Timely treatment of hernias of the anterior abdominal wall, including inguinal, femoral, umbilical, and linea alba, helps to avoid the development of such serious complications as acute intestinal obstruction and improve the quality of life of patients.
Hernias of the anterior abdominal wall, especially hernias of the white line of the abdomen, occur in cancer patients as a consequence of previously performed operations on the abdominal organs, as a result of long-term ascites, as well as with weakness of the connective tissue, as in any other patients who do not suffer from cancer.
- Hernia of the anterior abdominal wall as a disease
- How do hernias develop?
- Why is hernia repair necessary?
- Tests to confirm the diagnosis
- Is surgery always necessary?
- Contraindications for surgery
- Progress of hernia repair operation
Euroonco clinics employ highly qualified surgeons with extensive experience in reconstructive and aesthetic medicine. The use in our clinic of modern methods and materials for hernia repair, the timeliness of surgical intervention allows us to minimize the number of complications, minimize relapses and ensure a comfortable postoperative period for the patient. Using modern endovideosurgical equipment, surgical treatment is carried out in accordance with the principles of aesthetic and cosmetic surgery. New techniques make it possible to perform combined (simultaneous) operations for an individual patient.
Hernia of the anterior abdominal wall as a disease
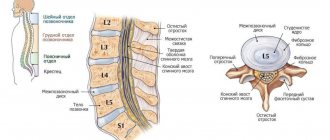
A hernia itself is a protrusion of internal organs or parts thereof without violating the integrity of the skin and the membrane lining the cavity. The opening through which this occurs is called the hernial orifice. The anatomical structure of the anterior abdominal wall is such that there are several “weak” places, which, due to the features of their structure, are predisposed to be hernial orifices. The most common hernial orifice is the inguinal ring (66% of hernias) and the adjacent area called the medial inguinal fossa. The contents of the hernial protrusion in this case may include the small intestine, omentum, occasionally the cecum, appendix, bladder, sigmoid colon, and internal female genital organs. Over time, the hernial sac descends into the scrotum in men, and into the labia majora in women. Inguinal hernias are divided into direct and oblique according to the location of the hernial canal.
Less common are femoral, umbilical hernias, and hernias of the white line of the abdomen.
In addition, the following types of hernias are distinguished: congenital and acquired, traumatic, postoperative; complete and incomplete, reducible and irreducible, complicated and uncomplicated.
Book a consultation 24 hours a day
+7+7+78
Diagnostics
To diagnose a paracolostomy hernia, it is enough for an experienced surgeon to perform a physical examination of the patient in a horizontal and vertical position. The doctor pays attention to the size and shape of the protrusion, the possibility of its independent reduction. A digital examination of the hernial orifice is performed. To clarify the diagnosis, instrumental methods are prescribed:
- X-ray examination. Radiography of the passage of barium through the intestines in dynamics is carried out to visualize the contents of the hernial sac and establish the anatomical relationships of the loops of the small intestine. On radiographs it is possible to detect signs of adhesions.
- Sonography. Ultrasound of a paracolostomy hernia is a quick and non-invasive way to visualize the organs that are inside the hernial sac. The technique helps to identify complications - the presence of an inflammatory process and exudate, adhesions between intestinal loops.
How do hernias develop?
As a rule, patients who develop hernias have certain characteristics of the physique and structure of connective tissue, which already loses its elasticity with age. The general name for these changes is “connective tissue weakness syndrome.” Modern studies have confirmed metabolic disorders of collagen, the main framework protein of connective tissue, in such patients.
Factors contributing to the clinical manifestation of a hernia are a decrease (hypotrophy) of the muscles of the anterior abdominal wall, an increase in intra-abdominal pressure with ascites, obesity, pregnancy, and intestinal dyskinesia. The occurrence of umbilical hernia in women is facilitated by multiple pregnancies and difficult childbirth. The holes and gaps between the muscles of the abdominal wall can increase with sudden weight loss.
