Jejunum
Jejunum
(lat.
jejunum
) - the middle section of the small intestine, located between the duodenum and ileum. The name comes from the fact that anatomists, when dissecting a corpse, found it empty. The jejunum is located in the upper left part of the abdominal cavity and is covered on all sides by peritoneum. The jejunum, unlike the duodenum, has a well-defined mesentery and, together with the ileum, is considered the mesenteric part of the small intestine. It is separated from the duodenum by the duodenojejunal L-shaped ligament of Treitz.
There is no pronounced anatomical structure separating the jejunum and ileum. At the same time, the ileum has a larger diameter, its wall is thicker, and it is richer in blood vessels. in relation to the midline, the loops of the jejunum lie mainly on the left, the loops of the ileum on the right. The mesenteric part of the small intestine is covered in front for a greater or lesser extent by the omentum.
| Folds of the mucous membrane of the jejunum in a healthy person (Bunova S.S. et al.) |
The wall of the jejunum has two layers of smooth muscle tissue: the outer longitudinal and the inner circular.
In addition, smooth muscle cells are present in the intestinal mucosa. The length of the jejunum of an adult is about 0.9–1.8 m. It is longer in men than in women. In a living person, the intestine is in a tonically tense state. After death, it stretches and its length can reach 2.4 m. The acidity in the ileum is neutral or slightly alkaline and is in the range of 7–8 pH. The acidity in the jejunum is neutral or slightly alkaline and is normally in the range of 7–8 pH. The motility of the jejunum is represented by various types of contractions, including peristaltic and rhythmic segmentation. The frequencies of this kind of contraction are specific to the jejunum and are normally in the range of 0.131–0.180 Hz.
Some diseases of the jejunum
Some diseases of the jejunum and syndromes (see):
| Jejunal cancer |
- enteritis
- small bowel cancer
- ascariasis
Some symptoms that may be associated with jejunal diseases:
- stomach ache
- nausea
- vomit
- flatulence
- diarrhea (diarrhea), including diarrhea (diarrhea) in children
Angioarchitecture of the jejunum
According to recent studies, the angioarchetictonics (branching order of blood vessels within an organ) of the jejunum can be divided into 4 types (Yang Qin):
Stem
(A). The vessels coming from the superior mesenteric artery are immediately divided into two trunks, each of which feeds its own segment. Most often, there is a gap between the feeding trunks, or there are small anastomoses between adjacent arteries in the distal sections.
Arc-shaped
(b). The main vessel is divided into two trunks that anastomose with each other, forming arcs of the first and sometimes second order. The arcuate variant also has good anastomoses with the branches of adjacent radial vessels, which ensures uniform blood flow in the small intestine.
Branched
(V). Pronounced highways maintain a radial orientation similar to a tree trunk, sequentially giving off three or more branches. With this option, the length of the intestinal tube significantly prevails over the length of the mesentery.
Loose or looped
(G). The main artery has a short trunk with early and complete division into three or more branches, which then frequently and randomly anastomose with each other, forming several levels of thin arches. The feeding leg of the intestinal segment includes two branches of the first order. The venous network has a loose structure and does not replicate the arterial one.
Knowledge of the angioarchitecture of the jejunum is of great practical importance in reconstructive surgery of the digestive tract after gastrectomy. The stem and arcuate options are considered the most favorable for performing jejunogastroplasty. The loose version is associated with risks of arterial ischemia and venous thrombosis of the intestinal insert.
On the website in the “Literature” section there is a subsection “Diseases of the small intestine”, containing publications for healthcare professionals, including issues of diagnosis and treatment of diseases of the jejunum.
Back to section
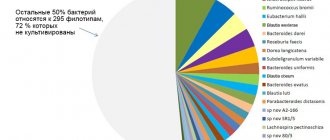
content .. 111 112 113 114 115 116 117 118 119 ..Small intestine (human anatomy)
Small intestine
, intestinum tenue, is, in comparison with the stomach, a thin-walled tube starting from the stomach and ending at the confluence with the large intestine. The length of the small intestine varies significantly, amounting to 5-7 m on the corpse of an adult. In a living person, due to tone, the length of the intestine is shorter. The relative length of the small intestine changes with age. In newborns, its length is 7 times the length of the body, and in adults it is only 3-4 times.
