Causes
A number of reasons can provoke the occurrence of the syndrome:
- congenital gastrointestinal diseases;
- pathologies of the mesentery;
- functional disorders of the digestive system;
- presence of foreign bodies;
- accumulation of parasites;
- volvulus;
- inflammatory processes;
- high mobility of the cecum;
- immature peristalsis;
- gallstones;
- strangulated hernias;
- intussusception;
- adhesions;
- formation of fecal stones;
- neoplasms.
Intestinal obstruction causes a buildup of stool and gases. With a long process, toxic substances are absorbed into the blood, resulting in the development of intoxication of the body.
Cystic fibrosis
The disease is caused by a defective gene that controls the body's absorption of salt. As a result, a large amount of salt and little water enters the cells. This causes the fluid that lubricates our internal organs to become thick and sticky. This pathological mucus clogs the lumen of the glands of the digestive tract and blocks the airways.
Attention! The skin of a baby with cystic fibrosis tastes salty.
Most often, symptoms of cystic fibrosis are detected at an early age. In twenty percent of cases, newborns have meconium ileus. The child is not gaining weight well. Sticky mucus can cause serious damage to your baby's lungs. Children often suffer from chest infections. They are worried about shortness of breath and wheezing.
Cystic fibrosis may be the cause of intestinal obstruction in children.
Thick mucus interferes with the normal movement of the food bolus through the intestines and complete digestion. Children experience bloating and abdominal pain. The only thing that specialists can currently do is to alleviate the manifestations of the disease and also slow down its progression.
Antibiotic therapy helps remove thick mucus. Children are prescribed a high-calorie, balanced diet high in protein and pancreatic enzymes. At the same time, the fat content in the diet is sharply limited.
No ads 1
Ascariasis
Roundworms reproduce in the small intestine. While their larvae can move to various organs of our body, for example, to the heart, liver, lungs. The main route of transmission of parasites is fecal-oral. A child can become infected through contact with soil or sand. Infection also occurs when eating unwashed vegetables and fruits.
After entering the intestines, the eggs turn into larvae, which spread through the bloodstream. Ascariasis causes fever, chest pain, and dry cough. Once the larvae are swallowed, they return to the digestive tract. Already there they develop and turn into adults. This process lasts about three months.
During this period, children are worried about the following symptoms:
Causes of bloating and abdominal pain
- weakness;
- nausea;
- irritability;
- stomach ache;
- dyspeptic disorders;
- weight loss;
- bloating;
- the appearance of roundworms in feces;
- stool disorders;
- nausea and vomiting;
- temperature increase.
To confirm the diagnosis, a blood and stool test is prescribed. Drug therapy includes the use of antiparasitic drugs, as well as immunomodulators, antihistamines and restorative drugs. During treatment, foods that provoke the proliferation of pathogens, such as sweets and baked goods, should be excluded from the diet.
Antiparasitic drugs inhibit the movement of roundworms by affecting their muscles. The worm is paralyzed and leaves the body naturally. In order to prevent ascariasis, parents need to thoroughly wash all vegetables and fruits. It is necessary to teach your child not to put dirty hands in his mouth.
Ascariasis can cause ileus in babies
Crohn's disease
The exact causes of this disease are not fully known, although scientists have identified a hereditary predisposition in the mechanism of chronic inflammation. An outbreak can be caused by viruses and bacteria, antibiotic therapy, and increased intestinal permeability.
First of all, attentive parents can pay attention to weight loss and the occurrence of problems with physical development. The disease affects the entire gastrointestinal tract, including the oral cavity. The pathology causes constipation, pain, nausea, and lack of appetite. The goal of the treatment process is to reduce clinical manifestations and achieve stable remission.
Drug therapy includes taking cytostatics and anti-inflammatory drugs. In some cases, the doctor may decide to perform surgery. This may include the formation of fistulas and abscesses, severe stenosis of the intestinal wall, and lack of results from drug therapy.
Signs
Symptoms of intestinal obstruction in children largely depend on the age of the patient, as well as the cause and form of the pathology. Yet, despite the wide variety of causes, the manifestations of the pathology are largely similar. Among them are:
- attacks of abdominal pain;
- nausea and vomiting with impurities of bile and mucus. Vomiting is associated with food intake;
- loss of appetite;
- flatulence;
- paroxysmal bloating, causing pain;
- constipation;
- dehydration.