Postoperative hernias occur at the site of a tissue defect, thinning of a postoperative scar, more often after various complications in the area of a postoperative suture (suppuration, infiltration, etc.). In patients with cancer, postoperative hernias can develop in later stages due to a sharp decrease in body weight, including the development of cancer cachexia.
Symptoms of paracolostomy hernia
According to the nature of the course, hernias can be asymptomatic or accompanied by clinical manifestations. An asymptomatic or low-symptomatic course is typical for small-sized formations that do not interfere with the passage of feces through the intestines. The leading symptom of paracolostomy protrusions of large diameter is pain. At first, painful attacks occur when changing body position, bending, and then become permanent.
Patients complain of a protrusion in the paracolostomy area, which hurts when pressed or rubbed by clothing. At the beginning, the hernia repairs itself into the abdominal cavity and disappears in the supine position. In the future, arbitrary or manual repositioning of organs becomes impossible. Characterized by a gradual increase in size of the formation. The skin over the hernia has normal color and temperature.
The pathognomonic manifestation of a paracolostomy hernia is a disturbance in the rhythm of bowel movements. In patients with colostomy, regular portioned bowel movements 2-3 times a day are established over time. With the development of hernial protrusion, the frequency of fecal excretion increases to 10-20 times a day, and the release of gases increases. Frequent bowel movements are replaced by prolonged constipation.
If there are stool problems, difficulties arise in using a colostomy bag, and with large protrusions this becomes almost impossible. Such problems put serious psychological pressure on a person: a patient with a paracolostomy hernia becomes irritable and anxious. Patients avoid contact with friends and family, which further aggravates neurotic reactions.
Why is hernia repair necessary?
In addition to the cosmetic defect and the discomfort caused by the hernia, there is a good reason not to put the operation on hold. This reason is the danger of infringement, i.e. sudden compression of the contents of the hernia in the hernial orifice. This usually happens after lifting something heavy, straining hard, or during a strong cough, i.e. with increased intra-abdominal pressure. Most often, the mobile small intestine is strangulated; in the strangulated part of the intestine, blood circulation is disrupted, which after a short time leads to necrosis of the intestine and even perforation (perforation) of its wall with the development of inflammation of the peritoneum (peritonitis) - a life-threatening condition.
Clinically, strangulated hernia is accompanied by a significant increase in hernial protrusion, its non-reduction, tension and severe pain. Pain can be localized only in the area of the hernia or spread over the entire surface of the anterior abdominal wall. The temperature rises, sometimes to a high level of 38-39'C. In some patients, blood pressure drops sharply with a decrease in the systole-diastolic interval, for example, to 80/60 mmHg. Some patients may vomit bile and even feces. Acute intestinal obstruction develops.
Treatment of paracolostomy hernia
Conservative therapy
It is possible to avoid surgical treatment for small paracolostomy hernias that do not manifest themselves clinically. An appropriate colostomy bag is selected for patients and the features of its use are explained in detail. Restriction of physical activity and a special diet to prevent constipation are recommended. Patients are subject to regular follow-up with a surgeon.
Surgery
The absolute indications for surgery are the presence of a large or giant paracolostomy hernia, clinical manifestations or complications. Surgeons determine the tactics of surgical intervention taking into account the general condition of the patient and the severity of the underlying disease for which the stoma was performed:
- Closing a temporary colostomy. During reconstructive surgery, the intestinal stoma is eliminated and the anatomical integrity of the intestine is restored. The intervention provides good long-term results and returns patients to a full life.
- Reconstructive surgery. Often in abdominal surgery they resort to hernioplasty of paracolostomy hernia using a mesh prosthesis, since such an operation has a minimal risk of relapse. Less commonly, excision of the hernial sac and reconstruction of the colostomy without plastic surgery are performed.
Tests to confirm the diagnosis
In uncomplicated cases of hernia, a standard preoperative examination is usually sufficient. The diagnosis is made during a routine clinical examination by a surgeon. In doubtful cases, the surgeon tries to insert a finger into the suspected hernial canal and asks the patient to strain or cough. At the same time, a push is felt, indicating the presence of a hernia. Carrying out an ultrasound examination of the patient in an upright position can detect thinning of the tissues of the anterior abdominal wall in the area of the hernial orifice.
