The colon makes up approximately 4/5 of the total length of the large intestine. It has four sections: the ascending, transverse, descending and sigmoid colon. The latter passes into the rectum.
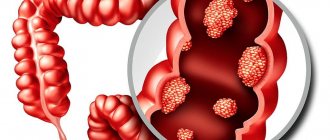
Colon cancer is one of the most common cancers. This pathology is usually referred to as “colon cancer.” Tumors of the colon and rectum are combined into one group of oncological diseases and are called colorectal cancer.
Typically, the appearance of a malignant tumor of the colon is preceded by the appearance of a benign neoplasm - a polyp. There are different types of polyps, and they have different potential for malignancy. The risks increase with age, so everyone 50 years of age and older is recommended to undergo a screening endoscopic examination - a colonoscopy.
Depending on the anatomical part of the tumor, cancer is classified into the transverse colon, ascending and descending colon, and sigmoid colon.
- Causes of colon cancer development
- Classification
- Stages of Colon Cancer
- How does cancer metastasize from the colon?
- Symptoms
- Complications of colon cancer
- Diagnostic methods
- Treatment methods
- Forecast
Causes of colon cancer development
It is impossible to say exactly why a particular person developed a malignant tumor in the colon. Cancer is always the result of a specific set of mutations in a cell, but what led to these mutations is a difficult question to answer.
There are some risk factors that increase the likelihood of developing colorectal cancer:
- Age. The risk of getting sick increases after 50 years. Apparently, this is due to the fact that over time, more and more genetic defects accumulate in the cells of the human body.
- Heredity. If your close relatives (parents, sisters, brothers, children) have been diagnosed with colon cancer, your risk is also increased.
- Unhealthy eating. The development of cancer is promoted by a “Western” diet, which contains a lot of red and processed meat, fast food, processed foods, and little fruits, vegetables and fiber. There are especially many carcinogens in food prepared by frying, grilling, or barbecuing.
- Low physical activity. People who lead a sedentary lifestyle are at increased risk.
- Excess weight. People who are overweight or obese are more likely to get colon cancer and have a worse prognosis.
- Smoking. The development of malignant tumors in the intestines is promoted by smoking and excessive alcohol consumption.
- Hereditary diseases. Parents can pass on certain mutations to their children that make them more susceptible to developing cancer. The most common hereditary diseases from this group are Lynch syndrome, as well as familial adenomatous polyposis.
- Chronic inflammation of the colon : ulcerative colitis, Crohn's disease.
None of these factors are 100% likely to cause colon cancer. Each of them only increases the risks to a certain extent. Some of these factors can be influenced, for example, start eating right, giving up alcohol and cigarettes, and playing sports.
Other factors, such as heredity, inflammatory bowel diseases, age, cannot be influenced. You need to be aware of your risks and get checked regularly. You can undergo screening using modern equipment at Euroonko.
Book a consultation 24 hours a day
+7+7+78
Classification
The most common type of colon cancer and colorectal cancer in general is adenocarcinoma . It develops from glandular cells that are found in the mucous membrane. Adenocarcinomas represent more than 96% of malignant neoplasms of the colon. In this group of tumors, a number of subgroups are distinguished. The most aggressive of them are mucinous and signet ring cell carcinoma . Such patients have the most unfavorable prognosis.
Why does inflammation occur?
Inflammation is the death of mucosal cells.
Before answering this question, you need to understand how this painful process generally proceeds.
From a medical point of view, any inflammation is the death of cells of the mucous membranes, accompanied by abundant blood supply to the affected area.
This process is accompanied by inevitable disruptions in the functioning of the “injured” organ and, as a consequence, pain.
The role of the factor that provokes the problem, as a rule, is various harmful organisms. When it comes to intestinal inflammation, it is usually:
- worms and other parasites;
- pathogens (viruses and microbes);
- other pathogenic flora.
