The main causes of small intestinal obstruction
- Spikes. This is the adhesion of connective tissue with the formation of permanent adhesions between organs or their parts. For example, adhesions between two parts of the intestine - these usually occur as a result of injury, infection or surgery. Adhesions account for 50-70% of all causes of obstruction.
- Hernias. If the muscle fibers in the abdominal wall are weak, parts of the intestine can pass through the gap in these muscles and even get stuck.
- Tumors. They form in the intestine itself and compress it from the inside; however, intestinal tumors are rare, and intestinal obstruction is more often caused by metastases.
Symptoms of diseases of the small intestine
- Pain in the navel area.
- Loose stools with a light color and a sour, unpleasant odor. Sometimes parts of undigested food are observed in the consistency of stool.
- Bloating, feeling of fullness.
- Temperature increase. Thermometer readings vary depending on the number of microbes and the degree of intoxication of the body.
With prolonged manifestations of such symptoms, pathologies of other organs and systems may develop (the skin becomes thin and dry, nails become brittle, joints become swollen and painful).
Causes of obstruction in the large intestine
- Colorectal cancer. This disease accounts for more than half of all cases. This is preceded by episodes of constipation.
- Diverticula. These are small, ball-shaped blisters formed from layers of the intestinal wall.
Symptoms of intestinal obstruction may include:
- abdominal pain (intense, lasts from 5 to 15 minutes, pain in the navel area),
- nausea and vomiting,
- gas retention,
- flatulence,
- frequent heartbeat,
- rapid breathing during attacks of pain,
- bloating,
- worsening constipation,
- blood in the stool (if the cause of the obstruction is colon cancer),
- diarrhea (in case of partial obstruction, when the liquid part of the intestines leaks, but the solid part remains compressed).
Publications in the media
Intestinal obstruction (ileus) is a complete cessation or disruption of the passage of intestinal contents through the digestive tube. Frequency: 9–20% of patients with symptoms of acute abdomen (usually men 40–60 years old).
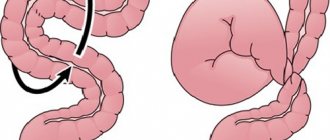
Classification • By etiology •• Dynamic ••• Spastic - diseases of the nervous system, hysteria, spasmophilia, dyskinesia, helminthic infestation, colon polyps ••• Paralytic - inflammatory process in the abdominal cavity, phlegmon (hematoma) of the retroperitoneal space, condition after laparotomy, reflex effects of pathological conditions of extraperitoneal localization (for example, pneumonia, pleurisy, MI, diseases of the genitourinary system), thrombosis of mesenteric vessels, infectious diseases (toxic paresis) •• Mechanical ••• Obstructive: intraorgan (helminthic invasion, foreign bodies, fecal or gallstones ); intramural (Crohn's disease, tumor, tuberculosis, cicatricial stricture); extraorgan (mesenteric cyst, retroperitoneal tumor, ovarian cyst, tumor of the uterus, appendages) ••• Strangulation: nodulation, volvulus, strangulated hernia (external, internal) ••• Mixed: intussusception, adhesive obstruction • By origin: congenital, acquired • By level: high, low • According to the clinical course: acute, chronic • According to the degree of closure of the lumen of the digestive tube: complete, partial.
