Pyloric stenosis (high gastrointestinal obstruction)
The main threat is the complete impossibility of food passing from the stomach to the underlying sections of the gastrointestinal tract and the development of exhaustion.
- Development mechanism
Post-ulcer cicatricial stenosis of the pylorus (pyloric stenosis) or duodenum is a complication of peptic ulcer of the gastric outlet (pylorus) or duodenal bulb. A scar forms at the site of a healed ulcer, the tissue in the scar area tightens, and the passage of food from the stomach to the duodenum becomes difficult. This place is constantly injured by food masses and is affected by hydrochloric acid. Chronic inflammation occurs, the narrowing zone progresses, and the passage becomes even narrower. Then decompensation develops: food passes with great difficulty, the stomach expands and loses its peristaltic function. In patients with signs of decompensated duodenal obstruction, the stomach can reach enormous sizes, food stops passing further into the intestine, and the digestion process stops. Exhaustion sets in.
- Symptoms
The ulcer manifests itself as pain in the abdominal cavity. This could be hunger pain or pain after eating. The narrowing of the gastric outlet manifests itself as nausea and a feeling of fullness after eating. Normally, a person should wake up in the morning feeling hungry, but a patient with high obstruction wakes up with a feeling of fullness in the stomach. Decompensation of stenosis is characterized by vomiting of food eaten 2-3 hours before. Decompensation is a life-threatening condition and you should consult a doctor immediately.
- Diagnostics
In order to diagnose post-ulcer cicatricial stenosis of the gastric outlet, computed tomography with water-soluble contrast and X-ray examination with water-soluble contrast or with barium are used. To understand how long it takes for a patient to evacuate the stomach contents to the underlying sections of the gastrointestinal tract, the doctor gives the patient barium, takes an x-ray, and sees where the barium has spread. Then pictures are taken after 3, 6, 12 hours - this allows you to evaluate the dynamics of contrast passage and the degree of stenosis. At the Ilyinskaya Hospital, patients with suspected high intestinal obstruction always undergo endoscopic diagnosis: using an endoscope, the doctor accurately localizes the site of the stricture and determines the scope of surgical care.
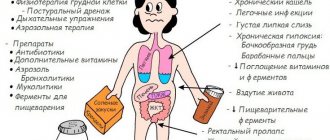
Pyloric stenosis
Image source: Designua / Shutterstock
- Balloon dilatation of the scar stricture area
If the patient applied to the Ilyinsky hospital at an early stage of the disease and was diagnosed with compensated cicatricial ulcerative stenosis of the gastric outlet, then the patient can be offered an endoscopic treatment method - balloon dilatation of the scar stricture area. A thin endoscope is passed through the mouth into the narrowing area. Under the simultaneous control of an endoscope and x-ray, a special balloon is delivered through the instrumental channel of the endoscope to the narrowing area. The balloon is inflated, the area of stenosis is stretched, and the obstruction is resolved. The pressure in the balloon is controlled by a pressure gauge, which eliminates damage and rupture of stomach tissue. X-ray endoscopically assisted balloon dilatation of the area of scar-ulcerative narrowing of the gastric outlet or duodenal bulb is a delicate but effective operation.
- Laparoscopic pyloroplasty
If the degree of gastrointestinal obstruction does not allow balloon dilatation, but there is no serious form of decompensation yet, surgeons at the Ilyinskaya Hospital perform laparoscopic surgery on the patient - pyloroplasty. Through small incisions on the abdominal wall (about 10 mm in size), a laparoscope and surgical manipulators are inserted into the abdominal cavity. At the same time, an endoscope is inserted through the mouth into the lumen of the stomach. Using laparoscopic instruments, the surgeon dissects the narrowed area of the duodenum and the outlet of the stomach in the longitudinal direction and stitches it in the transverse direction, thereby significantly expanding the narrowing site and resolving the obstruction. The second surgeon assists him from the lumen of the stomach using an endoscope, ensuring maximum safety of the manipulations. This is a low-traumatic operation that gives a lasting positive effect.
