The list of diseases affecting the pancreas is not limited to types of pancreatitis. Often, with improper or insufficient treatment, inflammatory pathologies develop into more serious diseases that require careful and long-term therapy. Such a complication is fibrolipomatosis.
General information
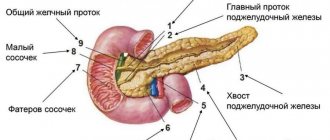
The pancreas is a digestive organ, produces digestive enzymes, and also has endocrine (produces the hormone insulin ) activity. Very often, its defeat is associated with obesity . In overweight patients, non-alcoholic fatty pancreatic disease is diagnosed, which can have two morphological variants - lipomatosis and steatopancreatitis .
They represent different stages of the pathological process. What is pancreatic lipomatosis? Pancreatic lipomatosis is fatty degeneration of the organ (synonyms: pancreatic steatosis, fatty degeneration, non-alcoholic fatty disease of the pancreas). The most acceptable term is pancreatic steatosis, and if it is associated with metabolic syndrome, non-alcoholic fatty pancreatic disease. The terms “lipomatosis” and “fatty gland” are used to refer to all types of fat accumulation in the gland; steatosis refers to the accumulation of fat in the cells of the gland (they are called pancreacytes) and intercellular tissues. The accumulation of fat is accompanied by a gradual disruption of gland function, but without signs of inflammation. Steatopancreatitis is the second, more advanced stage of fatty disease of this organ and additionally includes an inflammatory component (lymphomonocytic-plasmacytic infiltration of the gland tissue occurs).
The prevalence of steatosis increases with patient age. The accumulation of fat in cells is associated with weight gain , insulin resistance and metabolic syndrome . A direct connection has also been recorded between diabetes mellitus and this gland pathology, and vice versa - patients with fatty infiltration of the organ have a high risk of diabetes mellitus . At the initial stage, steatosis is reversible and a decrease in its severity is noted with weight loss.
Fatty infiltration of the organ is more common in men over 40 years of age, with elevated levels of cholesterol , triglycerides and glucose . Previously, fatty infiltration of the gland was considered a harmless condition, but observations of patients and studies have shown a high risk of developing diabetes mellitus, gland failure, acute pancreatitis and cancer of this organ, and therefore more attention has been paid to this condition.
Diagnostics
Pancreatic fibrosis in an advanced stage is not so common among the population, because today modern diagnostic methods are used that make it possible to identify the disease in the initial stages of its development and immediately begin treatment.
As for this particular pathology, a gastroenterologist deals with its treatment. During the initial examination, he notes objective signs of the development of the disease, among which are:
- dystrophic changes;
- dry skin and tongue;
- cyanosis;
- redness of the facial skin;
- atrophy of subcutaneous tissue.
The doctor can make a preliminary diagnosis at the initial appointment, but to confirm it you will need to undergo a more detailed examination
In this case, the doctor must palpate the pancreas, during which he notes its compaction. Next, a detailed examination of the body takes place, which, first of all, includes laboratory tests of the blood to determine the protein content in it and determine the level of albumin-globulin ratio. Laboratory tests reveal critically low activity of pancreatic enzymes, which gives an idea of total damage to the pancreas.
To understand how large the pathological processes are and what disorders they have already led to, an ultrasound examination of the abdominal cavity is prescribed. When it is carried out, a diffuse increase in the echogenicity of the organ, heterogeneity of its structure and a decrease in size are noted. During ultrasound, dilation of the Wirsung duct can also be detected.
However, endoscopic ultrography provides the most accurate information about the development of pathological processes in the pancreatic parenchyma. Using this diagnostic method, it is possible to identify linear stringy inclusions of various durations and shapes, the tuberosity of the contours of the pancreas and the hyperechogenicity of its parenchyma. Also, when using this diagnostic method, the condition of the ductal apparatus of the gland and the pathological processes occurring in it are assessed.
Endoscopic ultrasonography
Also no less informative methods for diagnosing pancreatic fibrosis are computed tomography (CT) and biopsy.
Pathogenesis
Fatty infiltration is formed against the background of obesity, which creates the prerequisites for the intracellular accumulation of fats (mainly triglycerides) in the gland cells. This process causes the death of β-cells (they are the endocrine part of the gland and produce insulin), which are replaced by adipocytes (fat cells). The constant influence of high concentrations of free fatty acids on β-cells (lipotoxicity) causes their secretory dysfunction: first, the level of fasting blood glucose increases moderately, then after a food load, and, ultimately, diabetes mellitus develops. And hyperglycemia further impairs β-cell function, completing a vicious circle.