In complicated cases, an ultrasound scan can reveal the corresponding organs in the hernial sac - the intestines, bladder and others.
In the presence of nausea, vomiting, pain and the absence of organ strangulation in the hernial orifice, other diseases with similar symptoms must be excluded. It happens that hernias of the white line of the abdomen accompany peptic ulcers, stomach cancer, cholecystitis, etc.
Classification
Based on the diameter of the hernia formation, they are divided into small (up to 10 cm), large (10-20 cm), and giant (more than 20 cm). In relation to a colostomy, protrusions are localized on one side of the removed intestine or have a ring arrangement around the stoma. Based on the anatomical features of the structure of the hernial sac, the English surgeon H.B. Delvin in 1983 proposed to distinguish 4 types of paracolostomy hernias:
- Interstitial. The hernial sac is localized between the muscles of the anterior abdominal wall. Such hernias are characterized by asymmetrical enlargement of the colostomy and cyanosis of the skin around it.
- Subcutaneous. The protrusion passes near the wall of the large intestine and is located at the level of the subcutaneous tissue. The muscle layers of the abdominal wall are not involved in the process.
- Intrastomal. With this complication, the movable organs of the abdomen penetrate into the outlet of the removed intestine, but do not protrude out through the colostomy.
- Transostomal. The rarest type of paracolostomy hernia is when the abdominal organs come out directly through the colostomy.
Contraindications for surgery
Acute infections, late pregnancy, dermatitis and eczema in the hernia area.
Since the herniotomy operation is performed under general anesthesia, the presence of decompensation of severe diseases of the internal organs, including coronary heart disease, stroke, diabetes, is a contraindication to the operation due to the high degree of anesthetic risk.
In cancer patients, a hernia of the anterior abdominal wall is treated according to the same principles as in other patients.
General information
Paracolostomy (parastomal) hernias are the most common complication after colostomy interventions. The anatomical feature of PCG is that one of the walls of the hernial sac is the wall of the excreted intestine. Depending on the surgical technique, pathological formations occur in 10-60% of patients. Hernias associated with colostomy develop 3 times more often than after ileostomy. The complication mainly occurs in people over 75 years of age, as well as those suffering from concomitant diabetes mellitus or cancer.
Paracolostomy hernia
Abdominal pain
Abdominal pain is a fairly common occurrence. It can be caused by many conditions - from mild gastritis to severe diseases.
I would like to dwell not on any specific disease, but on the general principles of approaching abdominal pain from the standpoint of surgery.
The primary goal of the surgeon is to determine whether the pain is caused by an acute surgical condition or whether the pain is a manifestation of a chronic or non-life-threatening condition.
Acute surgical diseases include conditions in which a person’s life is in immediate danger. Such diseases require emergency surgery or mandatory treatment and observation in a surgical hospital.
Acute surgical diseases include peritonitis (inflammation of the peritoneum), acute appendicitis, acute cholecystitis (inflammation of the gallbladder), acute pancreatitis (pancreatic necrosis) - inflammation of the pancreas), intestinal obstruction, perforated ulcer (as well as perforation of any hollow organ - intestine, etc. ), mesenteric thrombosis (blockage of intestinal arteries leading to intestinal necrosis), gastrointestinal bleeding, strangulated hernia and some others.
Publications in the media
Regarding the treatment of this disease, you can contact the Surgical Department No. 1 of the Clinic of Faculty Surgery named after. N.N. Burdenko
Abdominal hernias are divided into external and internal • External abdominal hernia is a surgical disease in which, through various openings in the muscular aponeurotic layer of the abdominal walls and pelvic floor, the viscera emerge along with the parietal layer of the peritoneum with the integrity of the skin • Internal abdominal hernia is formed inside the abdominal cavity in peritoneal pockets and folds or penetrates into the chest cavity through natural or acquired openings and slits of the diaphragm.
