The anatomy of the digestive system includes the oral cavity, esophagus, gastrointestinal tract and accessory organs. All parts of the digestive system are functionally interconnected - food processing begins in the oral cavity, and final processing of food is ensured in the stomach and intestines.
The human small intestine is part of the digestive tract. This department is responsible for the final processing of substrates and absorption (absorption).
What is the small intestine?
Vitamin B12 is absorbed in the small intestine.
The human small intestine is a narrow tube about six meters long.
This section of the digestive tract got its name due to its proportional features - the diameter and width of the small intestine are much smaller than those of the large intestine.
The small intestine is divided into the duodenum, jejunum and ileum. The duodenum is the first segment of the small intestine, located between the stomach and jejunum.
The most active digestive processes take place here; it is here that pancreatic and gallbladder enzymes are secreted. The jejunum follows the duodenum, its length on average is one and a half meters. Anatomically, the jejunum and ileum are not separated.
The mucous membrane of the jejunum on the inner surface is covered with microvilli that absorb nutrients, carbohydrates, amino acids, sugar, fatty acids, electrolytes and water. The surface of the jejunum increases due to special fields and folds.
Vitamin B12 and other water-soluble vitamins are absorbed in the ileum. In addition, this part of the small intestine is also involved in the absorption of nutrients. The functions of the small intestine are somewhat different from the stomach. In the stomach, food is crushed, ground and initially decomposed.
The most common intestinal diseases and their clinical manifestations
As a rule, problems with the intestines are indicated by the presence of unstable stools. This is manifested by constipation, diarrhea, or alternation of these two troubles. Patients express such complaints if the intestines are involved in the pathological process and there are disorders of absorption mechanisms in it. In addition to diarrhea, some people experience other problems. Often after defecation they have heaviness in the stomach. Sometimes there is a false urge to defecate. The stool may be too light in color or have a greasy texture. They are difficult to wash off. The presence of blood in the stool in the absence of hemorrhoids and fissures should also alert you.
Diseases of the intestinal tract are almost always accompanied by general abnormalities.
Stool disorder may be accompanied by characteristic pain in the abdominal area. If increased gas formation is observed in the intestines, then the pain is moderate. It is not long lasting. As a rule, the pain intensifies in the late afternoon. To reduce discomfort, you should take laxatives. During inflammatory processes, as well as impaired blood supply, the walls contract spastically. The pain is intense. It is antispasmodic in nature. It is impossible to identify a clear localization; the pain spreads throughout the entire abdomen.
Disorder - as one of the symptoms of small intestinal disease
Symptoms of intestinal manifestations include bloating, rumbling and movements in the abdomen. They occur after eating foods prone to gas formation. These are, for example, legumes, cabbage, rye bread, potatoes, etc. At night, these symptoms intensify significantly.
Absorption and digestion of food does not occur properly. This leads to weight loss. The skin becomes dry, hair falls out, and wounds appear at the corners of the mouth. Bones are more susceptible to fractures. Vision is impaired, limbs swell. There are two main signs by which a pathological condition is determined:
- maldigestion – insufficiency of digestion;
- malabsorption – problems with absorption.
Intestinal digestive insufficiency occurs due to insufficient enzymes. However, they may be completely absent or produced in small quantities. Enzyme deficiency can be either congenital or acquired. In the latter case, diseases arise due to:
Anatomy of the small intestine
The small intestine is in contact with the pancreas.
As we noted above, in the digestive tract the small intestine follows immediately after the stomach. The duodenum is the initial section of the small intestine, following the pyloric section of the stomach.
The duodenum begins with the bulb, bypasses the head of the pancreas and ends in the abdominal cavity with the ligament of Treitz.
The peritoneal cavity is a thin connective tissue surface covering some of the abdominal organs.
The rest of the small intestine is literally suspended in the abdominal cavity by the mesentery, which is attached to the posterior abdominal wall. This structure allows parts of the small intestine to be freely moved during surgery.
The jejunum occupies the left side of the abdominal cavity, while the ileum is located on the upper right side of the abdominal cavity. The inner surface of the small intestine contains mucous folds called circular rings. Such anatomical structures are more numerous in the initial part of the small intestine and contract closer to the distal ileum.
The assimilation of food substrates is carried out with the help of primary cells of the epithelial layer. Cubic cells located throughout the entire area of the mucous membrane secrete mucus, which protects the intestinal walls from an aggressive environment.
