The text is presented for informational purposes only. We strongly urge you not to self-medicate. When the first symptoms appear, consult a doctor. We recommend reading: “Why you can’t self-medicate?”
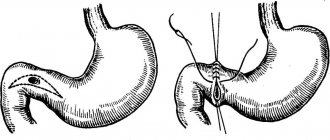
Jejunitis is a polyetiological disease of the jejunum, which is characterized by the development of inflammatory-dystrophic processes, atrophy of the mucous membrane, and impaired absorption and digestive functions.
As an independent disease, jeunitis is extremely rare and causes difficulties in diagnosis. Typically, inflammation of the jejunum is combined with damage to the ileum and duodenum, which is included in the general concept of “enteritis.”
Medical products (drugs, medicines, vitamins, dietary supplements) are mentioned for informational purposes only. We strongly do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?”
Total information
Inflammatory damage to the mucous membrane of the jejunum rarely manifests itself as a separate pathology. Often, jejunitis is associated with other pathologies of the gastrointestinal tract and in some cases, due to their symptoms, may go unnoticed. Difficulties in diagnosing jejunitis are one of the problems in treating patients suffering from this disease. Because of this, the patient is often mistakenly diagnosed with lactase deficiency (lack of the enzyme lactase, which digests milk sugar (lactose)) or celiac disease (congenital intolerance to the gluten protein contained in cereals - wheat, rye, barley). The result is improper treatment, progression of the inflammatory process in the mucous membrane of the jejunum and the occurrence of complications.
Together with the jejunum, the following are most often involved in the process:
- stomach;
- duodenum;
- ileum.
Eunit - what is it?
Jejunitis is a fairly rare disease accompanied by inflammation in the jejunum of the intestine. Clinical pathology usually does not manifest itself as an independent disease, but is combined with inflammation of other parts of the human intestinal system. The histology of jeunitis is characterized by swelling and shortening of the villi of the mucous lining of the jejunum, smoothness of epithelial cells, followed by their atrophy against the background of inflammatory signs. All these factors are accompanied by impaired absorption and digestion of food, and the manifestation of secondary immune and metabolic disorders.
Read also: Foods that most often cause heartburn
The clinical diagnosis of jejunitis is very difficult to determine, since there are no obvious symptomatic signs of the disease, which often leads to diagnostic error. Effective treatment of jeunitis is possible only after a high-quality diagnostic examination, including magnetic resonance and computed tomography, ultrasound scanning and other high-tech methods of instrumental research.
Causes and mechanisms of development
There are many reasons that provoke inflammatory damage to the jejunal mucosa. The peculiarity is that some causes cause acute inflammation of the mucous membrane, while others cause chronic inflammation. Based on this criterion, the factors that provoke jeunitis were systematized into two groups.
Acute inflammation occurs due to the introduction of an infectious agent into the mucous membrane of the jejunum. These are mainly pathogens such as:
- salmonella;
- Vibrio cholerae;
- paratyphoid pathogens
and others.
Also, a provocative factor in the occurrence of acute jeunitis can be:
- pronounced desensitization (increased sensitivity of the body) and, as a result, an allergic reaction to a foreign agent;
- some food products - mushrooms, jam with seeds, spices and hot seasonings, as well as alcoholic drinks.
Please note
One form of jeunitis is the so-called Whipple's disease. This is an infectious lesion of the mucous membrane of the jejunum, accompanied by fatty degeneration (replacement of cells with adipose tissue).
Several mechanisms play a role in the development of chronic inflammation of the jejunal mucosa:
- nutritional (food);
- toxic;
- thermal;
- immune;
- radiation.
In chronic jejunitis, pathological microorganisms are also found in the mucous membrane and lumen of the jejunum. But it turned out that they are not the impetus for the occurrence of the inflammatory process, but begin to act destructively on the mucous membrane of the jejunum only when exposed to additional factors that damage the mucous membrane of the jejunum. Meaning:
- food poisoning;
- toxic effects;
- action of high temperatures;
- impaired immunity;
- ionizing radiation.
The toxic factors that most often provoke jeunitis are poisoning with lead or phosphorus compounds.