Frequency. Observed at any age. Peaks of incidence are preschool age and age after 50 years. It is registered more often in men.
Etiology • Congenital defects of the abdominal wall (for example, congenital indirect inguinal hernias) • Enlargement of the abdominal wall openings. Normally existing but pathologically enlarged openings in the abdominal wall can cause protrusion of internal organs (for example, the protrusion of the stomach into the chest cavity through the enlarged esophageal opening of the diaphragm during a hiatal hernia) • Thinning and loss of elasticity of tissues (especially against the background of general aging of the body or exhaustion) lead to the formation of inguinal, umbilical hernias and hernias of the white line of the abdomen • Trauma or wound (especially postoperative), when degenerative changes develop in normal tissues along the incision line, which often leads to the formation of postoperative ventral hernias. Suppuration of a postoperative wound increases the risk of hernia formation • Increased intra-abdominal pressure. Factors contributing to increased intra-abdominal pressure: heavy physical labor, cough in chronic lung diseases, difficulty urinating, prolonged constipation, pregnancy, ascites, abdominal tumors, flatulence, obesity.
Basic concepts. The type of hernia can be determined by objective examination or during surgery • Complete hernia. The hernial sac and its contents exit through a defect in the abdominal wall (for example, a complete inguinal hernia, when the hernial sac with its contents is in the scrotum [inguinoscrotal hernia]) • Incomplete hernia. There is a defect in the abdominal wall, but the hernial sac with its contents has not yet gone beyond the abdominal wall (for example, an incomplete inguinal hernia, when the hernial sac with its contents does not extend beyond the external inguinal ring) • Reducible hernia. The contents of the hernial sac easily move through the hernial orifice from the abdominal cavity to the hernial sac and back • Irreversible hernia. The contents of the hernial sac cannot be reduced through the hernial orifice due to the formed adhesions or large size of the hernia • Strangulated hernia - compression of the contents of the hernial sac in the hernial orifice • Congenital hernia is associated with developmental anomalies • Sliding hernia contains organs that are partially not covered by the peritoneum (cecum , bladder), the hernial sac may be absent • Richter’s hernia is a strangulated hernia of the abdomen. Its peculiarity: infringement of only part of the intestinal wall (without the mesentery). There is no intestinal obstruction (or it is partial) • Littre hernia is a hernia of the anterior abdominal wall containing a congenital diverticulum of the ileum.
Complications mainly arise from delays in seeking medical help and late diagnosis • Obstructive intestinal obstruction develops when a loop of intestine protrudes through a defect in the abdominal wall with the appearance of a mechanical obstacle to the passage of intestinal contents as a result of compression or bending of the intestine (the so-called fecal strangulation) • Strangulated intestinal obstruction with necrosis and perforation of the intestinal loop develops as a result of compression of the mesenteric vessels with impaired blood flow in the wall of the strangulated intestine (so-called elastic strangulation) • Isolated necrosis with perforation of the strangulated area of the intestinal wall with Richter's hernia.
Inguinal hernia
• Indirect inguinal hernia •• Passes through the deep inguinal ring into the inguinal canal. In some cases, it can descend into the scrotum (complete hernia, inguinal-scrotal hernia) •• With congenital inguinal hernias, the processus vaginalis of the peritoneum remains completely open and communicates with the abdominal cavity, inguinal canal and scrotum. Partially obliterated processus vaginalis of the peritoneum can cause hydrocele of the spermatic cord •• Prevalence. 80–90% of all types of abdominal hernias are inguinal. Among patients with inguinal hernias, 90–97% are men aged 50–60 years. In general, it occurs in 5% of men •• In children, there is a significant tendency to incarceration. In 75% of cases, a right-sided hernia is observed •• Can be combined with undescended testicle into the scrotum, its location in the inguinal canal, the development of hydrocele of the testicular membranes or the vaginal membrane of the spermatic cord •• Bilateral nonfusion of the processus vaginalis of the peritoneum is observed in more than 10% of patients with an indirect inguinal hernia .
