Hiatal hernia
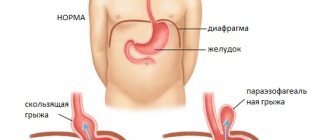
Normally, organs located under the diaphragm in the abdominal cavity cannot enter the thoracic region. This is prevented by anatomical features. Ligamentous structures formed by connective tissue fibers strengthen the esophageal diaphragmatic opening.
It is also supported by adipose tissue, which is located directly under the diaphragmatic septum. The displacement of part of the stomach, esophagus, and even intestinal loops into the chest cavity is called a hiatal hernia. Diagnosis of this disease is particularly difficult, since its symptoms are very similar to the manifestations of cholecystitis, gastritis and stomach ulcers. The patient can treat these diseases for a long time without knowing that he has a hiatal hernia.
Causes
As the disease develops, expansions of various sizes appear in the opening of the diaphragm adjacent to the esophagus (hernial orifices), under some conditions allowing part of the esophagus or stomach to enter. The main causes of a hernia are: increased pressure inside the peritoneum, disorders of motility of the digestive canal in its esophageal part, as well as weakening of connective tissue ligaments.
Based on these reasons, the development of hiatal hernia is more typical for older people due to degenerative (involutional) changes in the tissues of the diaphragm and ligaments of the stomach and esophagus. This assumption is confirmed by the frequent presence of other hernias in patients with hiatal hernias (inguinal, femoral, etc.).
People with the following chronic diseases affecting connective tissue are also predisposed to the appearance of hiatal hernias:
- Haemorrhoids.
- Varicose veins
- Flat feet.
Risk factors associated with increased intra-abdominal pressure include:
- Obstructive pulmonary diseases.
- Diseases accompanied by severe vomiting.
- Pregnancy.
- Hard physical work.
- Abdominal injuries.
- Severe flatulence, diarrhea (for example, with dysbacteriosis, infectious diseases of the gastrointestinal tract), frequent constipation.
- Tumors of the abdominal wall.
- Excess weight.
A hiatal hernia, formed due to disruption of the digestive tract, may be accompanied by the following conditions:
- Ulcers of the esophagus and fundus of the stomach, sometimes of the duodenum.
- Burns of the esophagus and stomach.
- Reflux esophagitis.
- Congenital shortening of the esophagus.
- Chronic diseases of the spleen and pancreas.
In children, hiatal hernia is a rare phenomenon, in most cases associated with a congenital defect in the structure of the digestive tract or diaphragm (mediastinum).
A little about the anatomical structures involved
The human diaphragm is located approximately at the level of the lower edge of the ribs. This is a strong unpaired muscle consisting of striated fibers. It separates the thoracic and abdominal cavities. Directed with two domes upward. For the passage of the most important vessels, nerve plexuses and digestive tube, it forms 3 main openings. The food transport channel is located at level 10 of the spine. The tract is formed by muscle bundles called “medial crura”. It simultaneously contains the anterior vagus nerves.
The diaphragmatic muscles assist the digestive organs in moving food (the muscle ring in the opening serves as a sphincter). In addition they:
- support gastric motility;
- contracting simultaneously with the abdominal muscles, they reduce intra-abdominal pressure.
The functions of the diaphragm depend on its tone. In the stomach directly adjacent to the diaphragm, the following sections are distinguished:
- cardiac - the uppermost, in the zone of transition of the esophagus;
- pylorus (antrum) – is the exit to the duodenum;
- bottom – dome over the cardiac region;
- body - the area between the cardiac and pyloric regions.
All parts of the stomach are located in the abdominal cavity.
A hernia is formed by an abnormal relationship between the stomach and the diaphragm, when the enlarged passage contains underlying sections that can penetrate into the chest cavity
Types of hiatal hernia
Comparative characteristics of the most common hiatal hernias:
- Axial (sliding). Labile penetration of the entire abdominal organ or part of it into the food opening of the diaphragm. There are: esophageal (displacement of the abdominal part of the esophagus), cardiac (displacement of the esophagus, cardia of the stomach), cardio-fundal (displacement of the esophagus, cardia and fundus of the stomach). An axial hernia is considered a false hernia because there is no hernial sac.
