In this article we will look at the pathological syndrome of intestinal obstruction, talk about the causes, symptoms in people and what to do, how to treat this disease for adults and the elderly, and also consider how the disease is classified in the international classification of diseases (ICD 9, ICD 10).
Intestinal obstruction (ileus) is a difficulty in moving digested contents through the intestines. It is provoked by blockage of the intestinal lumen, spasms, disturbances of innervation and blood supply.
If a diagnosis of “intestinal obstruction” is made, symptoms, both in adults and in older people, manifest themselves in the form of severe pain, delayed excretion of feces and gases, and vomiting.
The goal of treating this condition is to restore normal intestinal patency and remove feces from the body.
Features of the condition of intestinal obstruction
Intestinal obstruction, or ileus, is a complex of symptoms rather than an independent nosological entity. Gastroenterologists and coloproctologists say that intestinal obstruction accompanies many pathological processes.
In this condition, the movement of chyme through the small and large intestines is difficult. Intestinal obstruction is a polyetiological condition, that is, it can be caused by a variety of reasons. The forms of the condition are also diverse. H
The earlier the condition is identified, the more gentle treatment measures are applied and the greater the likelihood of successful treatment.
Diagnostics
To diagnose intestinal obstruction, the doctor must know the history of the disease:
- complaints,
- onset of illness
- accompanying illnesses,
- pre-existing conditions
- operations performed.
A physical examination is also important - palpation of the abdomen, rectal examination.
The diagnosis of the disease is confirmed by x-ray examination, which shows the accumulation of gas and liquid intestinal contents over the obstructed area. Urine and blood tests should be performed to assess the degree of dehydration and electrolyte concentrations.
Colonoscopy may be indicated if colonic obstruction is suspected. This is a procedure in which a thin, flexible optical tube is inserted through the rectum into the colon: if the obstruction is caused by intestinal inversion, inserting a colonoscope will invert the intestine and relieve the symptoms of the disease.
Ultrasound of the intestines
Classification of intestinal obstruction
There are several classifications of the condition that take into account clinical mechanisms, pathogenesis and anatomical features. Based on these factors, you can make a correct diagnosis and select the correct methods of therapy that are suitable in a particular case.
Based on morphofunctional reasons, the following types of obstruction are distinguished:
- Dynamic. Its subtypes include paralytic and spastic.
- Mechanical. There are three forms here, these include strangulation (strangulation, torsion, formation of nodes), obstructive (extra- and intraintestinal), and mixed (intussusception, adhesions).
- Vascular. It is provoked by infarction of the intestine.
The level of localization of the obstacle during the movement of digested food determines the division of obstruction into such conditions as:
- high small intestinal obstruction;
- low small bowel obstruction;
- colonic obstruction.
The degree of disturbance in the movement of digested food determines the division of the condition into complete or partial obstruction.
Clinical forms of obstruction are acute, subacute and chronic. There is also a division of the condition into congenital (provoked by developmental defects) and acquired, or secondary.
ICD-10 and ICD-9 code
ICD 10 code:
- K31.5 - Duodenal obstruction;
- K56.0 - Paralytic ileus;
- K56.1 - Intussusception;
- K56.3 - Ileus caused by gallstone;
- K56.7 - Ileus, unspecified;
- P75* - Meconium ileus in cystic fibrosis (E84.1+);
- P76.1 - Transient ileus in the newborn.
ICD 9 code:
- 537.2 - Chronic duodenal obstruction;
- 560.1 - Paralytic intestinal obstruction;
- 560.31 - Gallstone intestinal obstruction;
- 777.1 - Meconium ileus in a fetus or newborn;
- 777.4 - Temporary ileus in a newborn.
Stages of intestinal obstruction
Intestinal obstruction is characterized by a staged course. The stages include:
- Stage of “ileus cry”. Its duration ranges from 2 hours to 14 hours. Symptoms include severe pain.
- Intoxication stage. Lasts from 12 hours to 36 hours. It is based on “imaginary well-being,” which reduces the severity of pain and weakens intestinal peristalsis. Symptoms of intestinal obstruction also appear, such as: delayed excretion of feces and gases, bloating.
- Terminal stage. It occurs 36 hours after the onset of the first symptoms and is manifested by symptoms of circulatory pathology and peritonitis.
Causes of intestinal obstruction
Each form of the condition is provoked by certain reasons. Spastic obstruction is formed when the intestine spasms of a reflex nature. The spasm itself is caused by the following reasons:
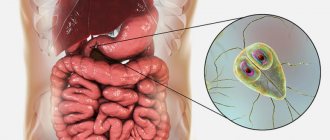
- helminthic infestations;
- foreign objects in the intestines;
- injury to the abdominal area;
- acute form of inflammation of the pancreas;
- biliary colic;
- colic of renal localization, nephrolithiasis, nephroptosis;
- pneumonia, pleurisy, pneumothorax;
- rib fractures;
- acute infarction conditions;
- pathologies of the nervous system (trauma, acute cerebrovascular accidents, dyscirculatory encephalopathy).
