Colon
Colon
(lat.
intestinum crassum
) - the lower section of the gastrointestinal tract, starting after the small intestine and ending with the anus. Together with the small intestine it makes up the intestine.
Colon Anatomy
There are three sections in the large intestine: the cecum (No. 6 in the figure on the right; lat. caecum
) with the vermiform appendix (No. 8), the colon (Latin
colon
) with four subsections (ascending colon, transverse colon, descending colon (No. 7 ) and sigmoid colon) and rectum (No. 9; lat.
rectum
) with a wide part - the ampulla of the rectum and a terminal tapering part - the anal canal (No. 10), ending in the anus. The length of the colon in an adult is on average 160 cm, the internal diameter is on average 5 to 8 cm and decreases in the direction from the cecum to the rectum. The thickness of the wall of the colon is 2–3 mm, during contraction it is 4–5 mm, the thickness of the wall of the rectum is 2.4–8 mm. The large intestine is separated from the small intestine by the ileocecal valve.
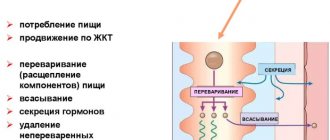
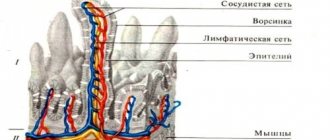
In the colon, the bulk of water, electrolytes, glucose, vitamins and amino acids produced by symbiotic bacteria are absorbed and feces are formed from chyme, as well as the accumulation and retention of the latter until it is excreted.
The most numerous endocrine cells of the intestine are located in the mucous membrane of the colon - L-cells, which produce the hormones enteroglucagon (glucagon-like peptide-1) and peptide YY.
The normal residence time of the contents (chyme and feces) in the large intestine is about 26 hours.
Acidity in the lower colon
I.A. Churkin studied the acidity in the lower parts of the colon in healthy people using endoscopic pH-metry. He found that the average acidity value for the entire rectum is 8.1 pH, for the sigmoid intestine - 8.1 pH, and also determined the following average acidity values for the lower parts of the colon (in pH):
- lower ampullary rectum: pH=7.3 (item 1 in the figure on the right)
- mid-ampullary rectum: pH=7.7 (position 2)
- upper ampullary rectum: pH=8.5 (position 3)
- supramullary rectum: pH=8.7 (position 4)
- distal third of the sigmoid colon: pH=8.7 (position 5)
- middle third of the sigmoid colon: pH=7.9 (position 6)
- proximal third of the sigmoid colon: pH=7.9 (position 7)
Colon microbiota
The large intestine, to a much greater extent than the small intestine, is populated by various microorganisms, the number of species of which approaches 500. In the large intestine, microorganisms make up 30% of the dry mass of the luminal contents.
The most common and physiologically significant are anaerobes: bifidobacteria, lactobacilli, bacteroides, veillonella, fusobacteria, eubacteria, peptostreptococci, clostridia and aerobes and conditional anaerobes: Escherichia coli, lactose-negative enterobacteria (Enterobacter, Citrobacter, etc.), Proteus, Enterococcus ki, klebsiella , staphylococci, yeast-like fungi. The number of microorganisms increases towards the distal parts of the colon, more in the luminal rather than in the parietal zones (Dobrovolsky O.V., Serebrova S.Yu.). Qualitative and quantitative composition of the main microflora of the colon in a healthy person in colony-forming units (CFU) in terms of 1 g of feces (according to OST 91500.11.0004-2003 “Protocol for the management of patients. Intestinal dysbiosis”):
| Types of microorganisms | Age, years | ||
| less than 1 | 1–60 | more than 60 | |
| Bifidobacterium ( Bifidobacterium ) | 1010–1011 | 109–1010 | 108–109 |
| Lactobacilli ( Lactobacillus ) | 106–107 | 107–108 | 106–107 |
| Bacteroides _ _ | 107–108 | 109–1010 | 1010–1011 |
| Enterococci ( Enterococcus ) | 105–107 | 105–108 | 106– 07 |
| Fusobacterium ( Fusobacterium ) | <106 | 108–109 | 108–109 |
| Eubacterium ( Eubacterium ) | 106–107 | 109–1010 | 109–1010 |
| Peptostreptococcus ( Peptostreptococcus ) | <105 | 109–1010 | 1010 |
| Clostridia ( Clostridium ) | ⩽103 | ⩽105 | ⩽106 |
| E. coli ( Escherichia coli ) typical | 107–108 | 107–108 | 107–108 |
| Lactose-negative E. coli | <105 | <105 | <105 |
| Hemolytic Escherichia coli | 0 | 0 | 0 |
| Other opportunistic bacteria: Klebsiella , Enterobacter , Hafnia , Serratia, Proteus , Morganella , Providencia , Citrobacter and others | <104 | <104 | <104 |
| Staphylococcus aureus (S taphylococcus aureus ) | 0 | 0 | 0 |
| Staphylococcus saprophyticus ( Staphylococcus saprophyticus ) and epidermal ( Staphylococcus epidermidis ) | ⩽104 | ⩽104 | ⩽104 |
| Yeast-like fungi of the genus Candida | ⩽103 | ⩽104 | ⩽104 |
| Non-fermenting bacteria: pseudomonas ( Pseudomonas ), acinetobacter ( Acinetobacter ) and others | ⩽103 | ⩽104 | ⩽104 |
In addition to those listed, bacteria of the following genera are present in the human colon in varying quantities: Actinomyces, Bacillus, Corynebacterium, Peptococcus, Acidaminococcus, Anaerovibrio, Butyrovibrio, Acetovibrio, Campylobacter, Disulfomonas, Propionibacterium, Roseburia, Ruminococcus, Selenomonas, Spirochetes, Succinomonas, Coprococcus
.