- Laparoscopic subtotal gastrectomy
If the patient is diagnosed with a severe decompensated stage of gastrointestinal obstruction, then the above operations are not effective. In this case, surgeons at the Ilyinsk Hospital perform laparoscopic subtotal gastrectomy. The patient's stomach is greatly enlarged, its peristalsis is impaired, and food accumulates in the stomach. Therefore, the surgeon needs to resect most of this stretched and loss of function stomach. The operation is performed laparoscopically through four small incisions. The remaining part of the stomach is connected to a loop of jejunum - an anastomosis is formed. The next day after such an operation, the patient can already drink water. Every other day, he undergoes an X-ray examination with water-soluble contrast to monitor the integrity of the anastomosis. If everything is in order, then the patient is immediately allowed to eat liquid food.
Symptoms of acute and chronic duodenitis
If we talk about the disease as a whole, the inflammatory process usually proceeds sluggishly, manifesting itself as disturbances in appetite and general well-being and some dyspeptic symptoms (for example, rumbling in the stomach, flatulence). Patients often seem to be self-absorbed and irritated. Children are usually “skinny” and grow poorly. But the clinical picture of duodenitis can develop quite rapidly, especially with concomitant infection with Giardia.
Acute duodenitis. Suddenly and, as a rule, after a heavy overeat, an attack of severe abdominal pain may occur, from which patients literally writhe. The pain is not relieved by any medications. The patient's face becomes covered with beads of sweat. Repeated vomiting may initially suggest acute pancreatitis, but a dry and white-coated tongue clearly indicates peritoneal irritation, leukocytosis and low-grade fever. All these symptoms leave doctors no choice: the only way out is surgical intervention. So, sometimes an accurate diagnosis is made on the operating table - acute duodenitis.
Symptoms of acute duodenitis also include pain and a feeling of fullness in the stomach area (the so-called epigastric region), excessive salivation, nausea and vomiting, and loss of appetite. Body temperature often rises. The attack may be accompanied by headaches, weakness and arterial hypotension.
Chronic duodenitis. This course of the disease is characterized by a variety of clinical manifestations, which make it difficult to make a diagnosis: chronic duodenitis is often mistaken for other diseases of the digestive system. So, most often it “simulates” a duodenal ulcer, but with less pain and less severe seasonal exacerbations. When disturbances in the normal functioning of the stomach (dyspeptic disorders) come to the fore, the disease is initially misdiagnosed as gastritis.
There are forms of this “many-faced” disease that manifest themselves as chronic cholecystitis or pancreatitis: pain occurs in the right hypochondrium or girdle pain in the upper abdomen, which certainly intensifies after eating fatty foods.
In young women, the neurovegetative form of duodenitis is more common. Autonomic disorders usually predominate here: increased fatigue or, on the contrary, excitability; weakness, headaches, etc. With mixed manifestations of chronic duodenitis, symptoms of a variety of clinical forms are combined. But often, especially in older people, the disease occurs in a latent form, that is, asymptomatic.
Separately, it should be said about phlegmonous duodenitis . It is rare, but, as they say, it “hits straight.” This is an acute purulent inflammation that affects the wall of the duodenum. It can occur as a primary factor due to the penetration of harmful microbes (staphylococci, streptococci, etc.) through the mucous membrane into the deep layers of the intestinal wall (this occurs with deep ulcers, disintegrating tumors and mechanical damage to the mucous membrane). Secondary phlegmonous duodenitis usually develops as a result of the spread of pathogenic microorganisms from any primary foci (for example, with furunculosis or abscesses of various locations).
Diagnosis of duodenal diseases
The main methods used in the diagnosis of duodenitis are as follows:
- Gastroduodenoscopy is the most informative method that helps to determine or exclude the disease. This endoscopic procedure determines whether there are inflammatory processes on the mucous membrane, whether erosions, duodenal ulcers, or duodeno-gastric reflux have developed. The study is carried out on an empty stomach with possible preliminary sedation of the patient.
