The structure of the formations, their size and type of contents vary, depending on the location and duration of the onset of the pathological process. They are true (inside lined with epithelial cells) and false (without lining). Based on the type of appearance, neoplasms are divided into:
- retention (usually formed due to a disruption in the process of outflow of secretions in tissues and organs, occurring in the mammary glands, uterus, cervix, ovary, etc.);
- ramolitic (usually found in the ovaries, brain and spinal cord, can form in areas of tissue necrosis, for example after a stroke);
- parasitic (appears in different organs, is the shell of the parasite);
- traumatic (due to bruises);
- dysontogenetic (usually congenital, include different tissues of the embryo);
- tumor (formed due to metabolic disorders, have cavities filled with physiological fluids).
Types of cystic formations
Based on the time of appearance, all cysts are classified into 2 categories:
- Congenital, or dysontogenetic, arise due to disruptions in the process of intrauterine development.
- Acquired ones appear as life progresses.
According to the mechanism of development of cysts, there are:
- Retention - the most common. They are formed if the excretory duct of the gland is compressed or blocked from the inside. The secretion has no outlet, accumulates and stretches the surrounding tissue.
- Ramolitic - arise at the site of dead cells, for example, in the brain after a stroke.
- Parasitic is a capsule within which the parasite is located. In this way, the helminth protects itself from the body’s immune attacks.
- Traumatic ones form at the site of bruises due to the accumulation of tissue fluid.
- Tumor - lined with epithelium with signs of metaplasia; inside there are seals and places where fluid accumulates.
Etiology of retroperitoneal cysts
This type of cyst is considered quite rare and at the initial stage practically does not manifest itself, which determines its danger: as it develops, suppuration develops, pressure on the internal organs and the risk of rupture of the membrane increases. The above poses a real threat to the patient’s health. The initiating factors for the development of cysts in the retroperitoneal space are as follows:
- traumatic injuries to the abdominal area;
- hereditary predisposition;
- congenital anomalies of the abdominal organs;
- parasitic lesions;
- effects of a chemical nature on the peritoneal area;
- hemorrhages and inflammatory processes of internal organs.
Is treatment necessary?
The doctor decides what to do with the identified cyst. It depends on its size, contents, patient complaints:
- Small formations, if they do not bother you, there is no rapid growth and no risk of degeneration into oncology, just observe.
- If the formation is large, causes pain, impairs the functioning of the organ in which it is located, grows quickly, festers or has signs of malignancy, it is removed. After surgery, the tissue is sent to a histology laboratory for examination.
Classic surgery is an open intervention with removal of the cyst using a scalpel. If possible, preference is given to gentle options - using endoscopic techniques, small incisions, and a short rehabilitation period.
The formation is removed using instruments inserted through incisions in the skin, or aspirated with a vacuum device. To avoid relapse, in the latter case it is necessary to cauterize the walls of the cyst. This can be done with a laser, injecting a sclerosant, treating the capsule with radio waves or cold (cryotherapy with liquid nitrogen).
Our doctors
Lutsevich Oleg Emmanuilovich
Chief Surgeon of CELT, Honored Doctor of the Russian Federation, Chief Specialist of the Moscow Department of Health in Endosurgery and Endoscopy, Corresponding Member of the Russian Academy of Sciences, Head of the Department of Faculty Surgery No. 1 of the State Budgetary Educational Institution BPO MGMSU, Doctor of Medical Sciences, Doctor of the Highest Category, Professor
43 years of experience
Make an appointment
Gordeev Sergey Alexandrovich
Surgeon, Candidate of Medical Sciences, doctor of the highest category
42 years of experience
Make an appointment
Prokhorov Yuri Anatolievich
Surgeon, head of the surgical service of CELT, candidate of medical sciences, doctor of the highest category
33 years of experience
Make an appointment
Fedorova Elena Vladimirovna
Surgeon, Candidate of Medical Sciences, doctor of the highest category
22 years of experience
Make an appointment
What types of cysts are there in the human body?