In addition to these groups of microorganisms, you can also find representatives of other anaerobic bacteria ( Gemiger, Anaerobiospirillum, Metanobrevibacter, Megasphaera, Bilophila
), various representatives of non-pathogenic protozoan genera (
Chilomastix, Endolimax, Entamoeba, Enteromonas
) and more than ten intestinal viruses (Ardatskaya M.D., Minushkin O.N.).
According to some data, approximately 1% of the total microbiota consists of the bacteria Christensenella minuta.
A decrease in the amount of
Faecalibacterium prausnitzii
in the normal microflora may be associated with Crohn's disease.
The figure above shows the species and quantitative composition of the dominant microflora of the human colon, obtained by the most modern method - using the analysis of the 16S rRNA gene (may vary in different populations, but not in a very significant way).
Slightly less than half of the total number of bacteria in the colon are bacteria of the following species: Faecalibacterium prausnitzii, Eubacterium rectale, Collinsella aerofaciens, [Clostridium] clostridioforme, Bacteroides vulgatus, Anaerostipes hadrus, Ruminococcus bromii, Eubacterium hallii, Blautia wexlerae, Bacteroides dorei, Roseburia faecis, Dorea longicatena, Subdoligranulum variabil, Bacteroides uniformis, Blautia obeum, Bacteroides ovatus, Blautia luti, Parabacteroides distasonis, Lachnospira pectinoschiza Dialister invisus, Roseburia inulinivorans, Ruminococcus callidus
.
Large intestine in children
A child's colon has a length equal to his height.
The sections of the large intestine are developed to varying degrees. The newborn has no omental processes, the bands of the colon are barely visible, and haustra are absent until six months of age. The anatomical structure of the colon after 3–4 years of age is the same as in an adult. The cecum, which has a funnel shape, is located higher, the younger the child. In a newborn it is located directly under the liver. The higher the cecum is located, the more underdeveloped the ascending colon is. The final formation of the cecum ends by the age of one year.
The appendix in a newborn has a cone-shaped shape, a wide open entrance and a length of 4–5 cm, by the end of 1 year - 7 cm. It has greater mobility due to the long mesentery and can be located in any part of the abdominal cavity, but most often occupies a retrocecal position.
The colon in the form of a rim surrounds the loops of the small intestine. The ascending part of the colon in a newborn is very short (2–9 cm), and begins to increase after a year.
The transverse part of the colon in a newborn is located in the epigastric region, has a horseshoe shape, length from 4 to 27 cm; by two years she is approaching a horizontal position.
The descending colon in newborns is narrower than the rest of the colon; its length doubles by 1 year, and by 5 years it reaches 15 cm. It is poorly mobile and rarely has a mesentery.
The sigmoid colon is the most mobile and relatively long part of the colon (12–29 cm). Until 5 years of age, it is usually located in the abdominal cavity due to an underdeveloped small pelvis, and then descends into the small pelvis. Its mobility is due to the long mesentery. By the age of 7, the intestine loses its mobility as a result of shortening of the mesentery and the accumulation of adipose tissue around it.
The rectum in children of the first months is relatively long and, when filled, can occupy the small pelvis. In a newborn, the ampulla of the rectum is poorly differentiated, the fatty tissue is not developed, as a result of which the ampulla is poorly fixed. The rectum reaches its final position by the age of two years. Due to the well-developed submucosal layer and weak fixation of the mucous membrane, young children often experience its loss.
The anus in children is located more dorsally than in adults, at a distance of 20 mm from the coccyx (Bokonbaeva S.D. et al.).