The acute form is characterized by a sudden onset of symptoms. The chronic process is more characterized by increasing symptoms. In the first case, an urgent operation will be required. In case of chronic obstruction, the baby is placed in pediatric surgery for conservative treatment.
Attention! Ileus can be fatal.
The acute process occurs in three main stages:
- Stage of "ileus cry". Accompanied by severe abdominal pain. Lasts from two to twelve hours.
- Intoxication. The maximum duration is 36 hours. At this stage, the intensity of pain decreases. Abdominal bloating appears, as well as gas and feces retention.
- Terminal. Requires immediate qualified assistance.
In the chronic form, cramping pain in the lower abdomen appears only a few hours after eating. The child is bothered by vomiting and constant constipation. The child's body is exhausted.
Classification
Depending on the time of formation, the pathology can be congenital or acquired. The first option is formed during intrauterine development. Pathology can manifest itself in the form of narrowing of the organ lumen, fusion or inflammatory processes. The acquired form develops against the background of deterioration of peristalsis with subsequent stagnation of chyme.
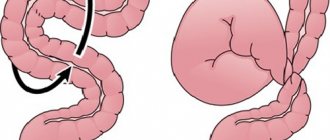
Depending on the pathogenesis (mechanism of formation), the syndrome can be mechanical or dynamic. The first form develops against the background of adhesions, intussusception, surgical interventions, as well as compression by tumors, parasites and foreign bodies. It, in turn, is divided into strangulation and obstruction types.
With obstruction, or blockage, the intestinal lumen is compressed by fecal stones, tumors, etc. Strangulation obstruction develops against the background of circulatory disorders. It can cause peritonitis and necrosis of the intestinal wall. The causes of dynamic obstruction are associated with impaired blood circulation, central nervous system, and water and electrolyte balance. It can be paralytic and spastic.
High obstruction is diagnosed if the affected area is in the small intestine. Low – if the pathological process is localized below the bauhinium valve of the small intestine. Depending on the course of the process, CI can be acute or chronic. In childhood, the first option most often occurs. The syndrome can also be complete or partial. With a partial variant, the tone of the intestinal wall is disrupted. The full version requires immediate treatment and is life-threatening for the child.
The syndrome causes pain and bloating
CONGENITAL INTESTINAL OBSTRUCTION
Congenital intestinal obstruction is one of the most common causes of emergency surgery in children of the neonatal period. Reasons leading to obstruction: 1) malformations of the intestinal tube; 2) disruption of the process, intestinal rotation; 3) malformations of other abdominal organs and retroperitoneal space.
The most common form of malformation of the first group is atresia and stenosis, the occurrence of which is associated with defects in the formation of the lumen of the intestinal tube and impaired blood supply to certain parts of the intestine in the embryonic period. There are 3 types of atresia: in the form of a fibrous cord, membranous form (if there is a hole in the membrane, they speak of stenosis) and complete with separation of the blind ends.
More often, atresia and stenosis are localized in places of complex embryological processes—in the duodenum, the initial section of the jejunum, and the ileum; Sometimes multiple atresias occur. Less commonly, the cause of obstruction is intestinal duplication (duplications, enterogenous cysts), while the obstruction is more often of an obstructive nature. This group also includes disturbances in the formation of nerve ganglia in the intestinal wall, which leads to changes in peristalsis of the affected section and difficulty in the passage of intestinal contents (see Hirschsprung's disease).
The second group of causes of congenital intestinal obstruction includes disruption of intestinal rotation processes in the embryonic period. Delayed rotation at various stages can cause three types of obstruction: 1) volvulus of the so-called midgut, that is, the part of the intestine from the jejunum to the middle of the transverse colon, which has a common blood supply from the superior mesenteric artery; 2) Ladd syndrome - volvulus of the jejunum in combination with compression of the duodenum by peritoneal cords; 3) partial duodenal obstruction due to its compression by cords of the peritoneum and an atypically located cecum.