Whipple's disease occurs due to damage to the immune system, but the provoking factor (a kind of “trigger”) is bacteria. The disease develops as follows. The irritating factor affects the mucous membrane that lines the jejunum. Because of this, its enzymatic activity is disrupted. As a result, the nutrients that enter the intestine are not absorbed - chemical compounds formed during the preliminary breakdown of food.
note
Nutrients actively bind water molecules, resulting in fluid accumulation in the lumen of the jejunum and, as a result, intraintestinal pressure increases.
Jejunitis is a classic inflammation. The mucous membrane of the jejunum and, in particular, its villi are affected, due to the insufficiency of which the digestion process is disrupted . A role is also played by the fact that food breakdown products accumulate in the intestinal lumen, which begin to ferment and, being absorbed into the blood, provoke poisoning of the body.
Important
Due to the difference in causative factors and mechanisms of occurrence, the symptoms and course of acute and chronic jeunitis differ.
Traditional methods
During the treatment of the chronic form of jejunitis, the use of decoctions of medicinal plants is quite effective. Healing herbs can have a calming effect on the gastrointestinal tract, replenish the body with biologically active substances (essential oils, organic acids, vitamins, etc.), increase the patient’s immunity and general vitality.
The following recipes have proven themselves to be the best for folk treatment of jeunitis:
- Mint decoction. The soothing medicine is prepared as follows: 10 g of dry leaves must be placed in a teapot and filled with boiling water (200 ml). After 15-20 minutes, the decoction can be drunk as regular tea, 1 cup 2-3 times a day before meals.
- Chamomile decoction. To prepare a soothing, wound-healing decoction, it is most effective to use flowers: 25 g of dry raw materials should be placed in a glass jar with a capacity of 0.5 liters, fill it to the top with boiling water, close the lid and let it brew for 35-40 minutes. After straining through gauze, the healing composition can be drunk 150 ml three times a day on the eve of food intake.
It should be borne in mind that some components of medicinal plants can cause allergic reactions and provoke an exacerbation of the disease. For this reason, it is recommended to consult a doctor before starting to use decoctions.
Diagnostics
The signs of jeunitis are quite pronounced. But the problem of diagnosis is that it often occurs against the background of other diseases, so doctors may not suspect an inflammatory lesion of the jejunal mucosa. Therefore, in addition to asking the patient about complaints, it is necessary to study the medical history and conduct additional research - physical (examination, palpation, tapping and listening to the abdomen with a phonendoscope), instrumental and laboratory.
Important
One hundred percent confirmation of jeunitis can be obtained only after a histological examination of sections of the intestine - only thanks to this it is possible to 100% exclude diseases similar in their course to jeunitis (for example, enzymopathies - diseases due to impaired activity of food enzymes, accompanied by fermentation in the intestines).
If “fresh” acute jejunitis is diagnosed, the patient’s general appearance may not be affected. Sometimes there is pallor of the skin and visible mucous membranes.
With a chronic ongoing course, noticeable:
- general emaciation and exhaustion of the patient;
- sagging skin;
- coating of the tongue with a white coating;
- sometimes - trembling of the hands.
When palpating the abdomen, it is determined to be painful in the upper sections, but the abdomen is soft. The skin of the abdomen is inelastic and flabby to the touch, the same is revealed if you feel the skin of other parts of the body.
The following signs are characteristic when palpating:
- Porges symptom – severe pain when pressing on the anterior abdominal wall above the navel on the left;
- Sternberg's symptom - severe pain on deep palpation above the navel (when pressing on the mesentery of the organ - the connective tissue film that attaches the jejunum from the inside in the anterior abdominal wall).
Tapping the abdomen does not reveal any special signs, but auscultation during flatulence may weaken bowel sounds with sharp spasmodic “bursts” (loud rumbling).
Since jeunitis is difficult to diagnose, it is necessary to use all possible non-physical examination methods to clarify the picture.
The instrumental methods used in the diagnosis of jejunitis are as follows:
esophagogastroduodenoscopy (EFGDS) - using an endoscope (probe with built-in optics) to study the mucous membrane of the jejunum. EGDS is partially informative, since the technical capabilities allow the probe to be inserted only into the initial parts of the jejunum. With jejunitis, multiple areas of inflammation are detected during EGD;- passage of barium to the small intestine - the patient drinks a portion of barium suspension, then using radiography, the passage of barium through the small intestine is studied. When jejunitis, the passage of barium through the jejunum is accelerated.