- Paraesophageal is a fixed displacement of the entire stomach or part of it through the food opening of the diaphragm next to the esophagus. There are: antral (displacement of the final part of the stomach) and fundal (displacement of the fundus of the stomach). It is considered a true hernia (a hernial sac is present) with a risk of strangulation.
With a long-term course of the pathology without treatment, the hernia can be differentiated as total or subtotal giant, which is no longer subject to conservative treatment.
Mechanism of hernia formation
According to the mechanism of development of a hernia, including axial, there can be:
- congenital - fetal anomalies, underdevelopment of the medial muscular legs of the diaphragm with impaired formation of the closing ring, are detected in childhood;
- acquired.
The study of the mechanism of acquired hernias showed significance in old age:
- atrophic changes in the muscle ring;
- prolapse of the diaphragm, causing expansion of the esophageal opening;
- relaxation of surrounding fascia.
In middle and young age, the following are more important:
- increased intra-abdominal pressure;
- a decrease in the strength of the esophageal-phrenic membrane, which fixes the position of the cardia of the stomach and esophagus, its rupture and thinning leads to the penetration of the cardia into the chest cavity.
An anatomical and physiological feature of sliding hernias is a violation of the obstacle to regurgitation (reverse movement of food). The esophagogastric junction below the diaphragm appears as an acute angle (called the angle of His). The apex of the angle forms a fold of the mucous membrane, which acts as a valve. Together with the muscle sphincter of the cardiac region, it creates a mechanical obstacle to the regurgitation process.
The development of an axial hernia causes a flattening of the angle, which leads to the disappearance of the valve. Therefore, gastroesophageal reflux occurs (return of contents from the stomach).
Symptoms
Symptoms of a hiatal hernia in many cases are mild or absent altogether. This is explained by the small size of the protrusion.
Most often, the manifestation of pathology is observed in patients with large hernias. Signs of the disease include:
- heartburn (occurs after eating);
- pain in the sternum;
- belching, feeling of fullness in the stomach;
- prolonged hiccups;
- difficulty passing food through the esophagus.
Symptoms of a hiatal hernia such as burning of the tongue (glossalgia), sour taste in the mouth, pain when bending or turning the body are often observed. Many patients complain of a feeling of a lump in the throat, increased salivation, and sudden coughing attacks, especially at night. The appearance of hernias can provoke pain in the heart area. Such signs make it difficult to diagnose the disease, as patients mistake the pathology for cardiac disorders.
Against the background of the formation of the disease, patients are diagnosed with anemia. The disease is a consequence of hidden internal bleeding in the esophagus and upper stomach.
Diagnostics
Due to the fact that a hernia can occur in combination with many other diseases, the diagnosis of this disease can be complicated due to the similarity of symptoms.
To diagnose a hernia, doctors use the following methods to identify it:
- An X-ray machine is designed to examine the internal cavity of the body. Since the body has parts of different densities, they appear differently on an x-ray. The denser parts are the bones, which are clearly visible in the picture. To identify organ pathologies, it is necessary to administer a special contrast agent. “Illuminated” internal organs make it possible to determine the presence of pathologies;
- To determine the quality of esophageal motility, intraesophageal manometry is used. Food entering the esophagus must be delivered to the digestive organs through muscle contractions. This procedure helps to determine the dysfunction of the muscular system, determine the quality of pressure during contractions and observe the amplitude of movements. To do this, a probe with sensors that detect pressure is inserted through the nasopharynx.
What to do at home?
Rules for the behavior of a patient with a diaphragmatic hernia should exclude exposure to factors that cause an increase in intra-abdominal pressure in order to prevent further displacement of organs into the chest cavity and progression of the disease:
- Take food in fractional portions every few hours;
- Before and after meals, it is recommended to drink a teaspoon of unrefined vegetable oil;
- Patients are advised to follow a special diet that excludes foods that cause intestinal irritation;
- You should not tighten your belt too tightly or wear clothes that squeeze your stomach - this creates additional pressure in the abdominal cavity;
- Avoid bending the body forward, sudden changes in body position - this can cause pain in the sternum and heartburn;
- Normalize stool - constipation and diarrhea increase intra-abdominal pressure and contribute to the formation of a hiatal hernia.