Enteric endocrine cells secrete hormones into the blood vessels. These hormones are essential for digestion. Flat cells of the epithelial layer secrete lysozyme, an enzyme that destroys bacteria. The walls of the small intestine are tightly connected to the capillary networks of the circulatory and lymphatic systems.
The walls of the small intestine consist of four layers: mucosa, submucosa, muscularis and adventitia.
Structure of the small intestinal wall
On a section, the intestinal wall consists of 4 membranes of different histological structure (from the lumen outward):
- Mucous;
- Submucosa;
- Muscular;
- Serous.
Mucous membrane
The mucous membrane of the small intestine has circular folds protruding into the lumen of the intestinal tube, with villi and intestinal glands. The functional unit of the intestine is the villus, which is a finger-shaped outgrowth of the mucous membrane with a small area of submucosa. Their number and size are different in different segments of the intestine: in 12 PCs - up to 40 units per 1 square millimeter and up to 0.2 mm in height. And in the ileum, the number of villi decreases to 20-30 per 1 square millimeter, and the height increases to 1.5 mm.
In the mucous membrane, under a microscope, a number of cellular structures can be distinguished: border, stem, goblet, enteroendocrine cells, Paneth cells and other macrophage cellular elements. Border cells (enterocytes) have a brush border (microvilli), at the level of which parietal digestion occurs and due to the number of villi of which the surface of contact of food with the area of the inner lining of the intestine increases 20 times. Also, the presence of folds and fibers contributes to a 600-fold increase in the overall suction surface. In total, the working area of the intestine is up to 17 square meters in an adult.
Be sure to read:
Large duodenal (Vater) papilla: location, functions and diseases of the structure
At the level of the border cells, proteins, fats and carbohydrates are broken down into their simplest components. Goblet cells produce a mucous secretion to facilitate the movement of food chyme through the intestine and prevent “self-digestion.” Paneth cells secrete a protective factor - lysozyme. Macrophages are involved in protecting cells and the body from the penetration of bacteria and viruses with food into tissues.
Submucosa
The submucosal layer contains abundant nerve endings, blood vessels, lymphatic vessels, and Peyer's patches (lymph nodes).
Muscularis
The muscular plate is represented by smooth muscle circular fibers that ensure the movement of villi and motility of the intestinal tube.
Serosa
The serous membrane covers the loops of the small intestine and provides mechanical protection from damage and mobility.
Functional significance
The small intestine consists of several sections.
The human small intestine is functionally connected to all organs of the gastrointestinal tract; the digestion of 90% of food substrates ends here, the remaining 10% is absorbed in the large intestine.
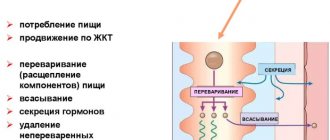
The main function of the small intestine is to absorb nutrients and minerals from food. The digestion process consists of two main parts.
Diseases of the small intestine
Among all intestinal diseases, pathologies of the small intestine are relatively uncommon. The most common diseases are:
- enteritis: infectious enteritis (cholera, typhoid, salmonella, tuberculosis, viral and other rarer forms);
- toxic enteritis due to poisoning by poisons, mushrooms, heavy metals (arsenic, lead, mercury), drugs;
- allergic enteritis;
- radiation enteritis (due to prolonged exposure to radiation);
- chronic enteritis due to alcohol dependence;
- household forms of enteritis due to the abuse of saline laxatives and certain foods;
- enteritis against the background of chronic severe diseases (uremia);
Be sure to read:
Gastroenteritis: how is the pathology manifested and treated?
Ensuring digestion
In the small intestine, proteins are broken down and fats are digested.
After rough processing of products in the stomach, it is necessary to decompose the substrates into separate components accessible for absorption.
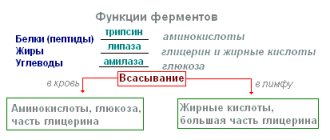
- Protein decomposition. Proteins, peptides and amino acids are affected by special enzymes, including trypsin, chymotrypsin and intestinal wall enzymes. These substances break down proteins into small peptides. The process of protein digestion begins in the stomach and ends in the small intestine.