Many authors consider the initial development of fatty infiltration of the liver, and then the pancreas. This is explained by the fact that a diet rich in fats and carbohydrates, as well as hyperinsulinemia, cause the development of changes in the liver and the flow of very low-density lipoproteins into the islets of the pancreas. Insulin resistance at one time causes the release of free fatty acids from adipose tissue, therefore their concentration in the blood increases. If the accumulation of fat in the gland cells exceeds the permissible threshold, then hyperglycemia , which closes a vicious circle of glucose metabolism disorders.
During hyperglycemia, free oxygen radicals are formed from glucose, which triggers free radical oxidation reactions of proteins and lipids. Increased free radical lipid peroxidation causes cell apoptosis, including β-cells, and dysfunction of the gland. At stages II and III of lipomatosis, its function is significantly impaired and the process of autolysis of the gland is started. As a result, inflammation of the parenchyma develops, necrosis , which invariably leads to fibrotic changes and fibrolipomatosis .
Classification
The most common ultrasound classification of glandular lipomatosis is:
- I degree. The size of the gland is not enlarged, the splenic vein and pancreatic duct are clearly visible. The echogenicity of the gland is uniformly increased and is equal to the echogenicity of the adipose tissue located in the area of the mesenteric artery.
- II degree. Indistinct edges of the splenic vein and pancreatic duct. The superior mesenteric artery is almost invisible. Increased echogenicity, but signal attenuation behind the posterior surface of the gland.
- III degree. Reduced ultrasonic conductivity.
According to the prevalence of fatty infiltration, according to the ultrasound picture, there are:
- Diffuse infiltration - fat cells are evenly distributed in the gland tissue.
- Nodular fatty infiltration - limited fat deposits are noted, which are surrounded by a connective tissue capsule and are often located symmetrically.
- Diffuse nodular infiltration - two types of changes are detected simultaneously.
In accordance with MRI data, the clinical course of lipomatosis has the following degrees:
- Pancreatic lipomatosis stage 1. This is the initial stage, when one third of the organ is replaced by adipose tissue. At grade 1 there are no symptoms. The function of the organ is compensated.
- At grade 2, half of the parenchyma of the gland is replaced by adipose tissue, which is accompanied by dysfunction of the gland and clinical manifestations. A patient at this stage of the disease most often seeks medical help.
- The 3rd degree is characterized by the replacement of more than 2/3 of the gland with adipose tissue. In this case, there is a violation of exocrine and endocrine function. The patient experiences digestive disorders and increased blood glucose levels.
The combination of pancreatic steatosis and hepatic steatosis occurs in 50-68% of cases of obesity . Liver lipomatosis (steatosis) and pancreas lipomatosis (pancreas) have the same development mechanism - the accumulation of triglycerides in the liver and pancreatic cells. Fatty liver disease is distinguished as an independent entity and also includes two forms: fatty steatosis and non-alcoholic steatohepatitis .
The amount of fat in cells depends on the balance between intake, synthesis and use for the body's needs. In both organs, changes can be focal or diffuse. In the diffuse form, fats are located over the entire surface, and in the focal form, grouped fat deposits are determined. In both cases, the condition of the organ worsens due to an increase in adipose tissue and a decrease in functioning parenchyma. Initially, excess fat in the form of triglycerides is located inside the cells, shifting the nucleus to the periphery. If fatty deposits accumulate in large quantities, the cells rupture and the fats move into the intercellular space, forming a kind of cysts that change the structure of the organ and its function. In most patients, changes at the level of steatosis can remain throughout life, while in others they progress with the development of spaatohepatitis and steatopancreatitis with the transition to fibrosis.
Skin lipomatosis has a completely different genesis and is not associated with general obesity, so these terms should not be confused. Skin lipomatosis (lipomas) is the occurrence of multiple fatty formations in the subcutaneous tissue, which may have a connective tissue capsule or transform into normal adipose tissue without a clear boundary.
Skin lipomatosis occurs more often in men. Lipomas are painless formations and histologically have the composition of adipose tissue. Lipoma fat cells are resistant to lipolytic factors, so they do not shrink even if a person loses a lot of weight.