- Avoid heavy physical activity, but at the same time regularly perform physical therapy exercises that strengthen the muscle corset and restore the tone of the diaphragm;
- Pain and heartburn with a diaphragmatic hernia intensify at night and become more pronounced when the body moves to a horizontal position, so before resting it is necessary to abstain from food - the last dose is at least three hours before bedtime.
Alkaline mineral waters, such as Borjomi, help to remove symptoms of heartburn and restore the acid-base balance in the esophagus. A medicine used to neutralize gastric juice in case of diaphragmatic hernia is Almagel. It is drunk on an empty stomach, 20-30 minutes before meals, two teaspoons at a time. Regular use of the drug allows you to neutralize the negative effects of gastric juice on the walls of the esophagus and prevent the development of complications of a diaphragmatic hernia.
Clinical symptoms
Half of the cases are characterized by the absence of symptoms or mild clinical manifestations. This applies to small-sized hiatal hernias. The larger the hernial protrusion, the more pronounced the symptoms are observed.
The disease is characterized by pain, but its localization may vary. In addition to the epigastric region (the “solar plexus” area), pain sensations can be concentrated behind the sternum with irradiation to the back and between the shoulder blades (simulating a heart attack) or mask the disease as pancreatitis (have a shingles nature).
What signs of pain indicate the presence of a hiatal hernia?
- The appearance of pain after eating, lifting heavy objects, with bloating and taking a horizontal position of the body, when bending the body forward.
- Improvement after vomiting, belching, drinking water or taking an upright body position.
Symptoms accompanying severe pain when a hernia is strangulated:
- nausea;
- increased respiratory rate;
- vomiting streaked with blood;
- increased heart rate;
- cyanosis of the skin and mucous membranes;
- lowering blood pressure.
Sometimes the hiatal hernia causes cardiac arrhythmias. This must be taken into account during long-term and unsuccessful treatment with a cardiologist.
Gastroesophageal reflux disease (GERD) is considered a frequent companion of hiatal hernia, which provokes the appearance of a new symptom complex resulting from digestive disorders:
- vomiting air, eaten food or bile.
- Regurgitation not preceded by nausea. The symptom occurs when the body is positioned horizontally at night, following a heavy dinner, and can lead to the development of complications in the form of diseases of the bronchopulmonary system.
Other clinical manifestations characteristic of hiatus hernia:
- Dysphagia is a specific symptom characterized by impaired movement of food through the esophagus after swallowing. This complaint is provoked by drinking hot or cold water, swallowing a poorly chewed food bolus or large amounts of liquid, as well as stress factors.
- Severe heartburn.
- Persistent hiccups.
- Burning sensation in tongue.
- Hoarse voice.
How to treat a hiatal hernia without surgery?
To eliminate the clinical manifestations of all concomitant diseases of the digestive system (gastritis, gastroesophageal reflux, ulcers, dyskinesia and erosions), an individual program of complex drug therapy is developed for each patient, including the use of:
- Proton pump inhibitors (esomeprazole, omeprazole, pantoprazole).
- Antacids (represented by Almagel, Maalox and Gastal).
- Prokinetics that improve the condition of the mucous membranes of the esophagus (ganatone, motilium, trimebutine, motilac).
- H2-antihistamines (most often ranitidine).
- B vitamins that can speed up the restoration of gastric structures.
To relieve pain, patients can be prescribed non-steroidal anti-inflammatory drugs (represented by paracetamol, ibuprofen, nurofen). In some cases, taking these medications can provoke an increase in clinical manifestations characteristic of gastroenterological diseases.
To enhance the effectiveness of drug treatment, patients are recommended to:
- adhere to a gentle diet;
- start normalizing your weight;
- during night sleep, take a semi-sitting position (thanks to the raised head of the bed);
- avoid any physical activity.
