What is pancreatitis
Pancreatitis is inflammation of the pancreas. This organ secretes enzymes into the duodenum (just behind the stomach) that help food digest, such as amylase (to break down carbohydrates) and lipase (to break down fats). With severe inflammation of the pancreas - acute pancreatitis - its cells are destroyed and enzymes enter the blood. Therefore, for any severe abdominal pain, doctors determine the level of amylase in the blood.
Acute pancreatitis is a painful and very dangerous disease. Its symptoms are almost impossible to endure “on your feet”: it is a severe, persistent pain in the pit of the stomach and under the left rib, which often radiates to the back (so-called girdling pain occurs). A person with acute pancreatitis often even takes a special position on the bed - lying on his left side, so as not to increase the pain by moving the ribs when breathing. Most people with acute pancreatitis experience severe nausea and vomiting; any food intake increases the pain: after all, the pancreas begins to secrete enzymes when eating, and this increases blood flow, and therefore pain. Many people's body temperature rises.
Diagnosis of acute pancreatitis is the job not so much of gastroenterologists as of surgeons, since the intensity of pain can be the same as with appendicitis and other “surgical” pathologies.
Organ transplant success
A relatively new word in surgery for pancreatic health is transplantation. It was first produced in 1967. But even then, scientists knew that it would be possible to change organs only together with the accompanying duodenum.
Despite the fact that after a kind of exchange it is possible to live with other internal organs for quite a long time, how long they live after such a transplant is not particularly encouraging. In official medicine, the longest life expectancy after a successful outcome was just over three years.
Due to the too high risks for the patient, as well as the high threshold of complexity, this transplant is not in significant demand, even if the victim has been diagnosed with a malignant tumor.
The difficulty ends with the fact that the gland is a hypersensitive component of the abdominal cavity. Even with a gentle touch with a finger, she receives significant injuries. If we add to this the need to suture a huge number of accompanying large and small vessels, then the manipulation turns into a many-hour ordeal for all medical personnel and the patient.
The search for a donor is also not particularly smooth, since this organ is classified as unpaired, which means it can only be taken from a deceased person. He must not only meet all the criteria, but also give prior permission for the use of his organs for those in need.
But even if you manage to get such a donor, the required part of the peritoneum must be delivered extremely quickly. The gland is sensitive to a lack of oxygen, and also begins irreversible processes half an hour after the cessation of stable blood flow.
This means that even after careful removal from the previous owner in freezing mode, it will survive no more than five hours. This is unlikely to be enough to organize transportation even between neighboring transplant centers, and if you add time for the procedure itself, it becomes completely difficult.
If the victim was lucky and the organ was delivered as soon as possible, then the algorithm for identifying it includes:
- placement in the peritoneum;
- connection with hepatic vessels;
- comparison with the splenic and iliac vessels.
This is difficult to implement from the technical side of the issue, and is also accompanied by a high chance of death due to extensive bleeding and subsequent shock.
How does acute pancreatitis occur?
About 70% of all cases of acute pancreatitis are due to either alcohol poisoning or gallstones. Excessive alcohol consumption (even without a history of alcoholism) causes inflammation of the pancreas. For the same reason, people who systematically abuse alcohol have every chance of not only ending up in the hospital with severe acute pancreatitis, but also experiencing pain attacks again for many years. A gallstone can also cause pancreatitis: the duct that carries bile from the bladder into the duodenum merges with the pancreatic duct. This situation - biliary pancreatitis - requires emergency intervention, for example, to dissect the large duodenal papilla: this is the place where the ducts flow into the intestine.
Acute pancreatitis can also be caused by the toxic effects of certain medications, trauma to the gland during surgery, or high levels of fat in the blood. It is extremely rare and, as a rule, in the presence of other similar diseases, the pancreas becomes inflamed due to the excessive action of the immune system on it.
Whatever the cause of the onset of the disease, acute pancreatitis is always accompanied by abdominal pain. You should not assume this diagnosis if you feel unwell from a medicine or some product.
Prevention
Primary prevention of acute pancreatitis is to follow the rules of a healthy lifestyle. The diet should contain a minimum amount of fatty, fried and spicy foods (it is recommended to completely avoid such foods). Smoking and drinking alcoholic beverages increase the risk of digestive system diseases. An attack of acute pancreatitis is provoked by the listed factors. These rules apply not only to primary, but also to secondary prevention of pathology.
Prevention measures:
- compliance with the rules of a healthy diet (harmful foods, overeating and irregular food consumption are excluded);
- the body must receive sufficient physical activity (if work activity involves a sedentary lifestyle, then it is recommended to do basic exercises in the morning);
- weight control (sudden weight loss, excess weight can cause abnormalities in the functioning of the digestive system);
- timely diagnosis and treatment of any symptoms of digestive tract dysfunction (if gastrointestinal diseases are identified, then examinations by a gastroenterologist should be carried out at least once every six months);
- eliminating alcohol abuse, smoking and other bad habits.
