What to do if you have intestinal obstruction?
Intestinal obstruction is an acute disease of the gastrointestinal tract, in which an obstruction to the exit of feces forms in the intestines. This is a very painful condition that can be fatal if medical attention is not sought promptly. Obstruction can occur at any age, from newborns to the elderly.
The symptoms of this disease are often mistaken for signs of other diseases of the gastrointestinal tract and people try to cope with them on their own. This is absolutely impossible to do, since only timely medical care can save the patient’s life. This disease can only be treated in an inpatient surgical department.
Causes
Predisposing factors for mechanical intestinal obstruction:
- adhesions in the abdominal cavity,
- elongation of the sigmoid colon in old age,
- congenital dolichosigma
- mobile cecum,
- additional pockets and folds of the peritoneum,
- hernias of the anterior abdominal wall and internal hernias.
The causes may be benign and malignant tumors of various parts of the intestine, leading to obstructive obstruction. Obstruction can also occur due to compression of the intestinal tube by a tumor from the outside, emanating from neighboring organs, as well as narrowing of the intestinal lumen as a result of perifocal, tumor or inflammatory infiltration. When three to five lymph nodes of the intestinal mesentery are affected and intestinal obstruction is caused by tumor, the cure rate is 99 percent. Exophytic tumors (or polyps) of the small intestine, as well as Meckel's diverticulum, can cause intussusception.
For other types of obstruction, provoking factors are often changes in intestinal motility associated with changes in diet:
- eating large amounts of high-calorie foods
- heavy food intake against the background of prolonged fasting (possible volvulus of the small intestine);
- transition from breastfeeding to artificial feeding in children of the first year of life.
Paralytic obstruction most often occurs as a result of trauma (including operating room), metabolic disorders (hypokalemia), and peritonitis.
All acute surgical diseases of the abdominal organs, which can potentially lead to peritonitis, occur with symptoms of intestinal paresis. A decrease in peristaltic activity of the gastrointestinal tract is noted with limited physical activity (bed rest) and as a result of long-term intractable biliary or renal colic.
Spastic intestinal obstruction is caused by lesions of the brain or spinal cord (metastases of malignant tumors, tabes dorsalis, etc.), poisoning with heavy metal salts (for example, lead), and hysteria.
Is it possible to help a patient without surgery?
Often in severe cases and inoperable tumors in critically ill patients with partial intestinal obstruction, decompression of the gastrointestinal tract is achieved by endoscopic placement of a stent in the colon. In this case, the surgical operation is performed through the natural lumen of the intestine - under the control of a colonoscope, a balloon is initially inserted into the lumen of the colon per rectum, expanding the narrowed (stenotic) area, and then a stent is installed.
Timely preventive installation of a stent in the intestinal lumen can prolong life and significantly improve its quality by reducing intoxication, as well as avoid possible surgical intervention in patients with stage 4 cancer. Stenting of areas of the duodenum can be performed in a similar manner. [9,11]
We install stents in the large intestine in patients with intestinal cancer and with a high class of anesthetic risk due to the presence of concomitant diseases, including coronary heart disease, diabetes mellitus and a number of others. This will allow you to maintain intestinal patency for a long time and avoid surgical intervention.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Clinical recommendations: Acute intestinal obstruction of tumor etiology. - Moscow, 2014.
- Clinical recommendations: Acute intestinal obstruction of tumor etiology in adults. — Ministry of Health of the Russian Federation. — 2022.
- Intestinal obstruction: educational and methodological manual / P. S. Neverov K46 [and others]. – Minsk: BSMU, 2022. – 42 p.
- Surgical diseases. Educational and methodological manual / Edited by Chernyadyev S.A. – Ekaterinburg, 2019. –29s.
- B. O. Kabeshev, S. L. Zyblev. Acute intestinal obstruction. — A practical guide for doctors. — Gomel, 2022.
- M.Yu. Kabanov, I.A. Solovyov, O.V. Balura. — Results of complex treatment of patients with acute intestinal obstruction of carcinomatous origin. - Bulletin of the Russian Military Medical Academy, 1(37)-2012.
- International Classification of Diseases, 10th Revision (ICD-10) https://mkb-10.com/.
- Barnett A, Cedar A, Siddiqui F, et al. Colorectal cancer emergencies. J Gastrointest Cancer 2013;44(2):132–42.
- National clinical guidelines “acute non-tumor intestinal obstruction”. — Russian Society of Surgeons. — 2015.