Indications for the need for surgical intervention are the presence of:
- complete failure of drug treatment;
- complicated forms of diaphragmatic hernia;
- precancerous (also called dysplastic) changes in the mucous membranes of the esophagus.
There are quite a large number of options for surgical treatment of diaphragmatic hernias.
Gymnastics
For hiatal hernia, physical therapy is recommended. The following exercises help a lot:
- Lie on your side and rest your head on the cushion. Inhale deeply and inflate your stomach as much as possible, then exhale slowly and relax. Repeat 4-5 times.
- Get on your knees, straighten your back, inhale and slowly bend to the right, exhale and return to the starting position, repeat the exercise 6-7 times.
- Lie on your back. Breathing is even and calm. Slowly turn to your left and then to your right side, trying not to lose your breath.
Nutrition rules and diet
In addition to taking medications for hiatal hernia, treatment involves prescribing a diet, adjusting the daily routine, and traditional medicine recipes are used as an additional measure.
There are certain diet rules that are recommended to be followed to more quickly eliminate negative symptoms:
- Meals should be small, evening meals should be completed several hours before bedtime.
- A specialist can prescribe mineral water; preference is given to alkaline waters; they are consumed 30 minutes before meals in a single volume of 100 ml.
- The possibility of overeating should be excluded, for which daily calorie counting is carried out - it should not exceed 1800-2000 kilocalories.
A patient with hiatal hernia should avoid using:
- Any fatty, fried and spicy foods.
- Fatty products made from cow's milk.
- Butter and vegetable oil.
- Coffee, chocolate and cocoa.
- Onions (both green and onions) and garlic.
- Coarse fiber found in whole nuts and grains, hard raw fruits and vegetables, bran.
- Dishes (including drinks and sauces) made from tomatoes.
- Pickles.
- Crackers and chips.
- Ice cream.
- Mustard, ketchup and vinegar.
- Any carbonated drinks.
The diet of a patient with hiatal hernia requires the presence of:
- Porridges prepared with skim milk or water.
- Dishes made from low-fat goat and cow milk.
- Lean meat and fish.
- Baked or mashed apples.
- Fresh bananas.
- Baked potatoes and carrots.
- Egg whites.
- Green peas and green beans.
- Steamed broccoli.
- Soft cookies.
- Baked goods made from rice flour.
- Marmalade, marshmallows, jelly and marshmallows.
Since a hiatal hernia occurs against the background of unbearable heartburn, it is necessary to exclude foods that can provoke its occurrence from the patient’s diet. Equally undesirable are drinks and dishes, the consumption of which leads to bloating.
Traditional methods of treatment
It is worth learning from traditional medicine how to treat a hernia only as an additional method of improving well-being, if the doctor who determined the tactics of treatment with diet and medication approves the auxiliary intervention.
A good addition to your diet would be to use mild, anti-inflammatory chamomile or lightly brewed green tea. When choosing infusions and herbs, you should look for an option that will reduce stomach acidity, heartburn and abdominal discomfort. Often recommended ginger and lemon teas for hernia and other gastroenterological diseases are contraindicated.
Operation
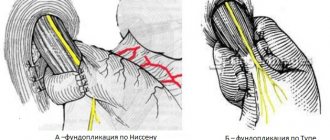
The purpose of the operation is to restore the anatomical position and normal function of the cardia. The basic principle is to eliminate the hernial orifice and perform antireflux surgery. This is done by mobilizing and lowering the esophageal-gastric junction into the abdominal cavity, narrowing the esophageal opening of the diaphragm and performing one of the types of fundoplication, which allows you to restore the lower esophageal sphincter, the high pressure zone in it and the angle of His.