• Direct inguinal hernia. The inferior epigastric artery and vein serve as an anatomical landmark for recognizing oblique and direct inguinal hernias. A direct inguinal hernia emerges from the abdominal cavity medially from the lateral umbilical fold •• Exits in the area of the bottom of the inguinal canal through Hesselbach’s triangle as a result of thinning and loss of elasticity of tissues •• Direct inguinal hernia is a direct exit of internal organs through the posterior wall of the inguinal canal posteriorly and medially from the spermatic cord; the hernia lies outside the elements of the spermatic cord (unlike an oblique inguinal hernia) and, as a rule, does not descend into the scrotum. The hernial orifice is rarely narrow, so a direct inguinal hernia (as opposed to an oblique one) is less likely to be strangulated •• The hernia is not congenital, it is more often observed in old age. In the elderly, it is often bilateral •• Recurrent hernias occur more often in patients with direct inguinal hernias than in patients with indirect inguinal hernias. Surgical treatment is aimed at strengthening the posterior wall of the inguinal canal.
• Combined inguinal hernias are classified as complex forms of inguinal hernias. The patient has 2 or 3 separate hernial sacs on one side, not communicating with each other, with independent hernial openings leading into the abdominal cavity.
• Femoral hernia exits through the femoral canal along the femoral fascia •• Prevalence - 5-8% of all abdominal hernias. Most patients (80%) are women aged 30–60 years •• Rarely large, prone to strangulation. The contents of the hernial sac are a loop of the small intestine, an omentum •• The appearance of hernias is usually associated with heavy physical exertion, chronic constipation and pregnancy.
• Diagnostics •• Patient complaints about a tumor-like protrusion in the groin area and pain of varying intensity (especially with physical stress) •• Objective examination ••• Examination. Pay attention to the shape and size of the hernial protrusion in the vertical and horizontal positions of the patient ••• Palpation. Determine the size of the hernial protrusion, the degree of reducibility, the size of the internal opening of the inguinal canal, the shape and size of the testicles ••• The symptom of a cough push is the jerk-like pressure of the hernial sac on the tip of a finger inserted into the inguinal canal when the patient coughs ••• Percussion and auscultation of the area of the hernial protrusion . Carry out to identify peristaltic noises and tympanic sound (if there is a loop of intestine in the hernial sac) •• Differential diagnosis: lipoma, inguinal lymphadenitis, abscess, orchiepididymitis, hydrocele of the testicular membranes, varicocele, cryptorchidism.
• Treatment •• The main stages of hernia repair: ••• Access to the inguinal canal ••• Isolation of the hernial sac, opening its lumen, assessment of the viability of the contents and its reduction into the abdominal cavity ••• Ligation of the neck of the hernial sac, its removal ••• Inguinal plastic surgery canal •• Features of hernia repair for oblique inguinal hernias: ••• Ligation of the hernial sac at the level of the parietal peritoneum ••• Suturing of the deep inguinal ring to normal sizes ••• Strengthening the anterior wall of the inguinal canal with mandatory suturing of the deep inguinal ring is used in young men with small indirect inguinal hernias. For sliding, recurrent and large inguinal hernias, the posterior wall of the inguinal canal is strengthened. For large defects of the abdominal wall, it is strengthened using various grafts. Strengthening the anterior wall of the inguinal canal. Girard's method: the internal oblique and transverse abdominal muscles are sutured to the inguinal ligament above the spermatic cord, and a duplicative aponeurosis of the external oblique abdominal muscle is created. Currently, various modifications of this operation are used - the Spasokukotsky method, the Kimbarovsky suture. Strengthening the posterior wall of the inguinal canal. Bassini's method: the edges of the internal oblique and transverse abdominal muscles, together with the transverse fascia, are sutured to the inguinal ligament under the spermatic cord, on top of which the edges of the previously dissected aponeurosis of the external oblique muscle are sutured. Alloplasty. Used for complex forms of inguinal hernias. Skin autografts, dura mater allografts, and synthetic materials are used. •• A feature of hernia repair for direct