Cystic formations can occur in any human organ. Most often, women develop cysts of the ovary, cervix, Bartholin's gland, and mammary gland. In men, a coccygeal cyst occurs, in patients of both sexes - a cyst of the thyroid gland, brain, paranasal sinuses, and larynx.
Ovarian cyst
The formation may be asymptomatic and is discovered accidentally during a pelvic ultrasound. If the size is large, it stretches the organ capsule and causes pain. A woman may also complain of non-cyclical spotting from the genital tract, disruptions in the menstrual cycle, and inability to become pregnant. In severe cases, torsion of the ovarian cyst pedicle occurs - an acute surgical pathology. It is accompanied by severe pain in the lower abdomen and requires urgent intervention. Otherwise, tissue necrosis may occur and peritonitis may develop.
The treatment is carried out by a gynecologist. He examines the woman, decides whether surgical intervention is necessary and what kind. If the formation has a low oncogenic risk, it is usually removed endoscopically. Sometimes diagnostic laparoscopy with puncture and biopsy of the formation is performed before surgery. If atypical cells are found in it, you may have to perform an oophorectomy (removal of the cyst along with the organ) or adnexectomy (removal of the fallopian tube from the affected side).
Physiological cysts also form in the ovaries, so before removal the patient is observed and ultrasound scans are performed several times, including transvaginally.
Pilonidal cyst
It occurs in men at a young age - up to 30 years. More often this is a congenital formation. A hole is visible in the skin in the area of the sacrum or coccyx. This is an epithelial passage that goes deep into the tissues. Another option is that a cyst forms around the hair, especially during puberty. As long as there is no inflammation in the tissues, there are no symptoms. If microbes get inside, the patient complains of pain, redness, swelling of the skin, and pus is released from the hole.
Conservative treatment can relieve the symptoms of inflammation. Outside of exacerbation, the formation is excised with a scalpel.
Bartholin's gland cyst
It is localized in the thickness of the labia majora. If it is large in size, it can cause pain to a woman while walking, sitting, or intimate relationships. If its contents fester, the pain intensifies, the surrounding skin becomes hot and red.
Sexual infections, poor hygiene in this area, wearing tight underwear, and weakened immunity contribute to the formation of Bartholin gland cysts.
Removal of the cystic formation is carried out using a laser or traditional surgery. After the operation, you may feel dry in the vagina, as the secretion of the Bartholin gland serves as a lubricant for the external female genitalia. If possible, during the intervention, a new excretory duct is formed to allow secretions to come out.
Cysts in the cervix
Nabothian retention cysts are most often diagnosed in the cervical area. They are formed when the mucous secretion has no outlet. This happens due to chronic inflammation, after abortions and other interventions. Sometimes the appearance of a formation is provoked by childbirth, hormonal changes during menopause, or wearing an intrauterine device. Less commonly, endometrioid cysts are detected in the uterus; they fill with blood during menstruation and can be localized in any organ. They are manifested by pain, bloody discharge, which coincides with menstruation.
A Nabothian cyst often occurs without symptoms; a woman may feel pain, discomfort during intimacy, and contact bleeding. Sometimes education is an obstacle to conceiving a child.
A cyst is diagnosed during a gynecological examination and a test is performed with iodine preparations or acetic acid to identify the risk of malignant degeneration. Cervicoscopy, cytology, and biopsy if indicated are performed. Only after all these studies the doctor will determine further treatment tactics.
A surgical removal method or more gentle methods are used: cryodestruction, laser, radio wave exposure, chemical cauterization. If a woman has not given birth and no signs of metaplasia have been detected, doctors try to preserve the cervix as much as possible.
Breast cyst
Cysts form from the ducts of the gland. They are single (solitary) and multiple. The capsule is formed by connective tissue or overgrown epithelium. Fatty cysts are formed from the sebaceous gland if its outlet is clogged with epithelial cells and fat.