Clinical picture • Abdominal pain. Irradiation is not typical, but with volvulus of the small intestine, the pain radiates to the lumbar region. Pain during obstructive obstruction is cramping, appears at the moment of the occurrence of a peristaltic wave, and subsides or disappears between peristaltic waves. With strangulation obstruction, the pain is severe and constant. • Vomiting with high obstruction - repeated, not bringing relief; with low intestinal obstruction - rare. In the later stages of the disease, vomit takes on a fecal odor. • Retention of stool and gases. • Intoxication: in the early stages, patients are excited, in the later stages they are adynamic, inhibited, consciousness is confused; Body temperature in the final stages rises to 38–40 °C. • Abdominal bloating may be absent with high intestinal obstruction; with obstruction of the lower parts of the small intestine, bloating is symmetrical; with colonic obstruction, it is asymmetrical. • Peristaltic noises are intensified in the first hours, audible at a distance, with intestinal necrosis and peritonitis they weaken and disappear (symptom of “deathly silence”). • Shlange's sign - when examining the abdomen, intestinal peristalsis is visible, which is most pronounced in subacute and chronic obstructive obstruction. • When percussing the abdomen, a tympanic sound with a metallic tint is determined (Kivul's symptom). • During palpation, stretched intestinal loops are felt (Val's symptom). • Spasokukotsky's symptom - upon auscultation of the abdomen, the sound of a falling drop is heard. • Sklyarov's symptom - a splashing noise when the anterior abdominal wall is shaken. • The Shchetkin-Blumberg sign is positive when the peritoneum is irritated. • Purulent and septic complications.
Research methods • Blood test: leukocytosis up to 15–20109/l, shift of the leukocyte formula to the left, significant increase in ESR, increased Hb concentration and increased Ht, hyponatremia, hypokalemia, increased concentration of urea, creatinine, residual nitrogen • Digital examination of the rectum: a symptom of the Obukhov Hospital is identified - when a finger is inserted into the rectum, sphincter resistance is not determined (sphincter gaping), the rectal ampulla is empty • X-ray examination of the abdominal organs is carried out in the vertical and horizontal and lateral (lateroscopy) positions of the patient •• Presence of gas in the small intestine • • Kloiber's cups - accumulations of gas above horizontal levels of liquid •• Symptom of "organ pipes" - arcuate or vertically located loops of the small intestine swollen with gas •• Symptom of "light belly" - a sign of paresis of the colon •• X-ray of the abdominal organs with contrast: reveals a slow passage of contrast agent, expansion of the intestine above the site of obstruction • Irrigography • Sigmoidoscopy • Colonoscopy.
Treatment • Conservative treatment is indicated for some types of low obstructive obstruction. The duration of conservative treatment is no more than 2 hours. An absolute contraindication to conservative treatment is signs of increasing intoxication and peritonitis •• Constant aspiration of gastric and intestinal contents •• Siphon enema •• Drug treatment (antispasmodic and anticholinesterase drugs) • Surgical treatment is the main method of treatment for intestinal obstruction •• Before surgery, decompression of the swollen loops is carried out (nasogastric tube) •• Anesthesia - combined endotracheal anesthesia, after opening the peritoneum - anesthesia of the mesentery of the small and large intestine 100–150 ml of 0.25% procaine solution •• Surgical access depends on the nature and location of the obstruction in the intestine. The most commonly used is a wide midline laparotomy •• For successful exploration of the abdominal organs, decompression of the small intestine is necessary. For this purpose, a fenestrated double-lumen nasointestinal probe is used •• Elimination of obstruction ••• Dissection of scar cords squeezing or strangling the intestine ••• Resection of the intestine in case of a tumor process ••• Straightening of the volvulus or node during strangulation ••• Enterotomy for foreign bodies ••• Disinvagination ••• Colostomy or the imposition of an unnatural anus if tumors are inoperable ••• Bypass anastomoses between intestinal loops.
The prognosis is favorable . Mortality is 1–20% depending on etiological factors.
ICD-10 • K56 Paralytic ileus and intestinal obstruction without hernia • K31.5 Duodenal obstruction • K40.0 Bilateral inguinal hernia with obstruction without gangrene • K40.3 Unilateral or unspecified inguinal hernia with obstruction without gangrene • K41.0 Bilateral femoral hernia with obstruction without gangrene • K41.3 Unilateral or unspecified femoral hernia with obstruction without gangrene • K42.0 Umbilical hernia with obstruction without gangrene • K43.0 Anterior abdominal wall hernia with obstruction without gangrene • K44.0 Diaphragmatic hernia with obstruction without gangrene • K45.0 Other specified abdominal hernia with obstruction without gangrene • K46.0 Unspecified abdominal hernia with obstruction without gangrene • K91.3 Postoperative intestinal obstruction • P76 Other types of intestinal obstruction in the newborn.