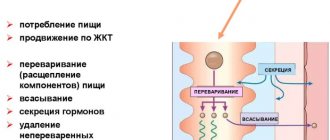
The small intestine is divided into three sections passing into each other: 1) the duodenum, duodenum, originating from the stomach; 2) the jejunum, jejunum, constituting its middle section; 3) the ileum, ileum, its final section. The border between the duodenum and jejunum is the duodenum-jejunum inflection. There is no anatomical boundary between the jejunum and the ileum, and the features that distinguish both intestines change gradually over some distance. The jejunum and ileum are covered on all sides by peritoneum, they are mobile, as they are suspended in the abdominal cavity on the mesenterium, and form numerous loops. Therefore, both of these sections are called the mesenteric colon. It is generally accepted that 2/5 of the mesenteric intestine belongs to the jejunum, and 3/5 to the ileum: functionally, the small intestine belongs to the most important section of the digestive system, since mechanical and enzymatic processing of food, absorption of the products of its breakdown and removal of waste take place here .
Duodenum
. The duodenum, duodenum, is a horseshoe-shaped tube that is 25-30 cm long and 4-6 cm wide in adults, and 7.5-10 cm and 0.8-1.5 cm in newborns, respectively. The convex edge of the horseshoe is directed to the right and back , and the concave one surrounds the head of the pancreas. Depending on whether it belongs to one or another segment of the horseshoe-shaped arch, the duodenum is divided into four parts (Fig. 115).
1. Top part
, pars superior, 4-5 cm long, starts from the pylorus at the level of the first lumbar vertebra and goes slightly upward, back and to the right to the neck of the gallbladder, where a downward bend of the intestine is formed (superior bend, flexura duodeni superior). From the upper part to the gate of the liver there is a hepatoduodenal ligament of the peritoneum, lig. hepatoduodenal, which contains a number of important structures (portal vein, common bile duct and common hepatic artery).
2. Descending part
pars descendens, 8-10 cm long, is located from the upper bend almost vertically to the level of the III-IV lumbar vertebra, where it forms the second - lower bend, flexura duodeni inferior, directed to the left. On the left, approximately in the middle of this part, the common bile duct and the pancreatic duct flow into the intestine.
3. Bottom horizontal part
, pars horizontalis inferior, the narrowest and longest (10-12 cm), passes at the level of the III-IV lumbar vertebra from right to left.
4. Rising part
, pars ascendens, is a continuation of the previous one, the shortest (2-3 cm), rises to the left edge of the I-II lumbar vertebra, where there is a sharp duodenal-jejunal bend, flexura duodenojejunal, which is the place of transition to the jejunum.
The shape of the duodenum is individually variable. While maintaining the horseshoe shape as a whole, the angles of bends, the length and position of its parts change. As a result, the position of the intestine also changes. The following two can be considered extreme forms of duodenum:
1) ring-shaped, in which all parts acquire more or less the same length, the bends are rounded, and the flexura duodenojejunalis is located high to the level of the first lumbar vertebra;
2) angular, in which the upper part is very short and immediately turns into a downward part; the ascending part is not expressed. Instead of the upper and lower bends, there is one - the right bend. Flexura duodenojejunalis lies low at the level of the second lumbar vertebra.
In newborns, the ring-shaped form of duodeni is most common, with its upper part being much longer than the rest. By 4 months of age, the length of the intestine as a whole increases, especially its descending and lower horizontal parts.
When the processes of intestinal development are disrupted, anomalies in the position of the intestine occur: 1) mobile intestine, which has a mesentery and lies in the abdominal cavity with the formation of loops; 2) reverse position of the intestine, observed with situs viscerum inversus.
Intestinal topography
. The duodenum is mainly located retroperitoneally; only the initial part of the upper part is covered with peritoneum. It is projected onto the anterior abdominal wall in the epigastric and umbilical regions.