- Examination of biopsy material or a urease breath test helps determine the presence of Helicobacter infection.
- X-ray examinations (performed less frequently).
When contacting a clinic for diagnostics, you must remember that most of the proposed procedures are performed on an empty stomach. A preliminary consultation with a gastroenterologist will allow you to properly prepare for the tests, which will significantly increase their information content.
Introduction
Postbulbar duodenal ulcers (DU) in diagnostic and tactical and technical terms are classified as “difficult” duodenal ulcers. According to the literature, they occur in 0.9-25% of the total number of cases of duodenal ulcer [1, 3, 7, 10, 12, 15].
According to the clinical course, postbulbar ulcers differ from duodenal ulcers of usual localization in their “aggression”, higher rates of acid production in the stomach, resistance to antiulcer therapy, high incidence of complications, especially penetration of ulcers into neighboring organs, and acute bleeding. Penetration of postbulbar ulcers, according to the literature, ranges from 25.3 to 90% and creates significant technical difficulties when performing surgical interventions [7, 9, 10].
The incidence of duodenal stenosis in postbulbar ulcers ranges from 45.1 to 65.5% [7, 10, 15].
In the surgical treatment of postbulbar ulcers and stenoses, many surgeons prefer gastric resection, including “turning off” the ulcer. The results of this operation cannot be considered satisfactory due to high mortality and a significant number of complications. The main cause of death is failure of the sutures of the duodenal stump, which is most often observed in patients operated on for so-called difficult ulcers [9, 12].
A number of surgeons for postbulbar stenosis consider selective proximal vagotomy (SPV) with duodenoplasty as an alternative to gastric resection, which preserves the anatomical and functional integrity of the pyloric sphincter [5, 13, 16].
Time has shown that gastrectomy for postbulbar stenosis cannot remain an alternative in the arsenal of surgical interventions due to the high incidence of postoperative complications and mortality. However, one cannot categorically speak out against gastric resection, including “switching off” the ulcer, as a method of surgical treatment of complicated duodenal ulcers, since the surgical situation sometimes dictates its own conditions.
Material and methods
Our conclusions are based on long-term observations of 214 patients who routinely underwent various surgical interventions for postbulbar duodenostenosis. Among them, there were 169 men (78.9%), women - 45 (21.1%), their ratio was 3.8:1. The age of patients varies from 16 to 66 years.
In the phase of exacerbation of peptic ulcer disease, 182 (85.1%) patients were admitted. Cicatricial stenosis was diagnosed in 85 (39.7%) patients, cicatricial ulcerative stenosis was diagnosed in 129 (60.3%) patients. Penetration of the ulcer into neighboring organs or formations was present in 184 (85.9%) patients, including 85 (68.5%) with periulcerous inflammatory infiltrate.
Duodenostenosis in the compensation stage was diagnosed in 24 (11.2%) patients, in the subcompensation stage - in 75 (35.1%), decompensation - in 115 (59.7%) patients.
In order to diagnose postbulbar stenoses, we used all the methods used to diagnose duodenal ulcer. Radiologically, it is sometimes difficult to establish the localization of stenosis due to a pronounced violation of the evacuation function of the stomach. Radiological diagnosis of postbulbar stenosis was established in only a third (33.8%) of patients. During gastroduodenoscopy, due to anatomical disorders in the pyloroduodenal zone, overdiagnosis of postbulbar stenosis is often observed, therefore the main way to accurately diagnose the localization of postbulbar stenoses remains intraoperative revision after mobilization of the duodenum according to Kocher.
Results and discussion
When performing an operation, the correct tactics of the surgeon for each specific patient with postbulbar stenosis of the duodenum is important. The nature of surgical interventions for postbulbar duodenostenosis is presented in the table.
