the branches of the portal vein; the vessels are not visualized | Dilatation of the hepatic vein | |
| Pulsating echo-negative structure communicating with the artery | Hepatic artery aneurysm | |
| Round anechoic formation with echogenic walls and calnates inside | Hydatid cyst |
Thus, an anechoic formation is understood as a cystic, fluid structure. To accurately determine the nature of echo-negative areas, it is necessary to undergo additional examinations.
How does our liver work?
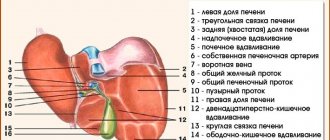
This important organ has 2 surfaces and 2 edges. The upper convex surface is located under the diaphragm. The lower surface contains impressions from nearby organs: colon, duodenum, kidney, adrenal, etc. The liver is divided into 4 lobes: left, right, caudate and quadrate. A healthy liver has a sharp leading edge and a rounded trailing edge. The mass of this organ is 1.6 kg in men and 1.2 kg in women.
Anatomical structure of the liver
The liver is divided into 8 segments by the hepatic veins. A segment is a triangular-shaped section of the liver parenchyma that has its own innervation, blood supply and bile outflow. The caudate lobe is the first segment of the liver, the second and third segments are located in the left lobe, the fourth segment is a quadrate lobe, the fifth, sixth, seventh segments are located in the right lobe, the VIII segment is located on its upper surface.