A type of lipoma is Dercum's disease ( neurolipomatosis ), which is characterized by the appearance of lipoma-like formations in the subcutaneous tissue of the arms, back, mammary glands, abdominal wall, buttocks or thighs. This is a chronic disease that is more common in women aged 30 to 60 years. Subcutaneous tumors from adipose tissue have an irregular shape and are detected simultaneously in different parts of the body.
Characteristic is the pain of the formations with slight pressure and touch, which distinguishes this disease from ordinary lipomas. Pain syndrome has varying degrees of severity in different patients - from moderate intensity to severe. Sometimes pain also occurs in areas where there are no fatty tumor-like formations.
Dercum's disease occurs with compression neuropathy of the nerve branches, resulting in a pain syndrome that is not eliminated by classical analgesics, amitriptyline and carbamazepine . The lack of effective treatment leads to a decrease in quality of life. Other symptoms include: numbness in the fingers, spontaneous swelling in different parts of the body, stiffness in the morning, sleep disturbances, anxiety-depressive syndrome, weakness, aggravated by light exertion, pain in the joints (wrist, elbow, hip) and in long tubular, headache (classic migraine and tension headache), memory impairment, possible fever. The disease is systemic and the localization of fatty formations in the lungs or heart is deadly. The course of the disease varies - the condition can slowly worsen over several years or quickly, under the influence of various factors (surgeries, pregnancy, influenza). More than half of the patients lose their ability to work.
The cause of the disease has been little studied. It is believed that the cause of the disease is a disorder of lipid metabolism and endocrine disorders. A hypothesis is put forward about the autoimmune nature of the disease. Dercum's disease is inherited through the grandmother-mother-daughter line.
A variant of Dercum's disease is Gram syndrome . It is found in older women and is characterized by rapidly increasing obesity with fat deposition in the area of the knee joints and arthrosis of the knee joints. It is also a hereditary disease.
Causes of lipomatosis
The main cause of this disease in various age groups is obesity , which is a leading risk factor for pancreatic pathology.
- Obesity is accompanied by hyperlipidemia and promotes fatty infiltration of the gland and liver. In addition, eating fatty foods causes excess production of pancreatic enzymes and cholecystokinin and disrupts the outflow of pancreatic juice.
- Atherosclerosis . With it, the fat content in the gland exceeds the norm by 25%.
- Fatty degeneration of the pancreas also develops due to the toxic effects of alcohol . Ethanol also negatively affects the progression of the disease and stimulates fibrotic processes.
- Consumption of foods high in animal fats and proteins, as well as alcohol abuse, are the main risk factors for this disease.
- Toxic effects of corticosteroids , gemcitabine and rosiglitazone .
- Presence of diabetes mellitus .
- Hemochromatosis . Iron overload during blood transfusions also causes fatty replacement of the organ parenchyma.
- Kwashirkor.
- Metabolic syndrome (includes abdominal obesity , hyperlipidemia and insulin resistance ).
- Hereditary diseases ( cystic fibrosis , and Johanson–Blizzard syndromes , lysosomal acid lipase mutations).
- Viral diseases ( viral hepatitis , HIV/AIDS).
Prognosis and prevention
The prognosis for pancreatic fibrosis depends on several factors:
- the scale of the disease;
- volumes of functioning of the affected organ;
- patient's lifestyle.
If the patient leads a healthy lifestyle and strictly follows all the doctor’s instructions, then he has every chance of living a long and happy life. However, for this you will have to give up alcohol and smoking once and for all, as well as take enzyme preparations correctly and regularly.
As for the prevention of pancreatic fibrosis, it consists of giving up bad habits and timely treatment of pathologies that can trigger the development of this disease. Persons who have been diagnosed with fibrosis must undergo medical examination. They need to undergo preventive examinations several times a year, including laboratory tests of stool, urine and blood, as well as ultrasound and CT. Based on the results of the examinations, the doctor may periodically adjust the treatment.
Remember that pancreatic fibrosis is a very dangerous disease. And it is much easier to prevent than to treat. Therefore, carefully monitor your diet and lead a healthy lifestyle. Well, if it so happens that this illness does occur to you, strictly follow the doctor’s recommendations. This will allow you to avoid further progression of the disease and the occurrence of serious complications against it.