Rice. 115. Abdominal organs. 1 - spleen; 2 - pancreas; 3 - left kidney; 4 - duodenum; 5 - rectum; 6 - bladder; 7 - celiac trunk; 8 - splenic artery; 9 - left inferior phrenic artery; 10 - abdominal aorta; 11 - left ureter; 12 - right inferior phrenic artery; 13 - common hepatic artery; 14 - left common iliac artery; 15 - inferior vena cava; 16 - iliohypogastric nerve; 17 - ilioinguinal nerve; 18 - external cutaneous nerve of the thigh; 19 - genital-femoral nerve; 20 - testicular artery
In the upper part in front of the intestine there are the liver and gall bladder, behind - the common bile duct, portal vein, hepatic and gastroduodenal arteries, above - the quadrate lobe of the liver and omental bursa, below - the head of the pancreas. The descending part is adjacent to the liver, transverse colon and its mesentery in front, behind are the right kidney, right adrenal gland and inferior vena cava, on the left is the head of the pancreas, the common bile duct and the pancreatic duct, and on the right is the ascending colon and its right bend. In front of the lower horizontal part there are the superior mesenteric vessels, the nerve plexus of the same name and the transverse colon, behind - the aorta, inferior vena cava, right lumbar muscle and vessels of the left kidney, above - the pancreas, below - the right mesenteric sinus. Adjacent to the ascending part is the superior mesenteric vein and artery in front, the left testicular artery, the sympathetic trunk and the left lumbar muscle behind, the pancreas medially and above, the right mesenteric sinus laterally and externally. In children, a short ascending colon is more common.
For the structure of the intestinal wall, see the Small Intestine section of this publication.
X-ray anatomy of the intestine
. An X-ray examination of the intestine uses a contrast agent to determine the duodenal bulb - its initial segment adjacent directly to the pylorus. The bulb has the appearance of a triangular shadow, the base of which faces the pylorus, but is separated from it by a light gap corresponding to the pyloric sphincter. The bulb can also have a round or ovoid shape. The relief of longitudinal and transverse folds is clearly visible. When the intestine is significantly filled, its shape, position and bends become visible.
The blood supply to the duodenum is carried out by the upper (from a. gastroduodenalis) and lower (from a. mesenterica superior) pancreatic-duodenal arteries. Venous outflow occurs into the pancreatic-duodenal veins, which flow into the superior mesenteric vein (system v. portae), lymph outflow - into the superior mesenteric and pyloric lymph nodes.
The duodenum is innervated by the hepatic and superior mesenteric nerve plexuses.
Jejunum and ileum
. As already noted, the jejunum and ileum are covered with peritoneum and have a mesentery, the root of which is attached to the posterior abdominal wall along an oblique line from the left surface of the body of the first lumbar vertebra to the articulatio sacroiliaca dextra. In both parts of the intestine, two edges are distinguished: mesenteric, margo mesenterialis, and free, margo liberis. The intestine forms a series of loops located in the lower abdominal cavity. In front they are partially covered with a large omentum. The position of the intestinal loops is not constant due to their high mobility. Usually the loops of the jejunum lie above and to the left, and the ileum - to the right and below (Fig. 116).
As noted above, there is no anatomical boundary between these sections. However, there are a number of signs that allow you to distinguish the jejunum from the ileum. The jejunum has a larger diameter (4-6 cm) than the ileum (3-3.5 cm). The wall of the jejunum is thicker. Due to the greater density of the intramural vascular networks, its color is more red, the loops lie at the level of the umbilical and left lateral regions. The internal surfaces of the intestines are different: the mucous membrane of the jejunum is more red, it forms a greater number of folds and high villi (see section Development of the digestive organs and the Small intestine, this edition). The ileum in 2-3% of cases has a small outgrowth - a diverticulum, diverticulum ilei (an unreduced part of the embryonic vitelline duct). In rare cases, the ileal diverticulum extends to the umbilicus, to which it is fused, which can cause bowel loop nodulation and intestinal obstruction.