Of course, other negative factors can also be the cause of the violation. Among them are:
- autoimmune diseases leading to spontaneous rejection of cells from the mucous membrane of the large intestine;
- genetic predisposition, in other words, an inherited lack of digestive enzymes, causing problems with the gastrointestinal tract;
- poor nutrition, which provokes chemical and mechanical damage to the mucous membranes of the organs involved in the digestive process (usually through the consumption of excessively spicy or fatty foods);
- atherosclerotic abnormalities, due to vasoconstriction, inevitably leading to disruption of the blood supply to the intestinal walls.
The following video will tell you about the symptoms and treatment of colitis:
Stages of Colon Cancer
Colon cancer is classified into stages depending on the size and depth of the primary tumor (T), the presence of foci in regional lymph nodes (N) and distant metastases (M). There are five main stages:
- Stage 0 - “cancer in situ.” A small tumor that is located within the mucous membrane does not grow deeper.
- Stage I is a tumor that has grown into the submucosa or muscle layer of the intestinal wall.
- Stage II - a tumor that has grown into the deep layers of the colon wall (IIA), has grown through it and spread to neighboring organs (IIB), or there is a small tumor, as in stage I, and foci in 1-3 nearby lymph nodes (IIIC ).
- Stage III is divided into three substages: IIIA, IIIB and IIIC, depending on how deep the tumor has grown into the intestinal wall and how many lymph nodes are involved.
- Stage IV : There is metastasis in one organ (such as the liver or lungs) or in a group of lymph nodes that is far from the bowel (IVA), or there are metastases in more than one organ or group of lymph nodes (IVB), or the cancer has spread over the surface peritoneum (IVC). In this case, the size of the primary neoplasm and how deeply it has grown into the wall of the colon are not important.
Specialists
| 5.0 87 reviews | Grigorievskaya Zlata Valerievna Mammologist Experience 18 years Reception from 4500 rub. |
| 5.0 244 reviews | Zagryadsky Evgeniy Alekseevich Mammologist Experience 46 years Doctor of the highest category Reception from 4500 rub. |
Medical center ON CLINIC on Novy Arbat st. Bolshaya Molchanovka, 32, building 1
| 5.0 75 reviews | Brother Alexander Vladimirovich Mammologist Experience 29 years Doctor of the highest category Admission from 4000 rub. |
How does cancer metastasize from the colon?
Colon cancer can spread to other organs in different ways:
- The implantation route is when cancer cells penetrate into neighboring organs that are in contact with the intestine and “spread” over the surface of the peritoneum.
- Some cancer cells break away from the primary tumor, enter the blood or lymph vessels, and migrate through them to the lymph nodes or other organs. Such routes of metastasis are called hematogenous and lymphogenous .
Most often, metastases from colon cancer are found in the lungs and liver, less often in the bones and brain.
Symptoms
Colon cancer often exists for a long time without causing any symptoms. But even when symptoms do occur, they are nonspecific and resemble those of many other diseases. If you are experiencing problems from this list, most likely you do not have cancer, but you should definitely visit a doctor and get tested:
- constipation or diarrhea that lasts for several days;
- change in the appearance of the stool: if it becomes dark, like tar, or thin, like a pencil;
- blood in the stool;
- after visiting the toilet there is a feeling that the intestines have not been completely emptied;
- pain, abdominal cramps;
- causeless weakness, feeling tired, unexplained weight loss.
Preventive measures
You should always wash your hands before eating.
Like any disease of the gastrointestinal tract, intestinal inflammation can be easily avoided if you follow simple hygiene rules from childhood.
For example, keep your hands clean and wash food before eating. However, in practice, adherence to the banal principles of proper nutrition is no less important. What are they?
If the patient is already aware of the tendency of his intestines to inflammation, it would not be superfluous for him to completely review his diet in order to prevent the disease from becoming chronic. The most rational steps in this sense would be a complete rejection of any exotic food and reasonable restrictions on the use of spicy seasonings.