The stimulus for the appearance of cavity formations can be injuries, hormonal changes, and stress.
Small cysts do not manifest themselves in any way. With an increase in size, a woman can notice the formation and palpate it. It is necessary to contact a mammologist for further examination. Examination by a specialist, palpation, ultrasound, mammography will help make an accurate diagnosis and select treatment.
Modern methods of treatment are sclerotherapy and laser exposure. A puncture is performed through the skin under ultrasound guidance, the contents are aspirated and sent for cytology. A substance is injected inside to scleros and glue the walls of the cyst, or the capsule is treated with a laser. This method will not be suitable if there are signs of malignant growth, the formation is large (more than 1.5 cm), it is in the stage of purulent inflammation, and has a multi-chamber structure. Then a surgical operation is performed - sectoral resection, that is, they are removed along with part of the mammary gland.
Brain cyst
The formation can be congenital or acquired, located inside the brain or between the meninges. As it increases, it compresses the surrounding tissues, causes headaches, signs of intracranial hypertension appear, and sometimes focal symptoms (impaired vision, sensitivity, motor sphere). Possible dizziness, sensation of pulsation, noise in the head.
Intracerebral cysts form at the site of necrosis during a stroke. Sometimes parasites enter the brain through the blood and become encapsulated. The appearance of cystic formations is facilitated by injuries, inflammation, surgical interventions, and intrauterine development disorders.
Diagnosis is carried out by a neurologist; additionally, CT and MRI of the brain are prescribed. Depending on the diagnosis, treatment is chosen.
Thyroid cyst
An organ in which cysts are often found. They are visible on ultrasound. In suspicious cases (the formation has several chambers, inclusions, epithelial growths), additional tests and a biopsy are performed to exclude oncology. Small asymptomatic cysts are not removed. For large sizes and confirmed malignant growth, surgery is performed.
A cyst in the thyroid gland can manifest itself as pain, difficulty swallowing, and changes in voice. If the walls are formed by glandular tissue, the level of thyroid hormones changes.
Treatment is conservative, gentle surgical (puncture and sclerotherapy or diode laser exposure). If this does not help, the formation reappears, is actively growing, there are atypical cells in the punctate, an operation is performed - half or the entire organ is removed.
Cysts of ENT organs
Laryngeal cysts at the level of the vocal folds are most often caused by large vocal loads. In other sections, they are formed when the excretory ducts of the glands are blocked. The patient may experience changes in voice, sore throat, difficulty breathing, cough, or the presence of a foreign body.
An otolaryngologist examines the larynx and performs a puncture if necessary. They may prescribe an ultrasound, CT scan, or endoscopic examination.
The formation is observed for some time; it may resolve on its own. If it begins to grow, becomes inflamed, or bothers the patient, remove it. Treatment is surgical, often using endoscopic techniques. After the operation, histology is performed.
The cyst is also found in the paranasal sinuses, most often in the maxillary sinus. It may appear due to problems with teeth or developmental features of the nose and sinuses. It manifests itself as pain under the eye, a feeling of fullness, frequent exacerbations of sinusitis with nasal congestion, and discharge along the back wall of the throat. The diagnosis is confirmed by x-ray. The punctate has a yellow color and a thick consistency. After the puncture, anti-inflammatory treatment is carried out. In difficult cases, endoscopic or open surgery is performed.
Symptoms of retroperitoneal cysts
Clinical manifestations of the pathological condition in the form of a cyst are as follows:
- an increase in the size of the abdomen and a change in its shape;
- pain symptoms localized in the abdominal area;
- disturbances in the processes of defecation and urination;
- intestinal obstruction;
- feeling of weakness, lack of appetite;
- nausea and vomiting.
When the nerves of the retroperitoneal space are damaged, the patient experiences severe acute pain localized in the abdomen, lower back, and lower extremities.