They also conduct a series of examinations that will not demonstrate changes in the jejunum, but can identify disorders in other organs similar to manifestations of jeunitis. This is important for distinguishing jeunitis from other diseases. In particular, they apply:
- plain radiography of the abdominal organs;
- computed tomography (CT);
- magnetic resonance imaging (MRI);
- Ultrasound examination of the abdominal organs (ultrasound)
and other methods.
Laboratory research methods that are used in the diagnosis of jeunitis are:
general blood test - there is a slight increase in the number of leukocytes and ESR. These indicators are closely related to the intensity of the process: the stronger the inflammation, the greater the number and higher the ESR;- bacterioscopic analysis - it is carried out to identify the pathogen that caused the inflammatory process in the jejunal mucosa. To do this, the patient’s vomit or feces are examined under a microscope;
- bacteriological analysis - if the manifestations of the disease are not too pronounced, and doctors have time for a more thorough diagnosis without compromising the patient’s condition, the intestinal contents are cultured on nutrient media, and the pathogen is determined from the grown colonies;
- immunological study – necessary to assess the level of immunity that is involved in the body’s fight against jeunitis. This is the fight against infectious pathogens and allergic manifestations;
- examination of a biopsy specimen of the jejunal mucosa is the final diagnostic method for jejunitis. When studying the material, signs of inflammation, a decrease in the length of the villi and tissue swelling are determined.
In addition to instrumental and laboratory research methods, consultation with an infectious disease specialist will be required to rule out acute food poisoning.
Classification
By etiology
1. Primary:
- infectious;
- toxic;
- parasitic;
- allergic;
- medicinal;
- radial;
- nutritional;
- postoperative;
- congenital intestinal anomalies and fermentopathy;
- with insufficiency of the duodenal papilla.
2. Secondary (occurs against the background of other diseases).
By the nature of morphological changes
- without atrophy;
- with moderate partial villous atrophy;
- with subtotal villous atrophy.
According to the clinical course
In relation to chronic jeunitis:
- mild course;
- moderate course;
- severe course.
Treatment
Often, treatment begins before a comprehensive examination of the patient is completed. This is explained as follows:
- due to severe dehydration of the body, it should be flooded as early as possible, regardless of the diagnosis;
- treatment for jejunitis is similar to treatment for gastritis, so the doctor will not make a mistake with the prescriptions even before the final diagnosis;
- In 70% of cases, jeunitis and gastritis occur simultaneously, which is why early appointments are advisable if gastritis is diagnosed, and jeunitis is only suspected and examination of the patient continues.
Important
If there are signs of acute or exacerbation of chronic jeunitis, the patient is hospitalized in the infectious diseases department, since in some cases the disease is similar to acute food poisoning. The chronic form of the disease can be treated at home.
Jejunitis is treated with conservative methods. The therapy is based on the following purposes:
semi-bed rest (as much as frequent diarrhea allows);- diet;
- massive infusion therapy;
- antibiotic therapy;
- enterosorbents;
- antispasmodics;
- probiotics;
- prebiotics;
- enzyme preparations;
- desensitizing drugs;
- vitamin therapy.
The basis of therapy is the rapid replenishment of fluid and nutrient losses. It can also be carried out by the enteral route - the patient must drink a lot of fluid (on average 1.5 times more than he loses).
But in practice, the use of this technique is often impossible due to severe vomiting in the patient. Therefore, massive infusion therapy is carried out - intravenous drip administration of drugs such as:
- preparations of protein and protein fractions;
- saline solutions and electrolytes;
- glucose;
- blood serum.
In case of severe vomiting, fasting is recommended. As soon as the acute manifestations (in particular, dyspeptic symptoms - nausea, vomiting, diarrhea) subside, the patient can eat. The basis of the diet:
- fractional frequent meals with small portions;
- food should be liquid or crushed, warm, high in calories and with a sufficient amount of vitamins;
- food should not contain foods that are difficult to digest and irritate the intestines - spices, fats, fiber, and so on.
Antibiotics are prescribed to which microorganisms identified during bacteriological examination are sensitive.