The desire to necessarily perform radical surgery to remove the ulcer, which is recommended by a number of surgeons, is not justified [2, 5, 6, 8]. This tactic leads to irreparable intraoperative and postoperative complications: damage to the elements of the hepatoduodenal ligament, postoperative pancreatitis, failure of the sutures of the duodenal stump, etc. To avoid these complications, it is necessary in each specific observation, taking into account the nature and prevalence of the pathological process, to choose individual tactics and perform adequate surgical intervention.
Radical removal of a stenosing ulcer is indicated only in the absence of periulcerous inflammation and penetration, i.e. with cicatricial stenosis. However, such radicalization is not always justified, as it is associated with the risk of damage to the hepaticocholedochus, pancreas, and opening of the duodenal lumen. Often, a “difficult” duodenal stump is artificially created, the treatment of which is carried out in conditions of intestinal tissue deficiency. The latter always occurs and is most pronounced in penetrating duodenal ulcers.
Gastric resection with radical excision of the ulcer was used in 63 (29.4%) cases, including 6 in combination with selective vagotomy. In 39 cases, it was completed with the formation of gastroenteroanastomosis according to Hoffmeister-Finsterer, in 23 - according to Roux, in 1 - according to Balfour. However, if there was a real danger of damage to the elements of the hepatoduodenal ligament or the formation of a “difficult” duodenal stump due to an extensive cicatricial adhesive process or periulcerous inflammatory infiltrate, we refused such an intervention in favor of gastric resection “on switch” or PPV with drainage or duodenoplastic operations.
A retrospective analysis showed that during gastric resection with radical excision of the ulcer, technical difficulties in isolating and suturing the duodenal stump were observed in almost every second (32) patient. In 17 (24.6%) cases, cutting of sutures and opening of the intestinal lumen were noted, which forced to resort to “open” treatment of the duodenal stump. In the early postoperative period, failure of the sutures of the duodenal stump was observed in 3 (4.3%) patients who underwent radical excision of a postbulbar ulcer.
For stenosing postbulbar ulcers penetrating into adjacent organs with periulcerous inflammatory infiltrate, in 39 (18.2%) cases, gastric resection was used to “turn off” the ulcer, of which in 8 in combination with selective vagotomy. Gastrojejunostomy according to Roux was used in 14 of them, according to Hoffmeister-Finsterer - in 25 cases.
When performing gastric resection to “turn off” an ulcer, some authors give preference to the subpyloric option [11], which, in our opinion, is less reliable and creates technical difficulties when suturing the duodenal stump, since it has to be formed in conditions of tissue deficiency and inflammatory changes. The latter always occur and are more pronounced in penetrating ulcers of the duodenum.
When performing the suprapyloric variant of gastrectomy to exclude an ulcer, we, like other authors, highlight a number of mandatory stages of the operation. Among them, the most important are demucosation, maintaining good nutrition of the remaining part of the vestibule, careful hemostasis during the formation of the seromuscular cuff, and maintaining asepsis.
All these requirements are met to a greater extent by the improved G.P. Rychagov [14] a method of covering the duodenal stump during gastric resection to exclude an ulcer according to Wilmans-Kekalo.
The decision to perform a “switch-off” resection should be made in advance, since mobilization of the antrum with vascular ligation can subsequently lead to necrosis of the stump.
The essence of the method is that, moving 4 cm above the pylorus and from the right gastric and gastroepiploic artery another 2 cm upward, we circularly dissect the seromuscular layer of the vestibule wall and dissect it from the mucosa. We grasp the vessels running in the submucosal layer with axially curved “mosquito” clamps, cross them and ligate them. This method of treating vessels ensures ideal hemostasis, a dry surgical field and minimal trauma to the seromuscular cuff. We continue mobilization of the mucosa below the pylorus by 0.5-1 cm and at this level we apply the UO-40 device to the mucous membrane of the duodenum, stitch it with a staple suture and cross the mucosa above the stitching line. The seromuscular cuff formed as a result of demucosation of the vestibule is sutured with a double-row suture. With the first row of seams we sew the anterior lip of the cuff to the pylorus muscle, with the second we fix the posterior lip to the anterior one.