Reasons for appearance
A coccyx cyst may not bother the patient at all throughout his life, but still certain prerequisites and factors can trigger its development. It can be:
- weakened immunity;
- injuries to the lower back and in particular to the tailbone;
- low level of physical activity;
- sedentary work that involves sitting in one place;
- infection of the body;
- lack of proper personal hygiene;
- inflammation of the follicles;
- severe hypothermia.
When exposed to unfavorable factors of the external or internal environment, the epithelial coccygeal duct becomes blocked
Sometimes the doctor does not detect any visible reasons for the development of such a cyst. And in some cases it does not begin to grow even with the combined influence of all factors.
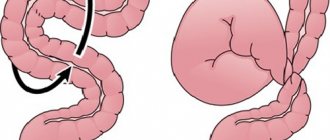
Colon
The large intestine is the next section of the gastrointestinal tract after the small intestine and is divided into the cecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum. The length of the colon is 1.5-2 m, the diameter is 4-6 cm. The wall of the colon is represented by longitudinal muscle fibers, which are concentrated in the form of three ribbons parallel to each other. The width of each of them is about 1 cm. They stretch from the origin of the appendix in the cecum to the initial part of the rectum. The intestine seems to be corrugated, forming protrusions - haustra. The inner (circular) muscle layer is continuous. The mucous membrane of the colon, unlike the small intestine, does not have villi. The submucosa is represented by loose connective tissue containing the bulk of the vessels. The ascending colon in the right hypochondrium forms a hepatic flexure and passes into the transverse colon, the length of which is 50-60 cm. In the left hypochondrium, the intestine forms a left (splenic) flexure and passes into the descending colon. The descending colon becomes the sigmoid colon and then the rectum.
Are there ways to prevent relapses/recurrences of the disease?
Despite the radical nature of the operations, there is always a risk of relapse of the disease. To reduce this risk it is recommended:
- compliance with the rules of personal hygiene and features of postoperative wound care, which will be announced by medical personnel;
- shaving the sacrococcygeal area for 3 months after surgery;
- limiting sitting for 2 weeks and intense physical activity for 2 months after surgery.
- timely visits to the attending physician in the early postoperative period
What operation is performed in case of an abscess (acute suppuration) of the EC?
In the event of an acute ECC abscess developing, in most cases, two sequential operations will be required. Treatment of a purulent focus of ECC should be carried out in a specialized coloproctology hospital. Its main goal is to ensure complete evacuation of purulent contents, stop inflammation in the surrounding soft tissues, and prevent further spread of the purulent process.
Important! Even such a simple step as opening an ECC abscess can significantly complicate the second (main) surgical intervention if simple rules are not followed.
The incision should be small and located as close as possible to the midline (intergluteal fold). During the second operation, the scar from the previous incision will need to be removed en bloc with the main volume of ECC tissue. The larger the primary scar, the more tissue will need to be removed during the second operation. At the same time, you should not make too small an incision, since the key to successful recovery is adequate drainage of the purulent-inflammatory focus (Fig. 8).
a)
b)
Figure 8. Stages of surgical treatment of ECX abscess:
a) local anesthesia
b) an incision above the place of greatest fluctuation and evacuation of purulent discharge with the collection of material to determine the microorganism that caused the inflammation.
Correctly performed opening of an abscess leads to the disappearance of pain, temperature and improvement of well-being. However, the final inflammatory processes (changes in the surrounding tissues) after the first stage of surgery (opening and draining the ECC abscess) usually subside within 1-2 weeks.
After successful completion of the first stage of surgical treatment, which will be accompanied by a decrease in the manifestations of acute inflammation and, in fact, is a “symptomatic operation”, it is no less important to carry out the second stage - a radical operation aimed at complete removal of the pilonidal cyst with the affected area of skin and subcutaneous fat. fiber and the subsequent plastic stage to achieve a good cosmetic result.