The cause of intestinal obstruction can also be strangulation of the intestine in internal hernias (for example, in the area of the peritoneal pocket at the duodenojejunal junction - Treitz hernia).
The third group includes malformations of the pancreas: annular gland and congenital cystic fibrosis. In the first case, stenosis of the duodenum develops, caused by compression from the outside; in the second, due to the increased viscosity of meconium, obstruction of the ileum develops.
Atresia and stenosis of the intestine, meconium obstruction cause the symptoms of obstructive obstruction (see Intestinal obstruction). With intestinal volvulus and intestinal strangulation in an internal hernia, symptoms of strangulation are characteristic. Depending on the anatomical variant of the defect, symptoms of intestinal obstruction occur immediately after birth or at a later date.
Congenital intestinal obstruction is divided depending on the level of localization and obstruction into high and low, on the degree of narrowing of the intestinal lumen - into complete and partial, on the time of occurrence - into intrauterine and postnatal.
High obstruction in newborns occurs with duodenal atresia or stenosis, rotation anomaly—Ledd syndrome, midgut volvulus, compression of the intestine by peritoneal cords, annular pancreas, aberrant vessel, and strangulation in a Treitz hernia. High intestinal obstruction appears from the first hours or days of life. Its main symptom is persistent vomiting of stagnant gastric contents mixed with bile. Children lose weight quickly; disturbances in the water-electrolyte balance and acid-base system increase, oliguria occurs, and hematocrit increases. With complete intestinal obstruction that developed in utero, there is no meconium stool.
On examination, the abdomen looks sunken, against the background of which, after feeding, swelling of the epigastric region is clearly visible. Ladd's syndrome and midgut volvulus are characterized by attacks of anxiety in the newborn, which intensify with palpation. When probing the stomach, stagnant contents are obtained in quantities exceeding the norm, usually with pathological impurities (bile, intestinal contents). It should be remembered that when the obstacle is located above the level of the major duodenal papilla (papilla of Vater), the vomit does not contain pathological impurities.
Low intestinal obstruction can be caused by atresia and stenosis of the jejunum, ileum and ascending colon, intestinal duplication, meconium ileus. Low intestinal obstruction also manifests itself from the first hours or days of life and is characterized by significant bloating. Characterized by increased peristalsis, visible to the eye, of dilated intestinal loops (Val's symptom). Vomiting is less frequent than with high obstruction, but the vomit always has a stagnant character, an unpleasant odor, and contains a significant admixture of bile and intestinal contents (the so-called fecal vomiting). Complete intestinal obstruction is also characterized by the absence of meconium passage after birth.
Symptoms of peritoneal irritation are detected, as a rule, in the case of late diagnosis of strangulation types of intestinal obstruction or perforation, when peritonitis develops.
If congenital intestinal obstruction is suspected, the doctor of the parental home should conduct an examination of the patient according to the following scheme: 1) assessment of the medical history (unfavorable course of pregnancy, polyhydramnios is characteristic); 2) assessment of the child’s general condition (detection of intoxication, dehydration - body weight deficiency is greater than physiological loss, high hemoglobin and hematocrit levels, acid-base balance disorders); 3) examination and palpation of the abdomen; 4) probing of the stomach with assessment of the quantity and quality of the contents; 5) rectal examination (with atresia there is no meconium). If the diagnosis of congenital intestinal obstruction is confirmed, the child must be urgently transferred to a specialized surgical hospital, where an X-ray examination is usually performed to determine the level of the obstruction. When performing a survey radiograph in frontal and lateral projections, attention is paid to the degree of filling of the intestines with gas, the number of fluid levels in the expanded parts of the digestive tract. With high obstruction there are two of them - in the stomach and duodenum, with low obstruction there are multiple levels and gas bubbles. The width of the fluid level can be used to judge the anatomical variant of the malformation. With atresia, the fluid level in the stomach is equal to or greater than the diameter of the stomach. With incomplete intestinal rotation, the size of the duodenum is normal, and there is scanty filling of the intestinal loops with gas. If a plain X-ray examination does not provide sufficient information, a contrast examination of the gastrointestinal tract is used. An aqueous suspension of barium sulfate in the amount of one feeding is administered in breast milk.