Complications of colon cancer
If the tumor blocks the lumen of the colon, the patient develops intestinal obstruction . This condition manifests itself in the form of lack of stool, severe abdominal pain, nausea, vomiting, and severe deterioration in general condition. The patient immediately requires medical attention, otherwise necrosis (death) of a section of the intestine may occur and peritonitis will develop.
If the tumor leads to constant bleeding, anemia develops. The patient becomes pale, constantly experiences weakness, and is bothered by headaches and dizziness. In severe cases, a blood transfusion is required.
Metastasis of intestinal cancer to the liver threatens to disrupt the outflow of bile and develop obstructive jaundice - a condition in which the skin and mucous membranes acquire a yellowish tint, itching, abdominal pain, and general condition worsen. Until the flow of bile is restored, it becomes impossible to carry out active antitumor treatment.
A condition in which cancer cells spread over the surface of the peritoneum is called carcinomatosis , and ascites , an accumulation of fluid in the abdomen. This complication develops in stage IVC colon cancer. Ascites worsens the patient's condition, complicates treatment and has a sharply negative impact on the prognosis.
Euroonco has everything you need to effectively combat complications of malignant tumors of the colon. In case of emergency, patients receive full treatment in the intensive care unit. Our surgeons perform palliative operations and install stents for intestinal obstruction. For obstructive jaundice, we perform drainage and stenting of the biliary tract. For ascites, our doctors perform laparocentesis (evacuation of fluid through a puncture), install peritoneal catheters, and conduct systemic and intraperitoneal chemotherapy.
For stage IVC colon cancer, when peritoneal carcinomatosis develops, Euroonco surgeons use an innovative treatment method - hyperthermic intraperitoneal chemotherapy (HIPEC). All large tumors are removed, then the abdominal cavity is washed with a chemotherapy solution heated to a certain temperature - this helps to destroy small lesions. According to the results of world practice, HIPEC can prolong the life of a cancer patient up to several years.
Book a consultation 24 hours a day
+7+7+78
Diagnostic methods
If a patient is concerned about symptoms that may indicate colon cancer, the doctor will first order an abdominal ultrasound and colonoscopy. These studies will help detect a tumor, and during a colonoscopy you can perform a biopsy - obtain a fragment of pathologically altered tissue and send it to the laboratory. A biopsy is the most accurate method for diagnosing cancer.
Colonoscopy is an effective screening method. It helps detect polyps and colon cancer in the early stages. It is recommended for all people over 50 years of age. At Euroonco, colonoscopy is performed by expert doctors using the latest equipment from leading manufacturers. Our procedure takes place in a state of “medicated sleep,” so you will not experience any discomfort.
Once cancer is diagnosed, its stage must be determined. For this purpose, CT, MRI, and PET scans are used. Metastases in the lungs are detected using chest x-ray. If there are metastases in the liver, angiography is used - an X-ray examination, during which a contrast solution is injected into the blood vessels.
Additionally, the doctor may prescribe a stool test for occult blood, a general and biochemical blood test to detect anemia, and evaluate liver function. Blood tests for tumor markers are usually performed during treatment to monitor its effectiveness.
Differential diagnosis
The symptoms that occur with colon cancer can be disturbing in many other pathologies. Most often, a malignant tumor must be differentiated from diseases such as intestinal infections, chronic inflammatory processes, hemorrhoids, and irritable bowel syndrome.
Typical symptoms
Bloating indicates a lack of digestive enzymes.
Symptoms that appear during inflammatory processes in the intestines can vary greatly depending on the location of the problem.
However, some of the characteristic manifestations of such ailments can be considered common.
It is on them that doctors rely when making a preliminary diagnosis of “inflammation of the intestines.” Among these specific features, the following can be particularly highlighted:
- pain of a bursting or compressive nature, the main source of which, as a rule, is not possible to determine;
- nausea and vomiting syndrome, usually worsening after eating and subsiding after cleansing the stomach;
- bloating and other symptoms indicating a lack of digestive enzymes;
- unstable stool (from constipation to diarrhea);
- anemia (anemia occurs as a result of a lack of iron, inevitable with intestinal damage);
- increased temperature (a reaction typical of any inflammatory process).