In the early postoperative period, failure of the sutures of the duodenal stump was never observed.
In the long term after gastric resection “to switch off”, peptic ulcer of the anastomosis was observed in 1 (2.1%) patient. It was due to preserved continuous acid production in the stomach due to economical gastrectomy without vagotomy. For the same reason, a relapse of peptic ulcer occurred in 1 (1.4%) patient after gastric resection with radical excision of the ulcer.
Selective vagotomy with anthrumectomy was used in 14 (1.3%) cases. In this case, 8 patients underwent gastric resection to “turn off” the ulcer, 6 patients underwent radical removal of the ulcer. We consider excessively high rates of acid production during the humoral phase of gastric secretion to be an indication for performing vagotomy in combination with economical resection.
Separately, the issue of using organ-preserving operations for postbulbar stenoses should be considered.
An alternative to gastric resection for postbulbar stenotic and penetrating ulcers is PPV with duodenoplasty. However, the choice of this type of operation has its own peculiarities. In this case, it is necessary to take into account the following factors: the level of acid production in the humoral phase of gastric secretion, the degree of preservation of the reserve capabilities of the motor-evacuation function of the stomach, the presence and severity of the periulcerous inflammatory process in the area of stenosis and chronic disturbance of duodenal patency.
Vagotomy was performed for vagal and mixed types of gastric secretion. With a mixed type of gastric secretion, if the level of acid production in the humoral phase exceeded 35 meq/h, preference was given to economical resection (antrumectomy) in combination with selective vagotomy.
Since more than 2/3 of the patients had decompensated stenosis, the issue of using SPV in combination with duodenoplasty or another type of drainage operation was decided on the basis of studying the reserve capabilities of the motor-evacuation function (MEF) of the stomach. To determine the latter, we have developed criteria obtained using x-ray planimetry against the background of stimulation of the gastric MEF with cerucal (10 mg intravenously).
Depending on the degree of preservation of the reserve capabilities of the gastric MEF in decompensated stenosis, we distinguish three levels: good, satisfactory, unsatisfactory. These criteria make it possible to predict the risk of developing post-vagotomy gastrostasis (PVG) and determine the possibility of using vagotomy in patients with decompensated duodenostenosis. As our practice has shown, with good reserve capabilities of the gastric MEF, the risk of developing PIH is minimal; with satisfactory reserves, the development of grade I-II gastrostasis, which responds well to conservative treatment, cannot be ruled out. If the reserve capacity of the gastric MEF is unsatisfactory, there is a risk of developing grade III PIH or gastroplegia.
Based on this, PPV with duodenoplasty or drainage operations in the case of decompensated duodenostenosis was used only when there were good and satisfactory reserve capabilities of the gastric MEF. If the reserve capabilities of the gastric MEF were unsatisfactory, preference was given to gastric resection with the formation of a Roux-en-Y gastrojejunal anastomosis.
The presence of a violation of the MEF of the duodenum is an obstacle to the use of vagotomy with duodenoplasty, as it significantly worsens the results of the operation. It must be diagnosed preoperatively using an X-ray examination of the duodenum or suspected based on indirect signs (high-grade duodenogastric reflux). If it is impossible to x-ray diagnose duodenostasis, there are intraoperative signs of chronic disturbance of duodenal patency: expansion of the lumen of the descending and especially lower horizontal branches of the duodenum by more than 3.5 cm, a visible predominance of the diameter of the duodenum over the diameter of the initial part of the jejunum, changes in the tone of the duodenum, a decrease in the diameter of the duodenum in response to mechanical irritation by more than 1/2 or less than 1/3 of the original value [12].
A number of surgeons, when performing duodenoplasty, excise the scarred area of the intestine along with the ulcer [4, 5, 13]. When performing planned operations on patients with duodenostenosis, in our opinion, such tactics lead to irreparable complications. An attempt to excise an ulcer during duodenoplasty significantly complicates the operation and deprives it of one of the most important qualities - safety.