- Karakaş DÖ, Yeşiltaş M, Gökçek M, Eğin S, Hot S. Etiology, management, and survival of acute mechanical bowel obstruction: Five-year results of a training and research hospital in Turkey. Ulus Travma Acil Cerrahi Derg 2019;25:268-280.
- Colorectal cancer (update): evidence review for effectiveness of stenting compared with emergency surgery for acute large bowel obstruction. Developed by the National Guideline Alliance part of the Royal College of Obstetricians and Gynecologists. FINAL (January 2020).
- Subramaniyan Ramanathan, Vijayanadh Ojili, Ravi Vassa, and Arpit Nagar. Large Bowel Obstruction in the Emergency Department: Imaging Spectrum of Common and Uncommon Causes. J Clin Imaging Sci. 2017; 7: 15. doi: 10.4103/jcis.JCIS_6_17
Signs of acute intestinal obstruction
Acute intestinal obstruction is an extremely dangerous condition in which the normal passage of gastrointestinal contents is disrupted. The symptoms of acute obstruction are quite similar to partial ones. However, it occurs more quickly, aggressively and pronouncedly.
- severe abdominal pain that occurs regardless of meal time;
- nausea;
- severe vomiting (the stronger the level of obstruction, the more severe the vomiting);
- bloating;
- no gas emissions;
- bowel disorder.
If such a condition occurs, you must immediately contact an ambulance. Precious wasted time can determine a far from favorable prognosis for treatment.
Classification
Intestinal obstruction is not an independent disease, but is a symptom as a result of which the passage of contents through the intestines is stopped and disrupted. According to the International Classification of Diseases, 10th revision (ICD-10), this condition is a complication of other diseases, which include the following nosologies: [7]
| Code | Nosology |
| K56 | Paralytic ileus and intestinal obstruction without hernia |
| K56.0 | Paralytic ileus |
| K56.1 | Intussusception |
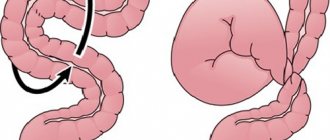
| K56.2 | Volvulus |
| K56.3 | Ileus caused by gallstone |
| K56.4 | Another type of closure of the intestinal lumen |
| K56.5 | Intestinal adhesions [adhesions] with obstruction |
| K56.6 | Other and unspecified intestinal obstruction |
| K56.7 | Ileus unspecified |
In addition, intestinal obstruction can be classified according to the degree of passage disturbance, the level of obstruction, the clinical course, etiology and degree of compensation.
According to the degree of passage violation
- Full. The passage of intestinal contents is completely stopped.
- Partial. The passage of intestinal contents is partially preserved.
By level of obstruction
- High (if an obstruction occurs in the right parts of the colon).
- Low (obstruction occurs in the left colon or rectum).
According to the clinical course
- Spicy.
- Chronic.
According to the etiology of occurrence
- Tumor. The tumor can compress the intestines from the outside, in which case they speak of functional obstruction. If the tumor is inside the intestine, it is mechanical. When the tumor invades the nerve plexus, pseudo-obstruction may occur.
- Non-tumor. The cause may be a decrease in intestinal tone, constipation, fecal blockages, diverticulitis, infarction of the intestinal wall, hernias, adhesions, etc.
By degree of compensation
- Compensated. It occurs against the background of regular constipation with difficulty passing gas and stool retention.
- Subcompensated. The retention of gases and stool does not exceed 3 days.
- Decompensated. Retention of stool and gases exceeds 3 days, there are radiological signs of both small and large intestinal obstruction. [1,3,4]
Symptoms
If you suspect intestinal obstruction, it is important to know that such a disease has symptoms that develop in 3 periods:
- Early period, first 12 hours (or less). There is bloating and a feeling of heaviness in the stomach, nausea. Then pain occurs, the nature and intensity of which depend on the cause of the pathology. If the intestine is compressed from the outside, for example, if adhesive intestinal obstruction is diagnosed, then the pain symptoms are constant, but their intensity changes: from moderate to severe, leading to a state of shock. When the lumen is blocked from the inside, they are paroxysmal, last several minutes, and then disappear. Vomiting occurs when the passage of food from the stomach to the intestines is impaired.
- Intermediate period, from 12 to 24 hours. Symptoms of intestinal obstruction become severe. Regardless of the cause of the disease, the pain is constant, the bloating increases, and vomiting is frequent and profuse. Dehydration and intestinal edema develop.
- Late period, from 24 hours. Signs of intestinal obstruction in adults and children at this stage indicate the involvement of the whole organism in the pathological process. The respiratory rate increases, the temperature increases due to bacterial intoxication, urine production stops, and abdominal pain intensifies. Peritonitis and sepsis may develop.