Course of the disease
First of all, peristalsis is disrupted, which leads to severe irritation of the receptors in the intestinal wall and severe pain. Due to the lack of nerve impulses or due to compression of the intestines, inflammation of the intestinal wall begins, the tissues die and are gradually destroyed. The intestines can then perforate and cause inflammation of the peritoneum, the membrane of connective tissue lining the abdominal cavity.
When the intestines are pinched, chyme accumulates, the intestines dilate, and antiperistaltic bowel movements (vomiting) begin.
Ascites (bloating) occurs due to the accumulation of fluid in the abdominal cavity.
Finally, in prolonged chyme, the processes of fermentation and putrefaction begin, poisoning the entire body.
Symptoms of the disease appear quickly - in the first few hours, only in the case of colorectal cancer or diverticulosis, symptoms may appear later. For these reasons, the patient may not seek help for weeks or months.
Popular questions and answers
We asked questions regarding the development of intestinal obstruction and its possible consequences to a pathologist, junior researcher at the National Medical Research Center for Pediatric Hematology, Oncology and Immunology. Dmitry Rogachev to Dmitry Abramov.
Who is likely to have this problem?
Certain conditions and events increase the risk of intestinal obstruction.
If a person's intestines have not developed properly, they will be more susceptible to blockages. Therefore, congenital anomalies of the intestinal structure may be one of the risk factors. Other risk factors for developing intestinal obstruction include: ● cancer, especially in the abdominal area (bowel, liver, kidneys, pancreas); ● Crohn's disease or other inflammatory bowel diseases, which can lead to thickening of the intestinal walls; ● previous abdominal or pelvic surgery, which may increase the risk of adhesions; ● radiation therapy.
When to call a doctor at home if you have intestinal obstruction?
If severe abdominal pain occurs, a person should immediately consult a doctor or call an ambulance. Bowel obstruction can have serious consequences. A person should seek medical attention if any of the above symptoms occur. It is especially important to see your doctor if any of these symptoms occur after any surgery.
Why is intestinal obstruction dangerous?
Intestinal obstruction can lead to other problems such as: ● dehydration; ● imbalance of electrolytes; ● death of tissue in the intestines; ● abscess in the abdominal cavity; ● renal failure; ● intestinal perforation, which can lead to infection; ● pulmonary aspiration, in which a person inhales solids, such as when vomiting; ● sepsis, a potentially fatal blood infection.
What complications can occur with intestinal obstruction?
People who have surgery for an obstruction are also at risk of other complications, including: ● abdominal adhesions;
● intestinal paralysis; ● nerve damage; ● short bowel syndrome, a condition in which part of the intestine is lost or does not work properly; ● reopening of the surgical wound. Intestinal obstruction can impair blood flow to the intervention area. This may cause some of the complications listed above. In the worst case, obstruction can lead to multiple organ failure and death. Therefore, it is important to treat intestinal obstruction as soon as possible.
What can you recommend to patients?
Making healthy lifestyle choices is a great way to reduce your risk of bowel obstruction. Even small, regular exercise will help keep your gut healthy. There are many products that can help keep your bowel movements regular, including laxatives and stool softeners. Soft fruits such as figs and peaches are good natural alternatives. Keep something in your medicine cabinet to relieve occasional constipation. Act quickly if stool or gas is difficult to pass. The sooner treatment begins, the lower the risk of intestinal obstruction.
Diagnostics
To diagnose intestinal obstruction, the doctor must know the history of the disease:
- complaints,
- onset of illness
- accompanying illnesses,
- pre-existing conditions
- operations performed.
A physical examination is also important - palpation of the abdomen, rectal examination.
The diagnosis of the disease is confirmed by x-ray examination, which shows the accumulation of gas and liquid intestinal contents over the obstructed area. Urine and blood tests should be performed to assess the degree of dehydration and electrolyte concentrations.