High intestinal obstruction is characterized by a violation of the evacuation function of the duodenum, therefore, two depots of the contrast agent are visible on the radiograph - in the dilated stomach and the duodenum. If an incomplete intestinal rotation is suspected, the study is supplemented with irrigography with air or barium suspension. Abnormal position of the cecum in the epigastric region or high under the liver confirms the diagnosis. In case of low intestinal obstruction, a contrast study makes it possible to clarify the degree of expansion of the intestinal afferent loops, the localization of fluid levels in them, and the nature of the violation of intestinal passage.
Treatment of congenital intestinal obstruction is only surgical. It is carried out after assessing the risk of anesthesia and surgery, preliminary preoperative preparation aimed at correcting disturbances in homeostasis and the functions of vital organs. The nature of the surgical intervention depends on the malformation: creating continuity of the lumen of the intestinal tube by performing entero-enterostomy, duodeno-, duodenoenterostomy, excision of the membrane. Down-stage operations are possible for low forms of intestinal obstruction, with the first stage involving the application of an intestinal fistula.
In case of incomplete intestinal rotation, the volvulus is straightened and the embryonic cords are separated. With meconium pleus, it is necessary to wash the intestine after opening its lumen with a solution of chymotrypsin, followed by a T-shaped enterostomy and the use of pancreatin in the postoperative period.
The prognosis for timely surgical intervention and the absence of other developmental defects is favorable. The exception is children with multiple developmental defects.
Atresia of the anus can cause low intestinal obstruction if not diagnosed in time. Anal atresia is often combined with rectal atresia or agenesis.
Atresia of the rectum, as a rule, manifests itself in the form of various fistulous forms. In girls, fistulas usually open in the vagina or on the vestibule. In boys, rectoperineal, rectourethral, and rectovesica fistulas occur. Anorectal defects in 30% of cases are combined with malformations of the urinary system.
Actopia of the anus should be distinguished from the fistulous form of rectal atresia, in which the normally formed anal opening is displaced anteriorly along with the external sphincter. The function of the latter is not impaired. However, with significant movement of the anus anteriorly, girls may develop vulvar ginitis, an ascending urinary tract infection.
Treatment of atresia of the anus and rectum is surgical. It is carried out immediately after diagnosis. For fistulous forms of pathology in girls, surgery can be postponed until 1 year from the date of birth.
Intestinal obstruction in newborns
The occurrence of the syndrome in infants is associated either with impaired intestinal motility, or with the presence of some kind of mechanical obstacle. This condition can be fatal to infants.
Causes
The congenital process usually occurs due to abnormal size of the sigmoid colon or stenosis at its border. This condition causes delay and difficult passage of breast milk. As a result, about a week after the start of feeding, heavy regurgitation of undigested milk appears.
There may be other causes of intestinal obstruction:
- increased viscosity of feces. Usually this phenomenon occurs due to an incorrectly selected mixture or the characteristics of mother's milk. This is why during lactation it is extremely important for a woman to monitor her diet;
- a tumor that serves as a mechanical obstacle to the passage of chyme;
- worms and roundworms;
- adhesions;
- volvulus, hernia.
Symptoms
Difficulties in diagnosis are due to the fact that the child cannot describe his complaints. However, parents may be wary of the following signs:
- incessant crying that turns into screaming;
- refusal to feed;
- pulling the legs bent at the knees towards the tummy;
- colic;
- absence of feces for several days;
- lethargy;
- vomit;
- pallor;
- heavy sweating.
The first symptom of intestinal obstruction in newborns is an attack of abdominal pain. The mechanism for the development of this symptom is due to the fact that the intestines are trying to push through feces, but this is impossible due to a mechanical obstruction. Feces begin to accumulate and put pressure on the walls of the organ, thereby causing a painful outbreak.
The pain usually occurs in bursts of about ten minutes. If the pain syndrome has completely gone away, this is not a good sign, indicating the development of life-threatening complications. Another characteristic manifestation of CI is stool retention. If meconium is not passed within a few hours after birth, a pathology may be suspected.
With partial obstruction, thick and hard stool mixed with mucus and blood is observed. Foul-smelling diarrhea indicates the development of a bacterial infection. The accumulation of feces and gases in the intestinal lumen provokes bloating. Visually, you can pay attention to asymmetrical areas. This is due to the fact that the abdomen swells only in those areas where there is no patency.