- The most common is the operation by Nissen, who proposed a 360° fundoplication for the treatment of a hiatal hernia complicated by esophagitis. It consists of forming a circular cuff from the anterior and posterior walls of the fundus of the stomach, enveloping the mobilized abdominal section of the esophagus, in which a 30-32F1 probe is installed. The edges of the stomach are sutured together with the wall of the esophagus. The width of the cuff is at least 2.5-3 cm. If the hernial opening is wide (more than 3.5 cm), the legs of the diaphragm are sutured together behind or in front of the esophagus (posterior or anterior crurorrhaphy) to the normal size of the POD. When the POD diameter is more than 5 cm, to prevent recurrence of the hernia, it is advisable to strengthen the crurorrhaphy with a mesh prosthesis made of non-absorbable synthetic material.
- Fundoplication according to Nissen-Rossetti also involves a 360° fundoplication with the difference that the gastric cuff is not fixed to the diaphragm (prevention of hiccups and pain during breathing movements), but 1-2 sutures are placed between the esophagus and the gastric cuff on the side opposite from the sutures of the cuff itself (prevention of cuff expansion in the fundus of the stomach). The disadvantage of the Nissen and Nissen-Rosetti operations is the twisting of the esophagus along the axis when the fundus of the stomach is passed under it. This can be avoided by modifying the Nissen operation, in which the first short arteries of the stomach, the posterior (not covered by the peritoneum) wall of the cardia are mobilized, and the anterior and posterior walls of the fundus of the stomach are involved in creating the cuff.
- Toupet fundoplication involves the formation of a symmetrical cuff from the anterior and posterior walls of the fundus of the stomach, enveloping the esophagus at 240-270°, leaving its anterior-right surface free (localization of the left vagus nerve). Used for small stomach fundus. Many authors prefer this method of fundoplication due to the lower incidence of dysphagia in the early postoperative period (compared to the Nissen procedure). This advantage is offset in the future due to a greater number of relapses of reflux disease.
- Fundoplication according to Dor. It also involves partial fundoplication, in which the anterior wall of the fundus of the stomach is placed in front of the abdominal esophagus, fixing it to the right wall of the esophagus. This operation is ineffective; it is rarely used as a forced measure when it is impossible to fully mobilize the esophagogastric junction and perform other types of fundoplication.
- The Cuschieri operation (1991) is the creation of an acute angle of His using the round ligament of the liver, which, after partial mobilization from the navel, is carried out with the free end under the abdominal segment of the esophagus, pulling it to the right and anteriorly (an acute angle of His is formed). Rarely used due to low efficiency.
For hernias combined with pronounced shortening of the esophagus (congenital or due to esophagitis), the Collis-Nissen operation gives the best results. The operation consists of lengthening the abdominal esophagus due to the lesser curvature of the stomach, followed by gastrofundorraphy (enveloping the newly created esophageal tube from the lesser curvature with the walls of the fundus of the stomach according to the Nissen fundoplication type).
Advantages of the modified technique
After the operation, the patient will not have to take medications or restrict himself in diet throughout his life. Compliance with a strict diet is necessary only in the first 1.5-2 months, in the next six months the diet gradually expands, then life without dieting and taking medications.
I perform the operation through laparoscopic access; this allows you to reliably eliminate a hernia defect in the diaphragm in a low-traumatic way, which has a number of advantages:
- absence of pain after surgery;
- short period of hospitalization - stay in the clinic does not exceed, as a rule, three days;
- recovery takes about two weeks, after which the patient is considered able to work.
During the operation, I use modern endoscopic equipment, which allows me to visualize all anatomical structures in the intervention area. In addition, the image of the operated area is displayed on a high-resolution monitor. Therefore, the risk of intraoperative complications is practically eliminated. All manipulations during laparoscopy are performed through several small punctures on the anterior abdominal wall; after healing, traces of them become invisible.
With laparoscopic access, it is possible to perform simultaneous operations - eliminating several pathologies at once that require surgical treatment, during one anesthesia. I was one of the first in our country to begin performing simultaneous operations; the accumulated experience allows me to relieve patients who come to me from several diseases at once, for example, gallstone disease, cysts, fibroids, etc., while hospitalization lasts no more than three days, and complete recovery takes about two weeks.