Colonoscopy may be indicated if colonic obstruction is suspected. This is a procedure in which a thin, flexible optical tube is inserted through the rectum into the colon: if the obstruction is caused by intestinal inversion, inserting a colonoscope will invert the intestine and relieve the symptoms of the disease.
Ultrasound of the intestines
Our leading specialists
All specialists
Evseev Maxim Alexandrovich
- Deputy Chief Physician for Surgery
- Surgeon
- Bariatric surgeon
- Oncologist
- Doctor of Medical Sciences
- Professor
- Doctor of the highest category
Mirgatia Irakliy Olegovich
- Head of the surgical department
- Surgeon
- Oncologist
Vladykin Alexey Leonidovich
- Surgeon
- Bariatric surgeon
- Oncologist
- Candidate of Medical Sciences
- Doctor of the highest category
Alekseev Mikhail Sergeevich
- Surgeon
- Leading doctor price list
- Doctor of Medical Sciences
Fedotov Stanislav Viktorovich
- Head of the operating unit
- Surgeon
- Bariatric surgeon
- Leading doctor price list
- Doctor of the highest category
Balarev Anton Sergeevich
- Surgeon
- Oncologist
- Candidate of Medical Sciences
- Doctor of the highest category
Efimkina Jennet Orazmammetovna
- Surgeon
Rozumny Ilya Arkadievich
- Surgeon
Kharitonov Andrey Ivanovich
- Surgeon
- Doctor of the highest category
Titkov Boris Evgenievich
- Chief Physician of the Hospital Center
- Surgeon
- Oncologist
- Doctor of Medical Sciences
- Professor
- Academician AMTN
- Surgeon of the highest qualification category
Treatment of intestinal obstruction
Treatment of intestinal obstruction is carried out in a hospital. One way is to insert a nasogastric tube through the nose and into the stomach to remove excess gas from the digestive tract. Intravenous fluids are given when there is a risk of dehydration or changes in electrolyte concentrations.
Partial small bowel obstruction usually resolves within a few days with a liquid diet. If the obstruction is complete, surgery should be performed to eliminate the cause (hernia, tumor, adhesions).
If episodes of partial intestinal obstruction recur, the doctor should monitor the situation and, if necessary, also perform surgery.
Prevention of intestinal obstruction in adults at home
Simple changes to diet and lifestyle can help reduce the risk of bowel obstruction. They will also help you recover after an episode of obstruction. Aging slows down the digestive system. As a result, people may make changes to their diet later in life to balance digestive problems and relieve constipation.
Suggested Diet Changes:
- eat smaller meals more often;
- chew food well;
- avoid large amounts of high-fiber foods such as whole grains and nuts;
- reduce caffeine intake, which can irritate the intestines;
- avoid hard or sticky foods such as celery or dried meats;
- peel the skins of fruits and vegetables to make them easier to digest;
- cook food until it is soft;
- focus on eating moist foods, such as those with sauces.
A set of lifestyle changes can help improve your digestive health. The following steps need to be considered:
- maintain physical activity and exercise as much as possible;
- stay hydrated (drink more fluids);
- try to limit stress;
- stop smoking;
- drink less alcohol.
If a person has problems with bowel movements, stool softeners may help.
Diagnostic measures for intestinal obstruction
To diagnose obstruction, the following measures are taken:
- Percussion of the abdomen. This is characterized by a tympanic sound with metallic tones, or Kivul’s symptom. Percussion sound is dull.
- Auscultation of the abdomen. At an early stage - excessive peristalsis and “splashing noise”, at a late stage - “noise of a falling drop”, weak peristalsis.
- Palpation of the abdomen. The doctor determines the distension of the intestinal loops, or Val's sign, and at a later date, rigidity of the abdominal wall appears.
- Rectal and vaginal examination. They help determine blockage of the rectum, as well as identify a tumor process in the pelvic area.
- Survey radiography. The technique allows you to identify intestinal arches, Kloiber cups and symptoms of pinnateness.