It is also worth noting another sign of pathology – vomiting. It occurs some time after feeding. Typical regurgitation is “fountain”. Ileus in newborns is divided into four main forms: duodenal, intestinal, ileal, and large intestinal obstruction.
Attentive parents can pay attention to the incessant crying of the baby, which eventually turns into screaming
When diagnosing pathology in infants, treatment should be carried out immediately. The long course of the pathology makes the baby’s condition fatal. If you consult a doctor at the first signs of illness, surgery can be avoided. Now let's talk about the processes that can cause ileus in newborns.
Meconium ileus
Pathology occurs due to excessively dense meconium. Original feces have a fibrous and dense structure, which makes it difficult to pass. The causes of this disorder can be several reasons:
- enlarged lymph node;
- infectious processes;
- cystic fibrosis;
- deficiency of digestive enzymes.
Ileus manifests itself in the form of vomiting and bloating. The main task of the treatment process is to remove dense chyme. A gastric tube is inserted into the baby through the mouth and infusion support is provided. For prevention purposes, antibacterial drugs are prescribed. When pathology is diagnosed early, intestinal lavages are performed. In difficult cases and when conservative therapy is ineffective, surgical intervention is indicated.
Hirschsprung's disease
It manifests itself as a violation of motor function, the cause of which is the absence of nerve cells in the intestinal wall. Because of this, the intestinal section is essentially not involved in the digestion process. Hirschsprung's disease primarily affects boys. Hereditary predisposition plays a major role in the occurrence of the disease. Mutations in genes can trigger the development of the disease.
On the first day of life, pathology manifests itself in the form of a lack of stool. During the first years of a baby’s life, constant constipation, lack of appetite, poor weight gain, distended abdomen, vomiting, and developmental delays are troubling. Treatment involves removing the affected area of the large intestine. The operation is recommended to be performed at an early age. Infants are prescribed conservative therapy, which is a preparatory stage for surgical intervention.
Pyloric stenosis
The pathology is characterized by thickening of the muscle, which is located at the transition of the stomach to the duodenum. Pyloric stenosis becomes an obstacle to the entry of food into the small intestine. Immediately after feeding, the baby vomits the contents of the stomach. It turns out that the baby simply regurgitates everything he eats. Because of this, the child does not gain weight. The only solution to this problem is surgery.
Intussusception
There is an insertion of one segment of the intestine along with blood vessels into the adjacent part. Usually during sleep the baby wakes up from severe pain. The attack lasts about ten seconds. Then the child falls asleep safely, but not for a long time, since after about fifteen minutes the pain attack returns.
Children become pale and sweat excessively. Feces take on the appearance of raspberry jelly, as they contain blood and mucus. If the course is favorable, a special enema of the damaged area is performed under general anesthesia. If there is no improvement, surgery is performed.
Diagnosis of gastric obstruction
The doctor may suspect gastric obstruction during the initial examination of the patient. After collecting anamnesis, the specialist examines the patient, palpates and listens to the abdominal cavity. A violation of the evacuation function of the organ is indicated by asymmetry of the abdomen, whistling noises and splashing during auscultation, and a complete absence of peristalsis.
To find out the cause of gastric obstruction, the doctor prescribes an instrumental examination:
- fibrogastroscopy. A thin flexible tube with a camera at the end is inserted through the mouth. This allows you to visually assess the condition of the gastric mucosa, see neoplasms, ulcers, bleeding, and take tissue samples for histological examination. With pyloric stenosis, the outlet of the stomach is narrowed, the wall of the pyloric region becomes thicker and has a white tint;
- Ultrasound of the stomach. The examination reveals pathology of the pyloric canal, an increase in the thickness of the muscle wall to 0.4 cm or more;
- fluoroscopy with contrast. On X-rays, you can detect an object that has blocked the outlet and assess the degree of narrowing of the lumen. With pyloric stenosis, the stomach is noticeably dilated and pneumatization of the intestinal loops is reduced. A two-hour delay in contrast in the upper tract confirms the diagnosis of pyloric stenosis.