Paralytic intestinal obstruction is caused by paralysis and intestinal paresis. They also develop due to conditions such as:
- peritonitis;
- surgical manipulations on the abdominal organs;
- hemoperitoneum;
- intoxication with metal compounds, morphine derivatives;
- food poisoning.
Obstructive, or mechanical, intestinal obstruction is caused by the presence of obstacles along the movement of chyme through the intestinal lumen. Obstacles may include:
- fecal stones;
- bezoars;
- gallstones;
- accumulation of helminthic organisms;
- neoplasms, intestinal cancer;
- foreign object;
- neoplasms of nearby organs (kidneys, reproductive organs and others).
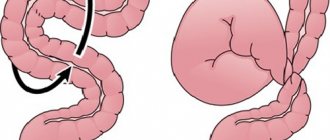
Strangulated intestinal obstruction in adults is provoked by compression of the intestinal lumen and compression of the mesenteric vessels. This condition is observed in the following cases:
- strangulated hernia;
- intestinal volvulus;
- formation of nodes (intestinal loops overlap and twist together);
- intussusception.
Such disorders develop with a large length of the mesentery, the presence of adhesions between intestinal loops, weight loss, fasting and subsequent overeating, and a sharp increase in pressure inside the abdominal cavity.
Vascular intestinal obstruction is provoked by acute blockage of blood vessels caused by thrombotic conditions, embolism of the vascular elements of the mesentery.
Congenital intestinal obstruction is based on anomalies in the formation of the intestinal tube (diverticula, atresia).
What are the types of intestinal obstruction?
There are different classifications of intestinal obstruction:
| Depending on the reason | Mechanical - divided into three types:
Dynamic intestinal obstruction occurs as a result of persistent spasm or paresis (relaxation) of the intestinal wall. |
| Depending on the level |
|
| Depending on the speed of occurrence |
|
| Depending on the degree of intestinal obstruction |
|
According to statistics, if timely medical care is not provided, with acute intestinal obstruction, up to 90% of patients die within 4–6 hours. Therefore, it is important for the patient to know the first symptoms of this condition and, if they occur, to immediately consult a doctor. [2,5,8]
Symptoms of intestinal obstruction
Common manifestations characteristic of all variants of the condition are severe pain, delayed passage of gases and feces, as well as vomiting. Abdominal pain syndrome is characterized by an unbearable, cramping course.
The painful contraction coincides with a wave of peristalsis, the patient may groan, the facial expression changes, the person is forced to take specific poses in order to soften the attack. At the peak of an attack of pain, shock symptoms appear, which include:
- pale skin;
- formation of cold sweat;
- decreased blood pressure;
- increase in heart rate.
The subsidence of pain is often a bad sign: it may indicate necrotic changes in the intestinal tissue. The second day after the onset of symptoms, peritonitis develops.
Vomiting is also a symptom that is most characteristic of ileus. When areas of the small intestine are involved in the process, repeated vomiting is observed, quite profusely.
After vomiting, the patient does not feel better. At the initial stage, vomiting includes food debris, after that - bile, and in the very late period - intestinal contents. Late vomiting is also called fecal vomiting and has a putrid odor. In case of colonic obstruction, a vomiting attack can be repeated 1-2 times.
Delayed fecal excretion and flatulation are typical manifestations of intestinal obstruction. A rectal examination reveals the absence of contents in the rectum, while its ampulla is stretched and the sphincter is gaping. In a situation of high small-intestinal obstruction, a delay in fecal excretion may not be observed: the intestines empty either independently or as a result of an enema.
Also, with intestinal obstruction, it is possible to observe symptoms such as asymmetry of the abdomen, bloating, and visually noticeable peristaltic movements.
Symptoms
The main symptom of intestinal obstruction is abdominal pain. They appear suddenly, for no apparent reason, and are cramp-like in nature. Painful sensations periodically subside and appear, intensify again, in accordance with the waves of peristalsis - physiological movements of the intestine. After some time, the pain may become constant.
With strangulation intestinal obstruction, the pain is constant, periodically intensifying during peristaltic waves. If the pain suddenly goes away, this is a bad sign; it indicates that movements in the intestinal wall have stopped and paresis (paralysis) has developed.
With paralytic intestinal obstruction, dull, bursting pain is most often bothered. [10,11]
Other possible symptoms: [2]
- Constipation: abdominal pain is accompanied by the absence of stool for several hours, and gas does not pass. If the obstruction is severe, the patient may pass stool due to the passage of the contents of a portion of the intestine that is located below the obstruction.