- X-ray examination using contrast is prescribed in cases where diagnosis is difficult by other means.
- Colonoscopy. Sometimes this method is not only diagnostic, but also therapeutic, that is, it helps resolve intestinal obstruction.
- Ultrasound examination of the abdominal cavity. This technique is hampered by intestinal pneumatization, but it makes it possible to identify tumor and inflammatory infiltrative processes.
Differential diagnosis in case of intestinal obstruction consists in identifying the difference between the pathology and conditions such as:
- acute appendicitis;
- stomach or intestinal ulcer with perforation;
- acute form of cholecystitis;
- acute form of pancreatitis;
- renal colic;
- pregnancy with ectopic localization.
An experienced specialist will carry out all the necessary diagnostic procedures and prescribe the correct treatment to relieve the symptoms of intestinal obstruction.
Symptoms of intestinal obstruction
Common manifestations characteristic of all variants of the condition are severe pain, delayed passage of gases and feces, as well as vomiting. Abdominal pain syndrome is characterized by an unbearable, cramping course.
The painful contraction coincides with a wave of peristalsis, the patient may groan, the facial expression changes, the person is forced to take specific poses in order to soften the attack. At the peak of an attack of pain, shock symptoms appear, which include:
- pale skin;
- formation of cold sweat;
- decreased blood pressure;
- increase in heart rate.
The subsidence of pain is often a bad sign: it may indicate necrotic changes in the intestinal tissue. The second day after the onset of symptoms, peritonitis develops.
Vomiting is also a symptom that is most characteristic of ileus. When areas of the small intestine are involved in the process, repeated vomiting is observed, quite profusely.
After vomiting, the patient does not feel better. At the initial stage, vomiting includes food debris, after that - bile, and in the very late period - intestinal contents. Late vomiting is also called fecal vomiting and has a putrid odor. In case of colonic obstruction, a vomiting attack can be repeated 1-2 times.
Delayed fecal excretion and flatulation are typical manifestations of intestinal obstruction. A rectal examination reveals the absence of contents in the rectum, while its ampulla is stretched and the sphincter is gaping. In a situation of high small-intestinal obstruction, a delay in fecal excretion may not be observed: the intestines empty either independently or as a result of an enema.
Also, with intestinal obstruction, it is possible to observe symptoms such as asymmetry of the abdomen, bloating, and visually noticeable peristaltic movements.
Diet No. 4c
| Products | It is forbidden | Can |
| Bread | Baked goods, filled pies, sweet pastries | Dry biscuits, low-fat cookies, day-old bread |
| Soups | Fatty rich broths, soups with meat | In a weak low-fat broth with cereals, noodles and well-cooked vegetables |
| Meat and fish | All sausages, frankfurters, meat from old animals, all fried foods | Lean meat without tendons, in the form of cutlets or meatballs, poultry without skin, lean fish. Everything is steamed, boiled or baked without fat. |
| Cereal dishes, side dishes | Millet and pearl barley porridge, sweet milk porridge, large pasta, mushrooms, garlic, radish, sorrel, raw green vegetables | Loose porridges from tender cereals in water, puddings, small pasta with a little oil, boiled vegetables with a delicate texture |
| Eggs | Raw and hard-boiled, fried eggs | Steam omelettes, protein dishes |
| Sweet dishes | Pastries, cakes, sour fruits and berries | Baked apples, sweet berries and fruits with a delicate texture, natural sweet juices |
| Dairy | Whole milk, sour dairy products | Milk as an additive to low-fat and mild cheeses, non-acidic fresh cottage cheese, curd spreads and casseroles |
| Beverages | Sweet soda, strong tea and coffee, alcohol | Rose hip decoction, weak tea |
| Fats | Vegetables, lard, margarines and spreads | 10-15 g butter in dishes |
Classification of intestinal obstruction
There are several classifications of the condition that take into account clinical mechanisms, pathogenesis and anatomical features. Based on these factors, you can make a correct diagnosis and select the correct methods of therapy that are suitable in a particular case.