Large intestine in newborns
The colon in a newborn has an average length of 63 cm, and by the end of the first year of life - up to 83 cm. Subsequently, the length of the colon is approximately equal to the height of the child.
By birth, the colon has not completed its formation. The newborn does not have omental processes (they are formed in the 2nd year of the child’s life); the ribbons of the colon are barely outlined; colon haustra are absent (appear after 6 months). The bands of the colon, haustra and omental processes are finally formed by 6–7 years. The large intestine provides water resorption and evacuation-reservoir function. It completes the breakdown (both under the influence of enzymes coming from the small intestine and bacteria inhabiting the large intestine) and the absorption of nutrients, and the formation of feces occurs.
The mucous membrane of the colon in children is characterized by: deepened crypts, flatter epithelium, and a higher proliferation rate. Juice secretion in the colon is insignificant under normal conditions, but it increases sharply with mechanical irritation of the mucous membrane (Geppe N.A., Podchernyaeva N.S.).
Still from the video lecture “Large intestine in newborns” by E.V. Gostishcheva “Anatomical and physiological features of the digestive organs in children. Methods and methods for studying the digestive system in children" for students of the Medical Academy named after S.I. Georgievsky Crimean Federal University named after V.I. Vernadsky.
Some diseases and conditions of the colon
Certain colon (including rectal and anorectal) diseases and syndromes:
| Three stages of colon cancer |
- colon cancer
- functional dyspepsia, including dyspepsia in children
- irritable bowel syndrome
- irritable bowel syndrome with diarrhea
- irritable bowel syndrome without diarrhea
- pseudomembranous colitis
- Crohn's disease
- nonspecific ulcerative colitis
- enterocolitis
Symptoms and conditions that may be associated with diseases of the colon (including the rectum):
- stomach ache
- nausea
- vomit
- constipation, including constipation in children
- dyschezia
- flatulence
- diarrhea (diarrhea), including diarrhea (diarrhea) in children
- anismus
- gastrocolic syndrome
- encopresis
- tenesmus
- melena
On the website GastroScan.ru in the “Literature” section there is a subsection “Diseases of the colon and anus”, containing publications for healthcare professionals regarding the treatment of the colon and diseases of the anal canal.
Back to section
Intestinal diverticula
Treatment of patients with an uncomplicated form of diverticulosis is carried out in the gastroenterology department, and in case of severe complications - in a surgical hospital. Patients with acute or exacerbation of chronic diverticulitis, intoxication, high fever, severe concomitant pathology, impossibility of enteral nutrition, as well as those over 85 years of age are hospitalized. If there is a clinic with an acute abdomen, an urgent operation is performed.
Conservative treatment
If a patient is accidentally diagnosed with an asymptomatic intestinal diverticulum, no special treatment is required. In the presence of uncomplicated diverticula, a diet rich in fiber, antispasmodics, and prokinetics are prescribed. If all recommendations for treatment of the disease are followed, a lasting clinical effect is usually achieved. If the patient has developed diverticulitis, the use of intestinal antiseptics, antibiotics, and osmotic laxatives is recommended.
To normalize intestinal function, cleansing enemas and uncontrolled use of laxatives should be abandoned. A positive effect is also achieved when moderate physical activity is introduced into the daily routine - they help strengthen the muscular corset of the torso and normalize intestinal motility. To reduce pressure in the intestinal lumen, a diet rich in fiber is prescribed (except for very coarse fibers - pineapples, persimmons, turnips, radishes). The amount of fiber in the diet is increased to 32 g/l. It is necessary to exclude gas-forming foods, legumes, and carbonated drinks. To achieve the desired effect, you should drink at least two liters of water daily.
The use of stimulant laxatives and morphine-based painkillers for diverticula is contraindicated, as they provoke further impairment of intestinal motility and aggravate the course of the disease. To improve the passage of food masses through the intestines, osmotic laxatives are prescribed - they increase the volume of feces and accelerate their movement through the digestive tract. For diarrhea, sorbents and astringents are prescribed, and simethicone preparations are prescribed to relieve flatulence.
Acute diverticulitis requires hospitalization of the patient in a surgical hospital, the appointment of detoxification and plasma replacement agents, and antibacterial drugs. Treatment lasts at least two to three weeks; after discharge from the hospital, maintenance therapy is similar to that carried out for uncomplicated diverticula.
Surgery
Surgical treatment is indicated for the development of life-threatening complications: perforation, abscess formation, intestinal obstruction, profuse bleeding, fistula formation. Also, planned surgery is prescribed for recurrent bleeding and diverticulitis. Usually, a part of the intestine affected by diverticulosis is resected and an anastomosis is performed. In difficult situations, a colostomy is performed to facilitate the outflow of feces, and after stabilization of the condition, reconstructive surgery is performed.