Treatment methods
There are different treatment options available for colon cancer. The doctor chooses the optimal tactics, depending on the stage of the malignant tumor, its location, the general condition of the patient, the presence of certain complications, and concomitant diseases. They perform surgical interventions, use different types of antitumor drugs, and conduct courses of radiation therapy.
Chemotherapy
Chemotherapy for malignant tumors of the colon can have different goals:
- Neoadjuvant chemotherapy is given before surgery to shrink the tumor and make it easier to remove.
- Adjuvant chemotherapy is given after surgery to kill any remaining cancer cells and reduce the risk of recurrence.
- as the main treatment method for advanced stages of cancer for palliative purposes.
For malignant neoplasms of the colon, different types of chemotherapy drugs are used: capecitabine, 5-fluorouracil, oxaliplatin, irinotecan, trifluridine/tipiracil (combination drug). Most often, two or more drugs are used simultaneously, this helps to increase the effectiveness of treatment.
Targeted drugs have a more targeted effect compared to classical chemotherapy drugs: they are aimed at specific target molecules that help cancer cells multiply uncontrollably and maintain their vital functions. Most often, two groups of targeted drugs are used for malignant intestinal tumors:
- VEGF inhibitors are substances that cancer cells use to stimulate angiogenesis (the formation of new blood vessels). This group includes: Ziv-aflibercept (Zaltrap), Ramucirumab (Ciramza), Bevacizumab (Avastin). They are used for advanced colon cancer, administered intravenously every 2 or 3 weeks, usually combined with chemotherapy.
- Inhibitors of EGFR , a receptor protein that is found on the surface of cancer cells and causes them to multiply uncontrollably. This group includes drugs such as Cetuximab (Erbitux), Panitumumab (Vectibix). EGFR inhibitors are administered intravenously once a week or every other week.
In some cases, drugs from the group of checkpoint inhibitors . They block molecules that prevent the immune system from recognizing and attacking cancer cells. This group of drugs includes: Pembrolizumab (Keytruda), Nivolumab (Opdivo), Ipilimumab (Yervoy). They are usually used for inoperable, metastatic cancer, when chemotherapy is ineffective if there is a relapse.
In order to figure out which drugs will be effective in a particular patient, you need to understand what properties cancer cells have, what mutations have occurred in them, and due to what substances they have acquired the ability to reproduce uncontrollably. Molecular genetic analysis helps with this - compiling a “molecular portrait” of cancer. Thanks to our cooperation with leading foreign laboratories, such research can be carried out at Euroonco. We know how to increase the effectiveness of antitumor treatment and what to do if it stops helping.
Surgery
In some cases (stage 0, cancer in situ; sometimes stage I), colon cancer can be removed during a colonoscopy. Unfortunately, this opportunity is rarely available. Most often, you have to perform a colectomy - partial or complete removal of the colon. The extent of surgical intervention depends on the location and size of the tumor. Typically, at least 12 nearby lymph nodes are removed at the same time. The remaining ends of the intestine are sewn together and an anastomosis .
Colectomy can be performed openly (through an incision) or laparoscopically (through punctures in the abdominal wall).
Sometimes the anastomosis cannot be performed immediately. In such cases, a temporary colostomy or ileostomy - a section of the colon or ileum is sutured to the skin and an opening is created for the passage of stool. The stoma is subsequently closed.
If the tumor blocks the intestinal lumen and cannot be removed, a permanent colostomy is performed. Intestinal patency can be restored using a stent - a metal frame in the form of a hollow cylinder with a mesh wall. Such operations are called palliative : they are not aimed at removing cancer, but at combating symptoms and improving the patient’s condition.
Surgeons at Euroonco perform various types of radical and palliative interventions. The specialists in our endoscopy department have extensive experience in installing stents in the intestine, bile ducts and other hollow organs. The Department of Interventional Surgery performs radiofrequency ablation and chemoembolization for liver metastases.