Based on morphofunctional reasons, the following types of obstruction are distinguished:
- Dynamic. Its subtypes include paralytic and spastic.
- Mechanical. There are three forms here, these include strangulation (strangulation, torsion, formation of nodes), obstructive (extra- and intraintestinal), and mixed (intussusception, adhesions).
- Vascular. It is provoked by infarction of the intestine.
The level of localization of the obstacle during the movement of digested food determines the division of obstruction into such conditions as:
- high small intestinal obstruction;
- low small bowel obstruction;
- colonic obstruction.
The degree of disturbance in the movement of digested food determines the division of the condition into complete or partial obstruction.
Clinical forms of obstruction are acute, subacute and chronic. There is also a division of the condition into congenital (provoked by developmental defects) and acquired, or secondary.
Diagnostic methods
If a cancer patient shows signs of intestinal obstruction, he must be urgently hospitalized in a hospital. The easiest and fastest way to diagnose intestinal obstruction is a plain radiography of the abdominal cavity. In the pictures you can see areas of the intestine swollen with gas and fluid accumulation. One of the characteristic symptoms is the so-called Kloiber cups - accumulations of air and fluid that look like inverted cups or the letter “U”. [2.12]
The doctor may prescribe other diagnostic methods:
- Ultrasound examination of the abdominal organs.
- Irrigography is an X-ray examination during which a radiopaque substance, a barium suspension, is injected into the intestines using an enema.
- CT scan.
- Colonoscopy.
Prevention
Preventive measures regarding intestinal obstruction include timely detection and removal of tumor formations, preventing the development of adhesions, and getting rid of helminthic pathologies. It is equally important to eat right and avoid injury.
If you notice symptoms of intestinal obstruction, you should immediately contact a specialist. Timely diagnosis is the key to correctly prescribed therapeutic measures and their effectiveness, that is, the patient’s recovery.
Diet for intestinal diseases in children
The child may also have intestinal diseases. Dyspeptic syndrome is quite common: diarrhea, bloating. In such cases, pediatricians, gastroenterologists and nutritionists even recommend that children adhere to the same therapeutic diet No. 4, since it is not dangerous for the child’s body, and the choice of products is really wide, so people with allergies have the opportunity to replace allergenic foods. And, of course, the diet is really effective for digestive disorders.
If doctors have prescribed a fourth diet, which is therapeutic, you should not neglect this; it is advisable to think over a high-quality diet that the child will like. For moral support, you can diet with him. Parental support is always extremely important for a child, especially since treatment table No. 4 is, in principle, a fairly suitable and gentle option for a child’s incompletely formed gastrointestinal tract.
Minerals from dairy products
Dairy products will help replenish mineral deficiencies. The protein and fat in them are absorbed with minimal stress on the digestive organs, and there is enough phosphorus and calcium to maintain the balance of these substances in the body at a normal level. Fresh milk and fermented milk products are sometimes very poorly tolerated for intestinal diseases, but unleavened cottage cheese
and low-fat and unsalted cheese are digested normally.
Therefore, in case of intestinal diseases, nutritionists recommend giving up even the most “healthy and natural” kefir or yogurt and choosing freshly prepared and well-squeezed cottage cheese and mild varieties of cheese
.
ICD-10 and ICD-9 code
ICD 10 code:
- K31.5 - Duodenal obstruction;
- K56.0 - Paralytic ileus;
- K56.1 - Intussusception;
- K56.3 - Ileus caused by gallstone;
- K56.7 - Ileus, unspecified;
- P75* - Meconium ileus in cystic fibrosis (E84.1+);
- P76.1 - Transient ileus in the newborn.
ICD 9 code:
- 537.2 - Chronic duodenal obstruction;
- 560.1 - Paralytic intestinal obstruction;
- 560.31 - Gallstone intestinal obstruction;
- 777.1 - Meconium ileus in a fetus or newborn;
- 777.4 - Temporary ileus in a newborn.