- Digestion of fats. Special enzymes (lipases) secreted by the pancreas serve this purpose. Enzymes break down triglycerides into free fatty acids and monoglycerides. An auxiliary function is provided by bile juices secreted by the liver and gall bladder. Bile juices emulsify fats - they separate them into small drops accessible to the action of enzymes.
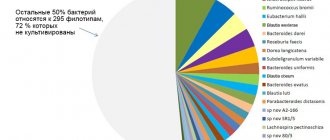
- Digestion of carbohydrates. Carbohydrates are divided into simple sugars, disaccharides and polysaccharides. The body needs the main monosaccharide – glucose. Pancreatic enzymes act on polysaccharides and disaccharides, promoting the decomposition of substances into monosaccharides. Some carbohydrates are not fully absorbed in the small intestine and end up in the large intestine, where they become food for intestinal bacteria.
Functions of the small intestine
The small intestine includes several important functions in the digestive system.
- Digestive function. Ensures the breakdown and absorption of nutrients (vitamins, organic structures, water, salt, some medications) into the blood for delivery to all organs and systems of the body, the formation of final products that pass unchanged into the feces.
- Secretory function. This is the secretion of intestinal juice up to 2.5 liters per day, containing enzymes for processing proteins, fats, carbohydrates into the simplest substances - peptidase, lipase, disaccharidase, alkaline phosphatase and others.
- "Reservoir" function. It is determined by the accumulation and activation of the secretions of other glands - pancreatic juice, bile, which are released when food enters the stomach and 12 PCs and are involved in digestion.
- Endocrine function. It consists in the production by cells of the small intestine (especially in the 12 PCs) of hormones and mediators (histamine, serotonin, gastrin, motilin, cholecystokinin).
- Motor-evacuation function. Provides for contraction of the wall of the intestinal tube due to peristaltic waves, advancement and mixing of food masses (chyme), and the work of villi.
Currently, despite the widespread prevalence of gastroenterological diseases, diseases of the small intestine (SI) remain unknown to practicing doctors. Some of these diseases are quite common, others are extremely rare. However, knowledge of the clinical picture of these diseases and methods of therapy can in many cases cure the patient or alleviate his condition and prolong life.
Diseases of the small intestine are characterized by specific morphological changes in the small intestinal mucosa (SIMU) of varying severity. In most cases, TC diseases have a severe, often progressive course. For 1973-2013 In the department of intestinal pathology of the Central Research Institute of Gastroenterology (TsNIIG), 1168 patients with various diseases of the colon were observed (see table).
Typical TC diseases were chronic diarrhea, malabsorption syndrome (MAS) and exudative enteropathy syndrome.
SNV is an indicator of decompensation of the digestive and transport function of the MC. The degree of its severity may change downward under the influence of treatment or increase with inadequate therapy or its absence. Malabsorption syndrome is the leading one in the clinical picture of TC diseases.
There are 3 degrees of severity of SNV [1].
I degree.
Impaired absorption is manifested mainly by a decrease in body weight (no more than 5-10 kg), decreased performance, general weakness, symptoms of vitamin deficiency, a positive symptom of “muscle roll” (an indicator of increased neuromuscular excitability due to calcium deficiency).
II degree.
More often there is a more significant deficiency of body weight (in 50% of patients more than 10 kg), severe symptoms of hypovitaminosis, electrolyte disturbances (potassium, calcium deficiency), hypochromic anemia, and in some patients - hypofunction of the endocrine glands, mainly the genitals.
III degree.
Body weight deficiency of more than 10 kg in the vast majority of patients. All patients have severe symptoms of polyhypovitaminosis, disorders of water and electrolyte metabolism (hypokalemia, hypocalcemia, convulsions, in some cases - osteopenia, osteoporosis), anemia, hypoferremia, hypoproteinemia, hypoproteinemic edema, dysfunction of the endocrine system (polyglandular insufficiency).
In a number of pathological conditions, increased losses of plasma proteins in the gastrointestinal tract (GIT) have been noted - exudative enteropathy syndrome. It is characterized by a decrease in plasma protein levels (often up to 30-40%), primarily due to a decrease in albumin levels. This syndrome differs from SNV in that with a sharp disturbance of protein metabolism (hypoproteinemia, often hypoproteinemic edema), almost no disturbances in other types of metabolism are detected.