inguinal hernias is the strengthening of the posterior wall of the inguinal canal after reduction of the contents of the hernial sac. The Bassini method is used •• Hernia repair for femoral hernias can be performed using the femoral and inguinal methods ••• Femoral method. The femoral canal is approached from its external opening. Most surgeons use the method proposed in 1894 by Bassini. Access: parallel to and below the inguinal ligament above the hernial protrusion. The hernial orifice is closed by suturing the inguinal and pubic (Cooper) ligaments. The femoral canal is sutured with a second row of sutures between the edge of the lata fascia of the thigh and the pectineal fascia. Unfortunately, the Bassini operation leads to deformation of the inguinal canal and in some cases contributes to the occurrence of indirect inguinal hernias. Rudzhi's operation does not have this disadvantage ••• Inguinal method according to Rudzhi. The inguinal canal is opened with an incision above and parallel to the inguinal ligament and (after removal of the hernial sac) the hernial orifice is sutured with sutures connecting the inguinal and Cooper ligaments with the internal oblique and transverse muscles. In this way, the inguinal and femoral canals are simultaneously closed •• Relapses after surgical treatment - 3–5% •• Special situations ••• Incarceration of a section of the intestine followed by necrosis. If the diagnosis is established, laparotomy, revision of the abdominal cavity and resection of the nonviable segment of the intestine are performed. ••• Relapses and large defects of the abdominal wall. To eliminate the defect, synthetic prostheses are implanted ••• Children. Krasnobaev’s method is often used: after removing the hernial sac, 2 sutures are placed on the legs of the external opening of the inguinal canal. In this case, 2 folds of the aponeurosis of the external oblique muscle are formed. They are sewn together with several additional sutures ••• A hernia bandage is designed to prevent the exit of abdominal organs through the hernial orifice. It is used if there are contraindications to surgical treatment (concomitant somatic diseases) or if the patient refuses surgery •• Laparoscopic repair for inguinal and femoral hernias ••• Absolute indications: recurrent and bilateral hernias ••• Contraindications: organ strangulation or intestinal infarction within hernias ••• Approaches - intraperitoneal and extraperitoneal ••• Complications: damage to the external iliac vessels, damage to the ilioinguinal and femoral nerves, the formation of adhesions during intraperitoneal surgery can cause small intestinal obstruction.
Other types of abdominal hernia
• Umbilical hernia - exit of abdominal organs through a defect in the abdominal wall in the navel area •• In women, it is observed 2 times more often •• Most often observed in early childhood, in 5% of cases - in older children and adults. As it develops, self-healing is possible at the age of 6 months to 3 years •• Causes of umbilical hernia formation in adults: increased intra-abdominal pressure, ascites, pregnancy •• Umbilical hernia repair ••• In children: Lexer's operation. The umbilical ring is sutured with a purse-string suture ••• In adults: Mayo operation: the hernial orifice is closed with a duplicate of the aponeurosis sheets stitched one on top of the other. Sapezhko's method. First, the peritoneum is peeled off from the posterior surface of the vagina of one of the rectus abdominis muscles. Then, using separate sutures, grasping on one side the edge of the aponeurosis of the linea alba, and on the other hand, the posteromedial part of the rectus sheath, where the peritoneum is separated, a duplication is created from muscular aponeurotic flaps.
• Hernia of the linea alba can be supra-umbilical, peri-umbilical and sub-umbilical •• More often observed in men (3:1). In children they are extremely rare •• Hernias can be multiple •• Plastic surgery by simply suturing the defect in the aponeurosis gives about 10% of relapses. For large hernias, the Sapezhko method is used.
• Postoperative ventral hernia is the most commonly observed type of ventral hernia, resulting from complications during the healing of a postoperative wound •• Predisposing factors: wound infection, hematoma, old age, obesity, high pressure in the abdominal cavity with intestinal obstruction, ascites, pulmonary complications of the postoperative period •• Surgical treatment is performed after eliminating the causes that determined their development.