Important! In case of acute inflammation, two-stage treatment is the most effective and quickly leads to restoration of ability to work. Despite the improvement in the condition after opening and draining the ECC abscess, it is extremely necessary to perform a second radical operation, since each subsequent inflammation will involve an increasing amount of unchanged tissue in the process!
With a small size of the purulent focus and a high level of professionalism of the surgeon, one-stage radical treatment of acute ECC is sometimes possible.
Long-term inflammatory changes lead to persistent pain and long periods of disability, impaired quality of life, complications and relapses after the second stage of surgical treatment, and complicate radical surgery. It is optimal to perform a second (radical) operation 3-4 weeks after opening and draining the ECC abscess.
What operations are performed for chronic and recurrent forms of ECC?
Currently, there are a large number of different radical operations to remove ECC, each of which has its own advantages and disadvantages.
All types of surgical interventions can be divided into 2 large groups:
- Minimally invasive techniques.
- Radical surgical treatment with suturing of the wound tightly.
Minimally invasive techniques
Minimally invasive techniques include, for example, sinusectomy and laser destruction of the EC. The advantage of these techniques is that after their implementation there is no significant restriction of physical activity; a return to work is possible on the same day after the surgical intervention. The disadvantage is: the possibility of performing it only with small sizes of ECX (the choice of volume and possibility of execution is determined by the doctor after the ultrasound performed).
a) Sinusectomy
If the patient has only primary passages, as well as in the absence of leaks and additional passages or branches, according to additional examination methods, it is possible to perform a minimally invasive operation - sinusectomy. This operation involves a very economical excision of the epithelial tracts using a scalpel, leaving skin bridges between the primary tracts. This allows you to return to work as quickly as possible, obtaining an excellent cosmetic result (Fig. 9).
a)
b)
Figure 9:
a) type of postoperative wound after sinsuectomy
b) appearance of the postoperative scar 3 weeks after sinusectomy
b) Laser ablation of ECX (diode laser)
The essence of the operation is to process the primary passages of the ECX using a laser. This allows you to destroy the ECC passages and prevent the development of complications of this disease. The operation uses a laser with a specific wavelength in continuous mode. During ECC, the laser beam is delivered using an LED (Fig. 10). The laser power can range from 1.5 to 3 W. The total duration of work ranges from 5 to 25 minutes and depends on the stage of the disease and the length of the coccygeal tract. Due to the ability to concentrate its effect only on the affected tissues, the procedure is minimally invasive and is accompanied by minimal pain. In addition, the laser has a coagulating property, thereby minimizing the possibility of bleeding from the affected vessels.
Figure 10. Laser ablation of ECC tracts
Radical surgical excision with suturing of the wound tightly
This operation, perhaps the most common in Russia, involves a more extensive excision of the epithelial sinus/course with plastic surgery of the defect using local tissues. There are many opinions about how effective and safe this operation is. In the hands of an experienced surgeon, as a rule, the probability of relapse with this type of intervention does not exceed 3-5% and is easily tolerated by patients. The main negative aspect of this technology is the need to limit mobility and eliminate sitting after surgery for a period of several days to several weeks.
The type of surgical intervention is finally determined after examination and receipt of ultrasound results of the soft tissues of the sacrococcygeal region and, if necessary, additional examination methods.
How should you prepare for surgery?
The night before hospitalization for surgical treatment, it is necessary to shave the sacrococcygeal and, if necessary, the gluteal region. It is possible to perform laser (Alexandrite or diode laser) or photoepilation a few days before hospitalization. However, the last two methods are ineffective for removing light hair. Another method of hair removal is electrolysis; it is more painful, but is suitable for all hair types. The effect after the procedures may not be achieved immediately, so it is better to perform them in advance - 14 days before the operation. Shaving, as an alternative to hair removal, will take you less time and money, but at the same time it may damage the skin, which can become a source of infection. No other special preparation is required for the operation; it will be enough to refuse food and liquids 8 hours before the operation.