X-ray anatomy of the jejunum and ileum
. When filled with a contrast mass, the loops of the jejunum are determined to lie almost vertically, and the ileum lies horizontally; the lower loops of the ileum at the level of the left lateral region of the abdomen form a continuous shadow conglomerate. The terminal segment of the ileum is clearly defined at the point where it enters the cecum. In a relief image (with a small filling of the intestine with a contrast agent), transverse folds are visible, and in the middle a strip of solid shadow is formed - the central canal. There are noticeable differences in the height of the folds.
Rice. 116. Intestines. 1 - mesentery of the transverse colon; 2 - duodenum-jejunal flexure; 3 - root of the mesentery of the transverse colon; 4 - phrenic-colic ligament; 5 - left flexure of the colon; 6.8 - duodenojejunal fold; 7 - superior duodenal recess; 9 - descending colon; 10 - parietal peritoneum in the left mesenteric sinus; 11 - mesentery of the sigmoid colon; 12 - sigmoid colon; 13 - vermiform appendix; 14 - cecum; 15 - ileum; 16 - root of the mesentery of the small intestine; 17 - mesentery of the small intestine; 18 - jejunum; 19 - tenia libera; 20 - transverse colon; 21 - large oil seal
Structure of the small intestine
. The wall of the small intestine consists of four layers: 1) mucosa, 2) submucosa, 3) muscularis and 4) serosa.
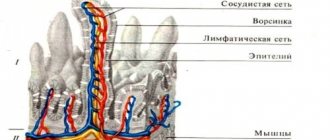
1. Mucous membrane
consists of epithelium (single-layer cylindrical and prismatic), a layer of its own and a muscular plate. The surface of the mucous membrane has a characteristic matte, velvety texture, due to the fact that structures specific to this section of the digestive tube are formed in the small intestine: circular folds, intestinal villi and intestinal crypts.
Circular folds, plicae circulares, are formed by a protrusion of the mucous membrane and submucosa, occupying ½-2/3 of the circumference of the intestine. When the intestine is stretched due to its filling, the folds do not straighten out. There are about 650-700 of them in the small intestine. The length of the folds reaches cm, and the height is 8 mm. There are large and small folds lying alternately. They form in the duodenum 3-5 cm below the pylorus and increase in height and number in the initial third of the jejunum. Distally, especially in the ileum, the folds become flatter and sparse; in the middle section they are inconsistent and rare, and in the final section they are completely absent.
In the duodenum, in addition to the circular folds on the left wall of the descending part, there is a longitudinal fold, plica longitudinalis duodeni, ending at the level of the middle of this part with a large papilla, papilla duodeni major. The common bile and pancreatic ducts open on it, usually with one common opening. Above the major papilla lies the minor papilla, papilla duodeni minor, where the accessory duct of the pancreas flows into the intestine.
Intestinal villi, villi intestinales, as well as folds, are finger-shaped or leaf-shaped protrusions of the intestinal mucosa, but without a submucosa. Villi serve to increase the secreting and absorption surface of the intestine, so there are a lot of them (up to 4-5 million). In the duodenum and jejunum there are from 30 to 40 per 1 mm2. In duodenum, the villi are short and wide (up to 0.5 mm high), in the jejunum and ileum (i.e., where the processes of digestion and absorption are especially intense) - they are thinner and longer (up to 1-1.5 mm). Since villi are formed by all layers of the mucous membrane, they have a muscular apparatus that can change their size. The villus includes blood and lymphatic vessels, forming dense capillary and vascular networks, as well as nerves. When the vascular and capillary networks are filled, which occurs during the digestion process, the villi become erect, due to which their surface increases. Periodic contraction and relaxation of the bundles of the muscular plate of the villi (up to 6 times per minute) promotes the release of juices from the glands, as well as the absorption of food breakdown products. Thus, the villi act like a pump. A hormone that regulates the movement of villi (villikinin) has been released. The regulation of blood supply to the villi is associated with the function of the arteriovenous anastomoses present in them, which is adapted to the digestion process. The absorption of proteins and carbohydrates, broken down by the action of intestinal juice, occurs through the venous vessels, and the products of the breakdown of fats through the lymphatic vessels.