Methods for diagnosing chronic intestinal diseases
Anamnesis
When collecting complaints, you should first of all pay attention to the nature of the stool. In chronic TB diseases, diarrhea is most often observed (it is important to take into account not only the frequency of stool, but also its daily quantity). In most cases, with chronic TB diseases, polyfecal matter with severe steatorrhea is observed. In this case, stool occurs not only during the day, but also at night. Polyfecalia with steatorrhea is most typical for patients with celiac disease, intestinal lymphangiectasia, and common variable hypogammaglobulinemia (CVGG).
Visible peristalsis is often observed with dynamic intestinal obstruction in patients with celiac disease and OVGG. Chronic partial intestinal obstruction develops most often as a result of stenosis of the area
TC - with organic damage by a tumor process, Crohn's disease.
When collecting an anamnesis, it is necessary to clarify the time of appearance of the first clinical symptoms - from early childhood (with typical celiac disease, primary lymphangiectasia), in women (connection with gynecological history: exacerbations associated with pregnancy, the postpartum period, which is typical for celiac disease). It is important to clarify the presence of a history of repeated infectious diseases (chronic bronchitis, pneumonia, sinusitis, otitis), which is typical for immunological deficiency (IVGG).
Objective examination
When examining the abdominal cavity in patients with SNV of I and II severity, it is relatively rare to suspect TC involvement. Sometimes there is bloating around the navel (a symptom of a knocked over pot). On palpation, the sound of splashing and rumbling in the cecum is most often detected (Obraztsov’s symptom).
In patients with severe malabsorption in the small intestine (with SNV of severity III), the abdomen is often enlarged, swollen, and flattened in a “frog” shape.
Palpation creates a feeling of “doughiness” and fullness of the abdominal cavity. Splashing and rumbling on palpation are detected not only in the blind, but also in the loops of the TC. Severe INV can be objectively expressed only by loss of body weight. An objective examination can reveal dryness and flaking of the skin, changes in its color (dirty gray tint, age spots on the face, pigmentation of the arms, hands, face and neck, diffuse pigmentation of the skin, especially pronounced in areas exposed to light and friction). Weeping cracks may appear in the corners of the mouth, less often behind the ears and at the wings of the nose. Nails become dull, thinned, cross-striated, flake, and sometimes take the shape of “watch glasses.” There is thickening of the terminal phalanges on the hands (symptom of “drum fingers”).
Symptoms of increased bleeding may appear in the form of petechial or subcutaneous hemorrhages (nasal, gum, uterine, hematuria, gastrointestinal). The language changes. It may be loose, swollen with teeth marks along the edges. In other cases, atrophy of the papillae may occur and then the tongue becomes smooth, as if polished, sometimes crimson-red in color.
Increased neuromuscular excitability often occurs, which is revealed by the positive symptom of a “muscle roll” (convulsive contraction of the biceps brachii muscle when irritated by pinching or tapping). With hypoproteinemia (SNV III severity), swelling of the legs, feet, thighs, and anterior abdominal wall may appear. The most pronounced edema, which occurs before other clinical manifestations of SNV, is observed in the syndrome of exudative enteropathy. Patients often experience severe hypotension [2].
Laboratory methods characterizing metabolic disorders in the body
In TC diseases, the level of hemoglobin in the blood is important. Celiac disease is characterized by the development of iron deficiency anemia. Some TC diseases can be complicated by blood loss (ulcerative jejunoileitis, intestinal angiodysplasia). In severe forms of malabsorption syndrome, mixed anemia (B12-folate-iron deficiency) often develops.
Biochemical blood tests reveal deviations from the norm only in patients with SNV of II-III severity. Hypoproteinemia due to hypoalbuminemia, hypocholesterolemia, hypocalcemia, hypokalemia, hypomagnesemia, hypoferremia may be observed.
In patients with SNV II and III severity, immunoglobulins of all classes are determined in order to diagnose OVGG or isolated IgA deficiency, and antibodies to gliadin, endomysium, tissue transglutaminase, deamidated gliadin peptide of the IgA class are also determined to identify patients with suspected celiac disease [3]. In case of heavy α-chain disease (Mediterranean lymphoma), pathological IgA, whose molecules consist only of heavy α-chains, is detected at an early stage.
Determining the daily amount of feces is of important diagnostic importance. Normally, it does not exceed 200-300 g, and in case of TC diseases it is often 1000-1500 g/day.