- Nausea and vomiting, which increases over time, can become uncontrollable. Vomiting does not bring relief. At first, it occurs reflexively; the vomit contains stomach contents and bile. Then, with some types of intestinal obstruction, it becomes fecaloid.
- Some patients with partial intestinal obstruction experience diarrhea.
- Loss of appetite.
- Blood in the stool.
- Bloating. It becomes asymmetrical, and intestinal movements—peristalsis—are noticeable. Gradually these movements disappear, which indicates that intestinal paresis has developed.
- Deterioration of the patient's general well-being.
- Dry mouth.
- Apathy, depression of consciousness.
Diagnostic measures for intestinal obstruction
To diagnose obstruction, the following measures are taken:
- Percussion of the abdomen. This is characterized by a tympanic sound with metallic tones, or Kivul’s symptom. Percussion sound is dull.
- Auscultation of the abdomen. At an early stage - excessive peristalsis and “splashing noise”, at a late stage - “noise of a falling drop”, weak peristalsis.
- Palpation of the abdomen. The doctor determines the distension of the intestinal loops, or Val's sign, and at a later date, rigidity of the abdominal wall appears.
- Rectal and vaginal examination. They help determine blockage of the rectum, as well as identify a tumor process in the pelvic area.
- Survey radiography. The technique allows you to identify intestinal arches, Kloiber cups and symptoms of pinnateness.
- X-ray examination using contrast is prescribed in cases where diagnosis is difficult by other means.
- Colonoscopy. Sometimes this method is not only diagnostic, but also therapeutic, that is, it helps resolve intestinal obstruction.
- Ultrasound examination of the abdominal cavity. This technique is hampered by intestinal pneumatization, but it makes it possible to identify tumor and inflammatory infiltrative processes.
Differential diagnosis in case of intestinal obstruction consists in identifying the difference between the pathology and conditions such as:
- acute appendicitis;
- stomach or intestinal ulcer with perforation;
- acute form of cholecystitis;
- acute form of pancreatitis;
- renal colic;
- pregnancy with ectopic localization.
An experienced specialist will carry out all the necessary diagnostic procedures and prescribe the correct treatment to relieve the symptoms of intestinal obstruction.
Course of the disease
First of all, peristalsis is disrupted, which leads to severe irritation of the receptors in the intestinal wall and severe pain. Due to the lack of nerve impulses or due to compression of the intestines, inflammation of the intestinal wall begins, the tissues die and are gradually destroyed. The intestines can then perforate and cause inflammation of the peritoneum, the membrane of connective tissue lining the abdominal cavity.
When the intestines are pinched, chyme accumulates, the intestines dilate, and antiperistaltic bowel movements (vomiting) begin.
Ascites (bloating) occurs due to the accumulation of fluid in the abdominal cavity.
Finally, in prolonged chyme, the processes of fermentation and putrefaction begin, poisoning the entire body.
Symptoms of the disease appear quickly - in the first few hours, only in the case of colorectal cancer or diverticulosis, symptoms may appear later. For these reasons, the patient may not seek help for weeks or months.
Therapeutic correction of intestinal obstruction
In case of intestinal obstruction, the patient should be immediately hospitalized in a surgical inpatient department. Before a medical examination, it is prohibited to give enemas, give the patient analgesics, laxatives, or wash the stomach.
If there is no peritonitis, then in stationary conditions decompression of the digestive tract is carried out using aspiration of the contents of the digestive system through a thin nasogastric tube, as well as a siphon enema.
In case of pronounced peristaltic movements and cramping pain syndrome, antispasmodics (platiphylline, drotaverine) are administered. In case of paresis, drugs are administered that stimulate intestinal motility (proserin), and a perinephric blockade is also performed using novocaine. To correct the imbalance of water and electrolytes, saline solutions are administered intravenously.
If the listed measures do not bring a visible positive result, a conclusion is made about the mechanical nature of the ileus, after which urgent surgical intervention is performed.
During the operation, mechanical obstruction is eliminated, the affected area of the intestine is resected, and measures are taken to prevent recurrent cases of intestinal obstruction.
If intestinal obstruction is caused by a tumor process in the area of the large intestine, then the operation involves a hemicolonectomy, as well as a colostomy. In case of inoperable tumor, surgeons perform a bypass anastomosis. For peritonitis, transversostomy is performed.
After surgery, the following measures are necessary:
- restoration of circulating blood volume,
- detoxification,
- administration of antibiotics,
- restoration of the balance of proteins, water and electrolytes.