• A hernia of the semilunar (Spigelian) line is usually located at its intersection with the line of Douglas. Treatment is surgical. For small hernias, the gate is closed in layers by applying sutures. For large hernias, after suturing the muscles, it is necessary to create a duplicative aponeurosis.
ICD-10 • K40 Inguinal hernia • K41 Femoral hernia • K42 Umbilical hernia • K43 Hernia of the anterior abdominal wall • K44 Diaphragmatic hernia • K45 Other abdominal hernias • K46 Abdominal hernia, unspecified
Profitable arithmetic: two operations in one
Cholecystectomy
- Cost: 100,000 - 160,000 rubles.
- Duration: 25-30 minutes
- Hospitalization: 3 days in hospital
More details
We consider performing two or more operations simultaneously for combined surgical diseases as another interesting area of work. There are not so few people suffering from several diseases at once that require surgery. Traditionally, they endure one operation after another, trying to gradually get rid of their ailments. The use of gentle laparoscopic techniques allows you to solve the problem in one step. Our department has accumulated extensive experience when laparoscopic hernioplasty was performed in conjunction with removal of the gallbladder for cholelithiasis, colon resection, gynecological operations, etc. Despite the expansion of the volume, patients tolerate these interventions well, are activated early and are discharged from the hospital in almost the same time frame as after one operation. At the same time, the patient avoids repeated intervention with all the ensuing difficulties and dangers, saving time, effort and money.
What to do if you have abdominal pain?
It is important to note that only a doctor can assess the patient’s condition and make a diagnosis. The presence of the above symptoms does not always indicate a severe acute abdominal disease, just as their absence does not guarantee the exclusion of such a disease.
If abdominal pain appears , and especially with the presence of “alarming” symptoms, you need to call “03” . The doctor who arrives on call will determine whether an acute surgical disease can be suspected, and if it cannot be ruled out, he will hospitalize the patient. Before being examined by a doctor, it is prohibited to take painkillers, which can erase the clinical picture - relieve pain, reduce temperature, etc., creating the impression of imaginary well-being.
If, during the examination, the doctor excludes an acute surgical disease, as well as other diseases requiring hospitalization (food poisoning, severe influenza, acute hepatitis, renal colic, myocardial infarction, acute gynecological diseases, etc.), he prescribes treatment or recommends contacting a specialized specialist - gastroenterologist, therapist.
In addition to acute surgical diseases, abdominal pain can be caused by many other diseases - gastritis, exacerbation of peptic ulcer disease, chronic cholecystitis, chronic pancreatitis, intestinal colic, irritable bowel syndrome, neuralgia, oncological processes, gynecology and many others. They are treated by therapists, gastroenterologists, neurologists, gynecologists, urologists, etc.
Belly patch or new techniques
In recent years, techniques have begun to be used to avoid tissue tension. During the operation, special meshes are inserted through the incision in the projection of the hernial ring to hold the exit of the hernial sac through the aponeurosis defect. The meaning of the action is clear: if a child wipes his pants, then the housewife does not sew up the hole, but sews in a patch. The comparison may be curious for such a serious topic, but it conveys the main idea embedded in the methodology. It should be noted that all “open” operations involve, first of all, an incision, the associated pain syndrome, the danger of inflammation of the suture and, finally, rough scars on the skin. Therefore, in hernia surgery, the search for new operations that would combine not only reliability, but also low trauma does not stop.
Scrotal hernia: causes
A scrotal hernia in a child is caused by pathological development of the fetus. In the womb, the testicles descend into the scrotum through the inguinal canal, which soon closes. If it does not close, a scrotal hernia forms. Scrotal hernia most often occurs in premature babies because they have weak muscles, and as a result, tears can form in thinner areas of the abdominal wall.
Scrotal hernia can also occur in adults. More often, the pathology occurs in men who are overweight and have problems with urination (for example, due to an enlarged prostate). Men with chronic constipation and pulmonary embolism also tend to develop a scrotal hernia.