If a helminthic or parasitic infestation is suspected, repeated stool tests are performed for protozoan eggs and worm eggs. Determining blood loss through the gastrointestinal tract is of important diagnostic importance, and therefore it is necessary to re-examine stool for the presence of blood pigment.
Microscopic examination of undigested food debris in feces is usually not informative enough. However, it is necessary to pay attention to the presence of undigested fat and large amounts of fatty acids in the feces, which may indirectly indicate a violation of the digestion and absorption of lipids.
Endoscopic examination of the small intestine
Esophagogastroduodenoscopy
with a biopsy from the descending part of the duodenum followed by a morphological study of biopsies of the mucous membrane is used in the diagnosis of patients with celiac disease, Whipple's disease, intestinal lymphangiectasia, and common variable immunodeficiency. Colonoscopy with examination of the terminal ileum is used to diagnose Crohn's disease of the ileum, tuberculous ileotiphlitis, and yersiniosis.
Capsule endoscopy
- a modern method for studying the gastrointestinal tract, which makes it possible to visualize areas of the intestine that are inaccessible to traditional methods of gastro- and colonoscopy. Used for bleeding to identify the source of bleeding, diagnose Crohn's disease TK, lymphoma.
Double balloon enteroscopy
allows you to examine deep areas of the small intestine and, if necessary, take a biopsy of the intestine. This method of endoscopic examination is used to determine the source of bleeding, diagnose Crohn's disease, tumors of the breast, or clarify the nature of the developmental anomalies of the breast revealed by X-ray examination.
X-ray examination of the TC
Despite the increasingly widespread use of double-balloon endoscopy, video capsule, computed tomography and magnetic resonance enterography, conventional X-ray examination of the colon (studying the passage of barium suspension after oral administration from entry into the duodenum to filling the ileocecal region) is an informative method with high sensitivity and specificity, allows you to assess the functional state of the MC (tone, peristalsis, speed and nature of filling), identify intestinal hypersecretion, and assess the condition of the mucous membrane. These changes are non-specific and complement the clinical understanding of the severity of TC lesions and the extent of changes.
With mild lesions of the TC, dyskinesias are observed - hypo-, hypermotor or hyperhypomotor. Violations of tone are observed less frequently and manifest themselves in uneven filling of the TC with barium, regional hypotension or spasms. In severely ill patients, in some cases with pronounced changes in tone and intestinal hypersecretion, horizontal levels of liquid and gas are found in individual intestinal loops.
Changes in the relief of the mucous membrane are characterized by persistent deformation in the form of rough, wide folds of Kerkring (the result of total edema and swelling of the mucous and submucosal layers), as well as uneven accumulations of barium between the changed folds of the mucous membrane after bowel movement. These changes in all diseases are most pronounced during periods of exacerbation and can gradually disappear with long-term stable remission.
If an organic lesion of the mast cell is suspected, it is necessary to additionally study radiological changes in the mast cell under probe enterography.
The method of probe enterography involves inserting a probe and placing the olive behind the duodenal flexure in the proximal loop of the jejunum. Through a probe, with the patient in the supine position, about 600-800 ml of barium suspension is gradually introduced. Then, to obtain a double-contrast picture, 400-800 ml of air is injected through the probe. To ensure artificial hypotension of the TC in terms of differential diagnosis of organic changes and functional strictures, 2 ml of atropine or metacin are administered intravenously. To achieve intestinal hypotension and open the ileocecal valve, in some cases, sublingual administration of 2-3 aeron tablets is used 20 minutes before the start of the study.
Probe enterography is performed if there is a suspicion of tumors, lymphogranulomatosis, lymphoma of the intestine and lymph glands of the abdominal cavity (mesenteric, retroperitoneal), Crohn's disease, tuberculous ileotiphlitis, celiac disease, Whipple's disease, intestinal lymphangiectasia.
In these cases, the X-ray method makes it possible to identify organic stenoses, intraluminal formations, persistent deformation of individual sections of the intestine, gross changes in the mucous membrane, hyperplasia of the lymphoid elements of the submucosal layer. Polycyclicity of intestinal contours is an indirect sign of enlarged lymph nodes. Severe damage to the upper parts of the colon and the absence of changes in the ileum are much more common than in other diseases in celiac disease.