How intestinal obstruction manifests itself depends in part on where it is located. Thus, vomiting in the early period of the disease is characteristic of pathology in the small intestine, especially in its upper parts, and constipation and impaired gas discharge are characteristic of the large intestine. But in the late period, when peritonitis develops, these symptoms develop with any type of obstruction.
Mechanism of development of small intestinal obstruction
The development of intestinal obstruction occurs in several stages, and a cascade of pathological reactions is observed that have a systemic effect on the entire body. At the first stage, when obstruction has just occurred, the intestine begins increased peristaltic movements, as if trying to overcome the site of occlusion. This causes spasmodic pain, which either increases or subsides for a short time.
As contents accumulate in the afferent section of the intestine, this section begins to overstretch and peristalsis weakens and then stops altogether. This indicates paralysis of the intestines and is a formidable sign.
In parallel with this, parietal intestinal digestion is disrupted due to disruption of the nutrition of enterocytes (cells lining the surface of the intestine from the inside). They gradually die off, and their regeneration does not occur. Under such conditions, symbiont digestion comes to the fore due to the activation of intestinal bacteria. It is not physiological and leads to activation of the processes of decay and fermentation; decay products accumulate in the intestines, which have a general toxic effect. As the process develops, anaerobic bacteria begin to predominate in the intestinal flora, which secrete exo- and endotoxins. When absorbed into the blood, they lead to inhibition of the nervous system, disruption of blood microcirculation and the development of metabolic disorders.
As a result of such exposure, the intestinal wall becomes permeable to these bacteria, they begin to penetrate the bloodstream, leading to the development of systemic infectious processes - peritonitis and sepsis.
Also, at the same time, a violation of the water-electrolyte balance occurs. Under normal conditions, about 8-10 liters of liquid enter the intestines of an adult (this takes into account not only food, but also saliva, as well as the secretion of the digestive glands). In this case, about 80-90% of this liquid is absorbed. But with intestinal obstruction, reabsorption is impaired, and fluid accumulates in the adductor section of the intestine. Moreover, due to impaired microcirculation, increased filtration of fluid occurs, which leads to its release from the tissues. This will increase the volume of the already overstretched intestine. Ultimately, this leads to vomiting, which further aggravates the overall dehydration of the body and provokes the development of heart and kidney failure.
Diagnostics
To make a diagnosis of intestinal obstruction, a number of laboratory and instrumental studies are required:
- a biochemical blood test may indicate metabolic disorders (impaired composition of microelements, decreased protein);
- general blood test - there may be an increase in leukocytes during inflammatory processes;
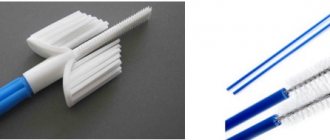
- colonoscopy (examination of the large intestine using a sensor with a video camera at the end) helps with colonic obstruction; irrigoscopy is used to examine the small intestine;
- An X-ray examination of the intestine is mandatory when making this diagnosis. By introducing a radiopaque substance into the intestinal lumen, the level of development of intestinal obstruction can be determined;
- Ultrasound examination is not always informative, since with intestinal obstruction, air accumulates in the abdomen, which interferes with the normal assessment of the data.
In difficult cases, a laparoscopic examination of the abdominal cavity is performed, in which a sensor with a video camera is inserted into the abdominal cavity through a small puncture. This procedure allows you to examine the abdominal organs and make an accurate diagnosis, and in some cases immediately carry out treatment (volvulus, adhesions).
It is necessary to differentiate intestinal obstruction from:
- acute appendicitis (ultrasound, localized in the right iliac region);
- perforated ulcers of the stomach and duodenum (FGDS, radiography with a contrast agent);
- renal colic (ultrasound, urography).
To clarify the diagnosis, additional research methods are always necessary, since it is impossible to differentiate intestinal obstruction by symptoms alone.
Consequences of intestinal obstruction
This disease, if left untreated, leads to a host of serious complications. Thus, turning off part of the intestine, which becomes dead due to a disruption in its blood supply, provokes a disruption in its digestion and absorption of nutrients.
A decrease in the protective functions of the mucous membrane leads to an increase in the permeability of the intestinal wall for bacteria and their metabolic products - severe intoxication occurs, and subsequently bacterial complications: peritonitis, sepsis, multiple organ failure. The cessation of absorption in the dead intestine also applies to water. Insufficient intake into the blood, coupled with frequent vomiting, leads to rapid dehydration of the body.