Enterosorbents are prescribed to stop fermentation processes in the intestines and eliminate intoxication
Antispasmodics are used for severe pain.
Probiotics are a suspension of normal microflora. Prebiotics are drugs that stimulate the development of one’s own microflora. Both drugs, as well as enzymatic agents, are prescribed to improve digestion.
Symptoms
In this case, the chronic and acute forms of the disease may have their own specific symptoms, which complement the general clinical picture of this gastroenterological pathology. Common symptoms include:
- a feeling of pain and discomfort in the abdominal area, discomfort may intensify after eating;
- signs of general intoxication of the body;
- loose stool.
Since such a clinical picture is almost identical to ordinary food poisoning, in most cases patients do not seek medical help in a timely manner, and adequate treatment of the pathology does not begin in a timely manner.
The acute form of jejunitis is manifested by the following symptoms:
- intense pain in the abdomen, which can be present even at rest;
- feeling of constant thirst;
- dry skin;
- decreased turgor;
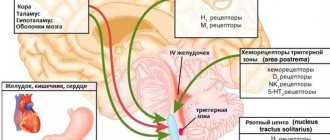
- nausea, sometimes with vomiting;
- bouts of diarrhea;
- increased body temperature;
- weakness, increased fatigue for no apparent reason.
In some cases, against the background of dehydration, vascular insufficiency may develop.
The chronic form of the disease is characterized by the following symptoms:
- flatulence;
- rumbling in the stomach;
- cramping, dull pain in the abdomen;
- bouts of diarrhea;
- symptoms of dysbacteriosis.
If you have the above clinical manifestations, you should consult a doctor and not self-medicate. Otherwise, not only complications may develop, but also the transition of the acute form of the disease to chronic, which complicates treatment.
Prevention
In order not to provoke the development of eunitis, it is enough to adhere to fairly simple rules:
maintain a diet;- adhere to the rules of sanitation and hygiene - in particular, thoroughly wash vegetables and fruits before eating them, follow the rules of heat treatment of products;
- do not eat spicy, rough and fibrous foods;
- do not ignore liquid warm dishes (soups);
- Be wary of foods that may provoke jejunitis - mushrooms, jam with seeds, etc., as well as alcohol.
If a chronic process has developed, then vigilance must be doubled so as not to provoke an exacerbation of the process.
Nutrition
For jejunitis, it is recommended to adhere to diet No. 4 according to Pevzner; depending on the activity of the inflammatory process and the phase of the disease, modifications of the main diet are used (4a, 4b, 4c).
Not recommended dishes:
- baked goods, brown bread;
- strong broths, vegetable broths;
- fatty meats and fish, sausages, smoked meats, pieces of meat, canned food;
- wheat, pearl barley porridge, pasta, all types of legumes, milk porridges;
- eggs, hard-boiled, fried;
- any raw vegetables and fruits;
- milk, sour cream;
- sauces, spices, snacks;
- alcoholic drinks.
Recommended dishes:
- dried white bread, crackers, savory cookies;
- slimy soups with the addition of pureed meat, meatballs;
- steamed cutlets, soufflé, meatballs made from lean meat and fish;
- pureed dairy-free porridge (rice, semolina, oatmeal, buckwheat);
- eggs in dishes, steam omelet;
- jelly, blueberry jelly, ripe pears, dogwood, quince, bird cherry, applesauce;
- freshly prepared mashed cottage cheese, pureed curd soufflé;
- tea with lemon and sugar, black coffee, blackcurrant juice, blueberries half and half with water, rosehip decoction, dried blackcurrants, blueberries, bird cherry.
Therapeutic nutrition involves limiting the diet of fats and carbohydrates, chemical and mechanical irritants of the mucous membrane. Small meals, 5-6 times a day. Dishes are served boiled or steamed.
Forecast
Despite the pronounced clinical picture, jejunitis responds well to treatment . Therefore, if treatment is started in advance (especially replenishment of fluid losses), the prognosis is favorable. Deterioration in nutrient absorption rarely develops at a moderate level.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
10,792 total views, 3 views today
( 48 votes, average: 4.46 out of 5)
Liver amyloidosis: causes, symptoms, treatment
Pancreatic stones: symptoms and treatment of pancreolithiasis