Acute pancreatitis has been dealt with. What about chronic?
If the toxic effect on the pancreas does not stop (for example, a person continues to drink excessively) or the organ was very damaged during the first (acute) episode of pancreatitis, the pain returns again and again.
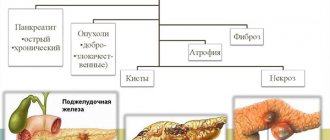
During exacerbations of chronic pancreatitis, blood tests may remain normal. But over time, external signs may appear, which doctors detect by examining the pancreas using ultrasound (ultrasound), X-rays (CT or computed tomography) or magnetic resonance imaging (MRI). These are narrowing of the pancreatic ducts, the appearance of compactions in it - calcifications, as well as the appearance of cysts - bubbles with liquid in place of dead tissue. An examination for suspected chronic pancreatitis is carried out with another important goal - not to miss pancreatic cancer, which may initially be accompanied by the same symptoms.
With constantly renewed inflammation of the pancreas, its function—the secretion of enzymes that digest food—is disrupted over time. As a result, a person is bothered by constant bloating, diarrhea, and the stool becomes greasy (for example, it is difficult to flush from the toilet). This condition - exocrine insufficiency - is most conveniently identified by determining the content of pancreatic elastase (a pancreatic enzyme) in the stool.
Consequences and complications
During the inflammatory process, there is a risk of infection of pancreatic tissue with pathogenic bacteria. The consequence of their vital activity will be necrosis of pancreatic tissue and the formation of abscesses. A state of shock can be an addition to the inflammatory process. The combination of such complications in the absence of adequate therapy poses a threat to the patient's life.
Complications of chronic pancreatitis gradually develop; the list includes dangerous diseases.
Complications:
- pseudocysts;
- fibrous-purulent peritonitis;
- parapancreatic infiltrate;
- arrosive bleeding;
- septic shock;
- ascites (abdominal dropsy).
How to treat chronic pancreatitis
In general, the goal of treating chronic pancreatitis is to eliminate pain. Anti-inflammatory drugs, such as paracetamol, are used for this. Enzymes are often prescribed to people with chronic pancreatitis. Unfortunately, this does not always relieve pain. Previously, it was assumed that adding enzymes to food would reduce the load on the pancreas - it would not have to secrete its own enzymes. In reality, everything is not so simple: the secretory (excretory) activity of the gland depends on completely different substances - hormones, for example secretin. Their production is more influenced by the fat content of food and the regularity of its intake than by the content of drug enzymes in the intestine. Nevertheless, enzymes for chronic pancreatitis are necessarily prescribed (often for life) if there are signs of poor secretion of one’s own enzymes (bloating, loose stools). Enzymes are always drunk directly with food: “between spoons.” For the same reason, it is illiterate to prescribe taking enzymes “so many times a day.” It is more correct to warn a person with the disease that the drug should be carried with them and taken with any food intake.
A diet for chronic pancreatitis alleviates the course of the disease, although it is difficult to accurately determine the list of possible products the first time. You definitely shouldn't drink alcohol, but traditionally it is recommended to eat less fatty foods and snack more often, giving preference to slow carbohydrates - fruits and vegetables. Cooking exclusively by steaming is not the most proven way to alleviate pancreatitis; it is much more important not to overindulge in very spicy foods. Roughly speaking, there will most likely be no harm from a chicken cutlet, even fried without much seasoning.
The main thing in the treatment of chronic pancreatitis is to remove the cause of the disease.
If a person suffers from alcoholism or smokes, refer him to a narcologist (smoking itself does not cause pancreatitis, but increases exacerbations). If pancreatitis occurs due to gallstones, remove the bladder. If fat metabolism is disturbed in the body, consult a cardiologist and select treatment with drugs that reduce the level of lipoproteins and triglycerides, and select a diet.
What surgery is indicated for abscesses?
If a person has been confirmed to have an abscess, then sending him to the operating room cannot be delayed. Especially when the abscess was a direct consequence of limited necrosis after exposure to an infectious pathogen. Sometimes the provocateur of the deviation is a long-term period of suppuration of the pseudocyst.
People usually ask what can be done in such a serious situation, other than surgery, but without an autopsy with drainage, a person’s life is unlikely to be saved. Depending on the affected area, it will depend on which technology the gastroenterologist will prefer:
- open;
- laparoscopic;
- internal.
The first combination is based on laparotomy, which involves opening the abscess with drainage of its cavity until the area is completely cleared.
When a verdict is made in favor of laparoscopic drainage, a laparoscope is required, with the help of which the problem point is opened carefully. Next, the expert removes non-viable tissue and installs channels for proper drainage to function.
A difficult and at the same time productive technique is internal drainage, the difficulty of which lies in opening the abscess through intervention through the posterior wall of the stomach. For a successful outcome, laparotomy or laparoscopic access is used.
The result is presented in the form of the release of malicious content through an artificially created fistula. Over time, the cyst becomes obliterated, and the fistula opening closes.