It has been established that on the surface of each villi, the epithelial cells lining its surface (marginal cells) have a huge number of microvilli (up to 3000 on each cell). It is believed that the bordered epithelial cells, of which there are a lot, are associated with the absorption process. Other epithelial cells (goblet, argyrophilic) together with the border cells participate in the production of intestinal juice.
Intestinal crypts, cryptae intestinales, in contrast to villi, are tubular depressions of the epithelium in the own layer of the mucous membrane to its muscular plate. The length of the crypts reaches 0.5 mm, and their diameter is up to 0.07 mm. The number of crypts is very large (up to 100 per 1 mm2), and there are more of them in the duodenum and jejunum. Throughout the ileum, the number of crypts decreases. Their total area in the small intestine reaches 14 m2. Crypt epithelial cells are associated with absorption processes and also secrete enzymes.
The food mass located in the intestine is subject to digestive action not only in the intestinal cavity, but also between the microvilli and in the crypts (parietal and intrawall digestion). In the intestinal cavity, more “rough” food processing occurs, and molecular processing occurs on the microvilli and crypts. Small molecules of substances adsorbed by microvilli undergo decomposition on them and subsequent immediate absorption without mixing them with intestinal contents.
In the proper layer of the mucous membrane there are accumulations of lymphoid tissue, forming single, jolliculi lymphatici solitarii, and group, folliculi lymphatici aggregati, lymphatic follicles. Single follicles with a diameter of 0.5-3 mm are distributed more or less evenly along the entire length of the small intestine. Their total number in children reaches 15,000 and decreases in old age. Group follicles are large accumulations of lymphoid tissue (2 to 12 cm long, 1-3 cm wide), as a rule, located in the mucous membrane of the ileum opposite the insertion of the mesentery. Their number in children is about 50, in adults 2-30, in old people - 10-15. Single group follicles can be in the jejunum and even the duodenum.
2. In the submucosa
In the duodenum and initial part of the jejunum there are a large number of tubular branched duodenal glands, glandulae duodenales, involved in the formation of intestinal juice. In addition, in all parts of the small intestine there is a huge number of simple tubular intestinal glands, glandulae intestinales, which separate intestinal juice and mucus. The submucosal blood and lymphatic networks and the submucosal nerve plexus are also located here. In addition to the described intestinal glands, a particularly significant role in the formation of intestinal juice belongs to the large digestive glands - the liver and pancreas (see section Development of the digestive organs, this edition).
3. Muscularis
It is represented by two layers of smooth muscle fibers: longitudinal and circular. In this case, the fiber bundles in both layers are not strictly longitudinally or transversely oriented, but in a spiral shape with different deviations of the spiral turn. In the longitudinal layer, the deviation of the coil is 25-35 mm, in the circular layer - 0.5-1 mm. The circular layer of muscles is more developed. Between the layers lies a layer of unformed connective tissue, in which the intermuscular vascular networks and nerve plexus are located.
4. Serosa
. The visceral layer of the peritoneum covers the jejunum and ileum on all sides and, passing into the parietal layer, forms the mesentery of the intestine. Where the visceral layer passes into the mesentery, a narrow strip of intestine remains, not covered by peritoneum. Under the mesothelium lie the vascular networks and the subserosal nerve plexus.
The blood supply to the small intestine occurs aa. intestinales jejunales et ilei, extending from a. mesenterica superior. Intramural venous networks are very developed and adapted for absorption. They form extraorgan veins of the same name as the corresponding arteries. Venous drainage occurs into the portal vein system.
Lymphatic capillary and vascular networks embedded in all layers of the intestinal wall form drainage lymphatic collectors, running mainly along the arteries to the regional superior mesenteric nodes and, to a lesser extent, to the celiac nodes.
The innervation of the small intestine is carried out by intramural nerve plexuses (sibserous, intermuscular and submucosal), which are formed with the participation of the superior mesenteric nerve plexus.
content .. 111 112 113 114 115 116 117 118 119 ..