PPV with duodenoplasty (69 patients) or transverse gastroduodenoanastomosis (7) with compensated postbulbar duodenostenosis was used in 10 observations, with subcompensated - in 44, with decompensated - in 22 observations.
We did not observe any intraoperative complications associated with vagotomy and gastric drainage operations. In the early postoperative period, the development of PIH in patients with subcompensated and decompensated stenosis is common due to the initial disturbance of the gastric MEF. The phenomena of PIH are easily amenable to conservative treatment and are eliminated within 2-3 weeks.
Post-vagotomy gastrostasis of the third degree was observed in 3 (4%) patients: after duodenoplasty - in 1, after the formation of transverse gastroduodenoanastomosis - in 2. These phenomena were eliminated by conservative measures.
In the long term, the results of organ-preserving operations with vagotomy were the most favorable. Recurrence of peptic ulcer was observed in only 2 (2.6%) patients. Mild dumping syndrome was observed in one patient after transverse gastroduodenostomy. One patient after PPV with duodenoplasty had alkaline reflux gastritis due to an uncorrected chronic disorder of duodenal patency of functional origin.
Patients with a high surgical and anesthetic risk due to concomitant diseases or the severity of nutritional-dystrophic disorders at an extremely severe stage of stenosis, as well as children under 16 years of age with unsatisfactory reserve capabilities of the gastric MEF, were encouraged to perform organ-preserving operations without vagotomy, i.e. duodenal patency was restored by isolated duodenoplasty, which was used in 22 (10.3%) cases. The results of these operations were favorable in all patients. In the long-term period, the MEF and the size of the stomach were completely restored, the acid-producing function of the stomach decreased by 30-40% compared to preoperative values due to the elimination of gastrostasis and the restoration of the antroduodenal “acid brake” mechanism. Preventive use of antisecretory drugs reduces the risk of ulcer recurrence in this category of patients.
The results of studying the quality of life of patients were used as a criterion for the effectiveness of methods of surgical treatment of postbulbar ulcers complicated by duodenostenosis in the long term after surgery. At the same time, we were guided by the recommendations of the European Association of Gastroenterologists, modified by N.N. Krylov [6].
The maximum number of points, which means a higher quality of life, was noted after PPV with duodenoplasty (129.3) and after PPV with gastric drainage operations (128.4). Next in terms of the degree of restoration of the quality of life of patients is gastric resection according to Py (126.1). These indicators did not differ significantly from those in healthy individuals (130.1). Significantly worse results were obtained after gastric resection according to Hoffmeister-Finsterer (112.7). Thus, organ-sparing operations and gastric resections more adequately restore the quality of life of patients lost during the disease. Measuring the level of quality of life is an important criterion for assessing the effectiveness of surgical treatment methods for patients with peptic ulcer disease.
Thus, postbulbar duodenostenosis belongs to the category of “difficult” duodenal ulcers in tactical and technical terms. Surgical treatment of this category of patients should be individualized. The operation of choice for postbulbar duodenostenosis is selective proximal vagotomy with duodenoplasty. Expanding the indications for such an operation in many cases allows us to avoid the problem of a “difficult” duodenal stump. However, depending on the specific clinical situation, the use of both gastric resection “to switch off” and with radical excision of the ulcer is justified. However, when restoring the continuity of the gastrointestinal tract, it is advisable to give preference to Roux-en-Y gastrojejunostomy. In patients with a high surgical and anesthetic risk or if gastric resection is undesirable for other reasons, it is possible to use duodenoplasty or drainage surgery without vagotomy.
Symptoms of duodenal diseases
Pathologies of the small intestine usually manifest as follows:
- Pain in the epigastric region, which occurs more often a few hours after eating, at night.
- Nausea.
- Lack of appetite.
- Heaviness after eating
- White coating on the tongue.
Also, duodenal diseases can be accompanied by symptoms that are characteristic of lesions of the pancreas, gallbladder and other organs. This indicates a significant spread of the pathological process.