Radiation therapy
Radiation therapy may be given before ( neoadjuvant ), after ( adjuvant ) colon surgery, or as the primary treatment for metastatic cancer to control symptoms.
When radiation therapy is combined with chemotherapy, the treatment is called chemoradiotherapy .
Colonoscopy only under general anesthesia
— Colonoscopy is a scary procedure for many. How is the research going?
— The proportion of patients undergoing endoscopic treatment is increasing. This is due to the greater introduction of endoscopic technologies, training of personnel, and education of people. Colonoscopy is becoming, shall we say, friendlier. Doctors used to tell their patients that a colonoscopy was the last thing they should do. People were more afraid not even of the diagnosis, but of the procedure itself - it was believed that it was painful, awkward, and humiliating for some. Preparation for it was difficult; if the first procedure was ineffective, it was necessary to do a second one. Taken together, this gave rise to the idea in people’s minds that a colonoscopy was something prohibitively acceptable for them. Of course, this is an unpleasant, intimate procedure. But today in Russia doctors have learned to do it well. Finally, anesthesia began to be widely used. There is no need to be afraid of him. Throughout the Western world, this procedure is performed only under general anesthesia. Because it ensures not only patient comfort, but also the quality of the study. This applies not only to colonoscopy, but also to gastroscopy. In order not to miss complex tumors (some differ little from gastritis), you need to study the stomach for 15–20 minutes. Study statically, without movements, rocking or belching air. It’s easier with the colon, but here people are afraid of pain. Therefore, I believe that everyone always needs anesthesia for both gastroscopy and colonoscopy, with rare exceptions when health does not allow it. But these are isolated cases. For 7 thousand anesthesia in our department per year, there are 1-2 refusals. Even in weakened and elderly patients, anesthesia is not contraindicated. This is not some special procedure for which you need to prepare for a month and collect tests.
— How long is the patient under anesthesia?
— Exactly as long as the research lasts. The time depends on the “finds” and the complexity of the intestine, it is different for everyone. In general, it is estimated that the machine takes between 3 and 15 minutes to pass through the colon. Next is the examination time, which can last 10, 15, sometimes 20 minutes if the polyp has to be removed. We allow ourselves 40–45 minutes for everything – from the moment of anesthesia to the end of the procedure. Then the patient wakes up, which usually takes him half an hour, sometimes an hour, and he goes home.
- So fast? In some hospitals, people are kept “under observation” for three days after such a procedure.
- There is no need to go to the hospital. This is a relic of the past, which is associated solely with the fear of legal liability. For us, this is already a routine, but in fact it is a great achievement to help a person here and now. The patient came to the doctor and all his polyps were immediately removed. Most polypectomies have the same risk of complications as a biopsy. The patient does not need to be hospitalized and go through all the procedures and manipulations (most of them completely unnecessary), as is customary within the compulsory medical insurance system, when a polyp is found in the patient, then a biopsy is taken, then referred to a proctologist. A person goes to the clinic, makes an appointment, and waits. Then he receives a referral to a hospital. He goes to the therapist and again waits for an appointment. Then an ECG, blood test, urine test, fluorography, Covid smear, and so on are recorded. Then he gets in line for hospitalization and, finally, goes to the hospital. There are allotted bed days. He undergoes colonoscopy and anesthesia again, and again he undergoes histology of the already removed polyp. Huge amounts of money are spent on removing a polyp. For what? If possible, I saw it right away and deleted it. Unfortunately, and this is a huge problem, the compulsory health insurance system does not provide funding for outpatient polypectomy.
— Are there any contraindications for examining and treating patients using endoscopes?
— An absolute contraindication is the terminal condition of the patient. As for relative contraindications... I can’t remember a single case where we refused someone the procedure because it could be dangerous. We have a wide arsenal of equipment and we can select it for a specific patient, taking into account all his characteristics.