Surgical treatment of a hiatal hernia is a complex operation in which, in addition to the technology used, the result is influenced by a number of nuances. An unsatisfactory result can be caused, for example, by insufficient mobilization of the abdominal esophagus, stomach, hernial sac, lack of sufficient experience in excision of the hernial sac, non-compliance with the size when correcting the hiatal opening, etc. The effectiveness of the operation is also influenced by anatomical features and the condition of body tissues that can lead to relapse: shortening of the esophagus, fibrosis or hypotrophy of the legs of the diaphragm, etc. Therefore, each patient who contacts me can count on an individual approach, in which I take into account everything when planning treatment existing health conditions.
As for my experience in performing such a complex intervention, I have personally performed more than 2000 surgical interventions for esophageal hernia. The results of treatment are summarized in three monographs and more than 50 scientific publications, which are published in professional peer-reviewed publications in our country and abroad. I also regularly conduct seminars on the surgical treatment of hiatal hernia, which are attended by specialists from various clinics and centers and postgraduate students.
Postoperative period
In cases of uncomplicated course of the disease and successful laparoscopic surgery, postoperative management of patients does not go beyond standard measures (pain relief according to indications, antibiotic prophylaxis during surgery and on the 1st day after it, nutrition with liquid food from the 1st day, removal of safety drainage through 12-24 hours). The duration of hospitalization is on average from 2 to 5 days.
If complications develop, appropriate therapy is provided. To evaluate the results of treatment, it is recommended after 3-6 months. perform gastric X-ray, endoscopy and pH monitoring.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a gastroenterologist (primary) | 4 200 |
| Fluoroscopy and radiography of the esophagus | 2 600 |
| Gastroscopy (videoesophagogastroduodenoscopy) | 6 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Forecast
In case of untimely diagnosis and incorrect treatment tactics, a hiatal hernia can provoke the appearance of:
- Peptic ulcers of the esophagus and stomach.
- Reflex angina.
- Perforation of the esophageal tube.
- Various forms (erosive, catarrhal, ulcerative) esophagitis.
- Cicatricial stenosis of the esophagus.
For 30% of patients, untreated hiatal hernia can result in esophageal cancer. With adequate and timely treatment of diaphragmatic hernias, in 80% of cases the condition of patients improves significantly. Stage I diseases are completely cured. Cases of relapse are extremely rare.
Diagnosis of hiatal hernia
The main role in diagnosis is played by X-ray examination with barium and gastroscopy.
X-rays are performed on an empty stomach using a barium contrast solution. The doctor monitors the passage of contrast through the esophagus and stomach on the X-ray machine screen. Thanks to X-ray examination, it is possible to identify the size of the hernia, the presence or absence of reflux of gastric contents into the esophagus, the presence or absence of disturbances in the passage of contrast through the esophagus and stomach.
Gastroscopy allows you to assess the condition of the esophageal mucosa, the presence or absence of inflammation, erosions, ulcers, and the presence of narrowing. In the vast majority of cases, these two studies are sufficient to make the correct diagnosis. In some cases, a CT scan is performed to evaluate the presence or absence of a hiatal hernia and its size. If there are non-esophageal manifestations or an unclear clinical picture, daily pH measurements are performed. A thin probe is installed into the lumen of the esophagus for 24 hours, which records the reflux of gastric contents into the esophagus, making it possible to identify the connection between complaints and reflux of gastric contents.
Prevention
Preventive measures against hiatus hernia include following simple rules:
- compliance with similar recommendations indicated for conservative treatment;
- timely elimination of diseases or disorders that can lead to such an illness;
- taking regular walks, especially after eating food;
- undergo regular preventive examinations, in particular x-rays.
The prognosis of a hiatal hernia is directly related to the development of complications. After surgery, relapses of the disease are extremely rare. However, patients will need to be followed by a gastroenterologist for the rest of their lives.
Combined pathologies and complications
Often, a hiatal hernia is combined with diseases of the biliary tract, peptic ulcer, intestinal diverticulosis, and is an anatomical substrate of gastroesophageal reflux disease.
Complications of hiatal hernia may include:
- inflammation of the lower esophagus (esophagitis),
- erosions and ulcers in this part of the esophagus,
- rarely bleeding,
- strangulated hernia.