Symptoms
Clinically, lipomatosis of the gland can be asymptomatic or have a pronounced picture. With a slight accumulation of fat in the gland cells, there are no clinical symptoms and the disease is discovered accidentally during instrumental examination (ultrasound, MRI). Only sometimes Tuzhilin’s symptom - the appearance of small red spots (vascular aneurysms) that do not disappear with pressure. They are located on the abdomen and upper half of the body, but this symptom is not specific to this disease.
With pronounced fatty infiltration, signs of exocrine insufficiency appear: diarrhea , steatorrhea (the presence of an excess amount of neutral fat in the feces), hypovitaminosis . The patient also experiences nausea, bloating, pain or discomfort in the left hypochondrium. Disruption of the endocrine function of the gland manifests itself in impaired carbohydrate metabolism ( fasting hyperglycemia , insulin resistance , impaired glucose tolerance). Since dysfunction of the pancreas always leads to dysfunction of the biliary system, the patient experiences bitterness in the mouth and pain in the right hypochondrium. If we talk about steatopancreatitis , it often appears as a moderately severe pain and dyspeptic syndrome (belching, nausea, tendency to frequent vomiting, bloating, aversion to fatty foods).
Main symptoms
The initial stages of the disease are often asymptomatic, making it difficult to diagnose. However, if the affected areas reach a maximum and an exacerbation of the pathology is brewing, the following symptoms may occur:
- nausea and vomiting;
- sudden weight loss;
- change in appetite;
- flatulence, heartburn;
- change in stool, diarrhea, indigestion;
- yellowing of the skin and sclera;
- heaviness in the stomach;
- bad breath;
- severe pain in the hypochondrium.
Most often, these signs are observed in older people. In the early stages of progression, lipofibromatosis is usually determined using ultrasound diagnostics. Treating the pathology is quite difficult.
Tests and diagnostics
- Transabdominal ultrasound. Signs of steatosis of the gland are: an increase in its echogenicity while maintaining the homogeneity of the structure, possibly a slight increase in the size of the organ. Such changes are referred to as diffuse changes in the pancreas. Its echogenicity is assessed indirectly by comparing it with the echogenicity of the liver and kidneys. The echogenicity of a healthy gland is the same as that of the liver. In fatty liver disease, the echogenicity is higher than that of the kidneys. The information content of ultrasound is quite low, since patients have abdominal obesity and flatulence .
- Multislice CT. Accurately determines the presence of fatty inclusions, layers, and allows you to detect fibrosis. The examination also gives a picture of the condition of the peripancreatic tissue.
- MRI. It is considered the best diagnostic method. Modern MRI technology determines homogeneous changes in the structure of the gland; with proton MR spectroscopy, the content of triglycerides is assessed quantitatively.
- Endosonography. It is an invasive procedure and allows you to obtain highly accurate images, as well as reliably confirm steatosis. The resolution of this method is superior to CT and MRI, but there is a risk of complications.
- From clinical and biochemical examinations, determination of the level of glucose, triglycerides, cholesterol, low-density lipoproteins.
Treatment
Therapy for many diseases of the internal gastrointestinal tract requires a special diet and drug or surgical treatment. To speed up the recovery process, as well as to improve the patient’s general condition, you can also use some folk remedies.
Therapy, diffuse organ changes
Fibrolipomatosis is directly treated in two ways: medication or surgery. In the early stages, as a rule, the following types of drugs are used:
- anti-inflammatory (Ibuprofen);
- containing digestive enzymes (Pancreatin, Festal);
- antiemetics (Metoclopramide);
- painkillers (No-Shpa, Mebeverine).
After such therapy, patients’ digestion improves and is restored, and weight loss stops.
If diffuse changes in the pancreas such as fibrolipomatosis affect more than 60% of the total volume of the organ, surgery is prescribed. In this case, the affected areas, abnormal fat and connective tissue are completely removed. The procedure is performed under general anesthesia and requires subsequent rehabilitation, adherence to the regimen and a therapeutic diet.
Patients undergoing treatment for fibrolipomatosis should attend preventive examinations with their doctor twice a year.
Diet
Proper dietary nutrition is one of the most important components of treatment. The list of permitted products includes:
- stale bread, crackers;
- vegetables, unsweetened fruits;
- fermented milk products;
- lean meat and seafood;
- cereals;
- steam omelette.