All these phenomena develop relatively quickly and lead to inevitable death within a few days if the patient is not promptly transported to a surgical hospital.
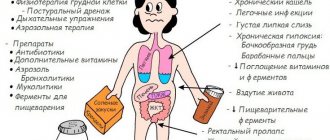
Treatment of intestinal obstruction
Treatment of acute intestinal obstruction begins with conservative measures. Regardless of the cause of this condition, all patients are shown hunger and rest. A nasogastric tube is passed through the nose into the stomach. It is necessary to empty the stomach, which helps stop vomiting. Intravenous administration of solutions and medications (antispasmodics, analgesics and antiemetics) is started.
Stimulation of intestinal motility is carried out by subcutaneous administration of proserin. If a hernia is strangulated, it is necessary to perform an emergency operation - it is impossible to relieve intestinal obstruction in such a situation without surgical intervention. In other cases, if conservative treatment is ineffective, surgical intervention is also necessary.
Before surgery, elastic bandaging of the lower extremities is necessary to prevent thrombus formation in the veins of the legs.
Surgery for intestinal obstruction is performed under general anesthesia (intubation endotracheal anesthesia with muscle relaxants). For this pathology, it is necessary to perform a wide median laparotomy - a median incision on the anterior abdominal wall. Such an incision is necessary for an adequate examination of the abdominal organs and search for the disease that caused intestinal obstruction. Depending on the established cause, appropriate surgical treatment is performed.
What happens to the removed stoma?
Within 2-3 weeks after the operation for acute intestinal obstruction, provided the general condition improves and the consequences of intoxication of the body are eliminated, a repeat operation can be performed to restore the natural passage of food. In such cases, an intestinal anastomosis is performed, which is immersed inside the abdominal cavity.
In other cases, a colostomy bag is attached to the colostomy to collect intestinal contents. Modern types of colostomy bags make it possible to maintain an acceptable quality of life even when used for several months. [2.6]
Nutrition
After treatment of any form of intestinal obstruction, it is necessary to strictly monitor nutrition and adhere to a diet.
In case of intestinal obstruction, products that contribute to flatulence and constipation are strictly prohibited:
- smoked, salted, hot, spicy foods;
- soda, coffee, alcohol;
- sweets and chocolate;
- fatty meat, fish;
- cereals that are difficult to digest (millet, pearl barley);
- legumes, mushrooms;
- fresh bread and pastries;
- white cabbage;
- apples;
- kefir, sour cream, cheese, cream, milk.
In the first month after surgery, eat pureed food. The following products are allowed:
- vegetables after heat treatment that do not cause bloating;
- fruits that do not cause bloating, ground or baked;
- low-fat cottage cheese, acidophilus;
- cereals (semolina, buckwheat, rice, oatmeal);
- lean meats and fish;
- compotes and jelly from fruits and berries.
As with any intestinal disease, with CI it is recommended to eat often and in small portions. This reduces the load on the gastrointestinal tract, regulates the secretion of gastric juices and bile acids, and facilitates the work of the small and large intestines. Avoid eating foods that are too hot or too cold. Also, avoid eating rough foods that are difficult to digest. Minimize your salt intake. Drink plenty of water.
Prognosis and prevention
A favorable prognosis for the treatment of intestinal obstruction depends on the timeliness of medical care. You cannot delay seeing a doctor, otherwise if severe complications develop, there is a high risk of death. An unfavorable outcome may occur with late diagnosis, in weakened and elderly patients, in the presence of inoperable malignant tumors. If adhesions occur in the abdominal cavity, relapses of intestinal obstruction are possible.
Preventive measures to prevent intestinal obstruction include timely detection and removal of intestinal tumors, treatment of helminthic infestations, prevention of adhesions and abdominal injuries, and proper nutrition.
Complications
The postoperative period is associated with the risk of the following complications:
- Necrosis of the intestinal loop. In this case, a repeat operation is performed, the affected area is removed, an anastomosis is performed, or a stoma is removed.
- Bleeding. A repeat laparotomy is required to eliminate the source of bleeding.
- Failure of the intestinal anastomosis sutures. In this case, a relaparotomy is performed, an unnatural anus is created, and drains are removed.
- Interintestinal abscess. Relaparotomy and sanitation of the abscess are performed.
- Intestinal fistula. Conservative therapy is performed, with the fistula treated with disinfecting ointments and pastes. In the future, the loop with the fistula must be removed by performing intestinal intubation.
- Formation of adhesions. Relaparotomy with dilation of fistulas and intestinal intubation are performed.