With tumors of the colon, filling defects, invaginations, circular narrowing of the intestinal lumen, deformation of the relief of the mucous membrane, rigidity of the shadow of the intestinal walls and the tumor itself are observed radiologically. In patients with lymphomas, the intestine has polycyclic contours due to external compression by enlarged lymph nodes [4, 5]. However, enlargement of mesenteric and retroperitoneal lymph nodes in lymphomas and other intestinal neoplasms is more often detected during computed tomography.
Ultrasound examination of the intestines
Ultrasound examination (ultrasound) of the TC is performed 4 hours after eating. Used for suspected neoplasm, Crohn's disease. Allows to identify focal or diffuse thickening of the walls of the colon, pathological narrowing of the lumen, pseudopolyposis, characteristic of Crohn's disease. This diagnostic method helps to detect cancer pathology in the early stages of the disease.
Morphological study of SOTC
A morphological examination of biopsy specimens of SOTK is carried out for all patients with malabsorption syndrome and exudative enteropathy syndrome if the presence of celiac disease, Whipple's disease, intestinal lymphangiectasia, OVGG, eosinophilic gastroenteritis is suspected in order to clarify the diagnosis. Intestinoscopy, double-balloon enteroscopy with targeted biopsy are used for morphological examination of biopsy specimens in cases of suspected TB tumors and TB Crohn's disease.
Morphological examination for celiac disease is the “gold standard”. Pathological changes in the STC can vary widely: from minimal enteropathy with a high number of interepithelial lymphocytes to a flat surface, typical for celiac disease, penetrated by deep crypts.
The standard for assessing the severity of pathological changes in the STC and their dynamics during therapy is considered to be histological examination in accordance with the Marsh-Oberhuber classification, according to which there are 4 stages of the disease [6].
The diagnosis of collagenous sprue is made on the basis of a histological examination of the CBF, which is atrophic, and a massive layer of collagen is formed under the enterocyte membrane, aggravating the malabsorption in the TC.
In Whipple's disease, macrophages with large granules in the cytoplasm are found in the STC - the so-called CHIC-positive or RAS-positive macrophages. The same macrophages are detected in the mesenteric lymph nodes. Electron microscopy reveals microorganisms inside macrophages - Tropheryma whippelii
[7]. After treatment with antibiotics in a phase of stable remission, they disappear, and during an exacerbation they reappear.
In case of amyloidosis, the deposition of homogeneous masses in the wall of small vessels and the lamina propria with a positive stain for Congo red and a positive reaction for amyloid is observed in the CTCS. Amyloid is detected under a polarizing microscope [8].
With intestinal lymphangiectasia in the intestinal tract, dilation of the lymphatic vessels is detected in the mucosal and submucosal layers of the intestinal tract. The wall of the mesenteric lymphatic vessels is thickened, their muscle layer is hypertrophied. Dilated lymphatic vessels look like cavernous formations in the submucosal layer of the TC, sometimes in the form of “lakes” filled with thick lymph. Signs of STC atrophy are not detected.
One of the forms of OVGGG is hypogammaglobulinemic sprue, in which the symptoms of OVGGG are combined with the symptoms of celiac disease. The disease is rare. Along with the symptoms characteristic of general variable hypogammaglobulinemia, there are pronounced gastrointestinal disorders. When studying the morphological structure of SOTK, along with the absence of plasma cells characteristic of OVGG, atrophy is revealed, similar to that found in celiac disease [9].
To diagnose Crohn's disease, as a rule, a histological examination of surgical material is used, since a biopsy does not always allow a correct diagnosis. Histological examination of surgical material for Crohn's disease reveals damage to all layers of the intestinal wall. The most characteristic are swelling and hyperplasia of lymphoid elements in the form of follicles in the submucosal layer. In more than half of the cases, it is possible to detect granulomas consisting of giant Pirogov-Langhans cells surrounded by a belt of lymphocytes that do not have clear boundaries. Ulcers, intramural abscesses, and infiltration of all layers of the muscle wall with plasma cells and fibroblasts may be detected.
Thus, the difficulties in diagnosing diseases of the small intestine are largely explained by the peculiarities of the location of the organ, which is almost inaccessible for research, and the similarity of clinical syndromes. Establishing the correct diagnosis is possible by prescribing the most informative laboratory and instrumental diagnostic methods for each disease. The use of such a clinical approach makes it possible to recognize most TC diseases in a regular gastroenterology department.