Treatment of intestinal obstruction in cancer patients
In some cases, in the absence of signs of peritonitis, intestinal obstruction can be combated with conservative measures within 24 hours. The stomach is lavaged through a tube, the patient is given solutions of proteins and electrolytes, the body is saturated with fluid to combat dehydration, and painkillers and antibacterial drugs are prescribed. If conservative treatment does not help, surgical intervention is performed as planned.
If upon admission to the clinic the diagnosis is immediately confirmed and/or there are pronounced symptoms of peritonitis, emergency surgery is indicated. [1.15]
There are different surgical treatment options: [2,7]
- In some patients, the cause of intestinal obstruction can be eliminated. The affected area of the intestine is removed, capturing a certain amount of healthy tissue above and below, adhesions are dissected, volvulus, nodes, and intussusception are eliminated. After the affected area of the intestine is removed, the remaining ends are connected. If the diameter of the remaining ends is approximately the same, an end-to-end anastomosis is performed; if it differs greatly, an end-to-side anastomosis is performed.
- If the cause of intestinal obstruction cannot be eliminated, a stoma is performed - a section of the intestine is sutured to the surface of the skin and an opening is created for the passage of feces. The name of the operation depends on which part of the intestine is sutured to the skin: Ileum - ileostomy .
- Cecum - cecostomy .
- Colon - colostomy (ascending colon - ascendostomy , transverse colon - transversostomy , descending colon - descendostomy ).
Sometimes, after some time, after the patient’s condition has stabilized, it is possible to perform a second operation to eliminate the cause of intestinal obstruction and close the stoma. In other cases, the stoma will be permanent.
Often, surgical interventions for intestinal obstruction are palliative . Their purpose is to ensure free passage of food through the intestines. Due to this, the patient's life expectancy increases. [7,8]
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Clinical recommendations: Acute intestinal obstruction of tumor etiology. - Moscow, 2014.
- Clinical recommendations: Acute intestinal obstruction of tumor etiology in adults. — Ministry of Health of the Russian Federation. — 2022.
- B. O. Kabeshev, S. L. Zyblev. Acute intestinal obstruction. — A practical guide for doctors. — Gomel, 2022.
- Tracy Jaffe, William M. Thompson. Large-Bowel Obstruction in the Adult: Classic Radiographic and CT Findings, Etiology, and Mimics. Radiology: Volume 275: Number 3—June 2015.
- Canaan Baer, Raman Menon. Emergency Presentations of Colorectal Cancer. Surg Clin N Am 97 (2017) 529–545. https://dx.doi.org/10.1016/j.suc.2017.01.004
- Methodological development for the practical lesson “Acute intestinal obstruction” Ed. USMA, Yekaterinburg, 2011 - 25 p.
- M.Yu. Kabanov, I.A. Solovyov, O.V. Balura. — Results of complex treatment of patients with acute intestinal obstruction of carcinomatous origin. - Bulletin of the Russian Military Medical Academy, 1(37)-2012.
- Barnett A, Cedar A, Siddiqui F, et al. Colorectal cancer emergencies. J Gastrointest Cancer 2013;44(2):132–42.
- Chalieopanyarwong V, Boonpipattanapong T, Prechawittayakul P, et al. Endoscopic obstruction is associated with higher risk of acute events requiring emergency surgery in colorectal cancer patients. World J Emerg Surg 2013;8:34.
- A.V. Pugaev, E.E. Achkasov, M.G. Negrebov. — Intussusception intestinal obstruction in adults. - Surgery, 5 - 2022. https://doi.org/10.17116/hirurgia2018540-44
- National clinical guidelines “Acute non-tumor intestinal obstruction”. — Russian Society of Surgeons. — 2015.
- Abdukarimova M.K. — X-ray diagnosis of intestinal obstruction. — Bulletin of AGIUV. — 2008, No. 5(8).
- Patrick Jackson, and Mariana Vigiola Cruz. — Intestinal Obstruction: Evaluation and Management, Am Fam Physician. 2022 Sep 15;98(6):362-367.
- Bertrand Trilling, Edouard Girard. — Intestinal obstruction, an overview — Rev Infirm. 2016 Jan;(217):16-8. doi: 10.1016/j.revinf.2015.10.028.
- Thévy Hor, François Paye. — Diagnosis and treatment of an intestinal obstruction. — Rev Infirm. 2016 Jan;(217):19-21. doi: 10.1016/j.revinf.2015.10.030.
Prevention
Preventive measures regarding intestinal obstruction include timely detection and removal of tumor formations, preventing the development of adhesions, and getting rid of helminthic pathologies. It is equally important to eat right and avoid injury.
If you notice symptoms of intestinal obstruction, you should immediately contact a specialist. Timely diagnosis is the key to correctly prescribed therapeutic measures and their effectiveness, that is, the patient’s recovery.