The following foods should not be consumed if you have fibrolipomatosis:
- fatty meats and fish;
- semi-finished products (especially purchased);
- fresh baked goods and white bread;
- sweets and confectionery;
- liver;
- hard and fatty cheeses;
- fatty and sour sauces;
- spicy seasonings;
- canned food;
- smoked meats
These lists may be changed and supplemented due to the individual characteristics of patients. It is important that gastric and pancreatic juice are released in sufficient quantities for digestion, but do not increase inflammatory processes.
Eating food should be done according to the following rules:
- You need to eat in small portions. The number of meals should be about five to six per day.
- Any food needs to be cooked only with water and steam. You can also bake in the oven.
- It is advisable to add as little salt as possible to dishes.
- Food should not be too hot or very cold.
- Mix ingredients carefully during cooking. They must be combined with each other so as not to cause harm to the digestive system.
By adhering to the correct diet after surgery or drug treatment, you can not fear for your life and lead a normal lifestyle.
Folk remedies
It is important to choose the right recipes for traditional medicine. Potentially dangerous or known harmful drugs should not be included in the course of therapy against pancreatitis or fibrolipomatosis.
The following effective recipes are known:
- Infusion of birch buds. Fill a glass of washed raw material to the top with vodka and leave for one month in a dark, cool place. Take the medicine three times a day, one tablespoon at a time.
- Infusion of lilac buds. Pour a tablespoon of the product into a glass of boiling water and leave for half an hour. Take the filtered product one tablespoon three times a day before meals.
- Plantain infusion. Wash and chop a tablespoon of leaves, pour a glass of boiling water and leave for three hours.
- Take the product three times a day before meals, 70 milliliters.
- Collection of medicinal herbs. Mix valerian, nettle, St. John's wort and calendula in equal quantities. Pour one spoonful of the mixture into a glass of boiling water and leave for half an hour. You need to drink this glass of infusion in small sips throughout the day.
You can use recipes for traditional methods of therapy only with the permission of the attending physician and only as an auxiliary treatment. In this case, the gland can restore its functions much faster.
Diet
Diet 8 table
- Efficiency: weight loss to the required level
- Time frame: long-term, until the expected effect is achieved
- Cost of products: 1120 - 1230 rubles per week
Fatty infiltration of the organ has a direct connection with nutrition, so diet takes a leading place in treatment. For patients with normal weight, the main goal of nutrition is to reduce the load on the gland, so Diet No. 5 . In case of obesity, it is important to reduce weight, so the basic principles of nutrition of table No. 5 are preserved, but in addition, patients are recommended to reduce calories by reducing fats and carbohydrates ( Diet 8 table ), while the diet should contain a normal amount of proteins. Daily calorie content is no more than 1500-1700 kcal. In case of disruption of the endocrine function of the gland, dietary Table No. 9 with a significant restriction of carbohydrates.
Saturated fats and fructose cause the progression of steatohepatitis and steatopancreatitis . At the same time, choline, a protein diet, unsaturated fats and antioxidants have a preventive effect. With lipomatous lesions of the pancreas, the digestion of dietary fat worsens. In the diet of such patients, the fat quota is reduced, and given the obesity of all patients suffering from this disease, this is all the more necessary. It is also important to avoid heating fats, since the substances formed when heating fats are difficult to digest. High-calorie, fatty, fried foods and smoked foods are excluded from the diet. At the same time, phospholipids, fat-soluble vitamins and omega-3 fatty acids are additionally introduced.
Dishes should be easily digestible, low-fat and steamed or baked. Such dishes do not require stress on the enzyme systems of the gastrointestinal tract. Recommended are cereal and vegetable puree soups, vegetable purees, stewed vegetables, meat and fish balls, boiled meat, steamed cutlets, non-sour cottage cheese, curd casseroles, omelettes, and fermented milk products. The volume of dishes should not cause discomfort. To prevent flatulence , dishes made from legumes and white cabbage are excluded.
Carbohydrates are the second component of nutrition, an excess of which in the diet leads to impaired lipid metabolism and the development of fatty infiltration of the pancreas. In this regard, the consumption of simple carbohydrates and sugary drinks is significantly limited. It has been established that sucrose and fructose influence the development of fatty infiltration of organs - they increase lipogenesis, cause insulin resistance and hypertriglyceridemia .
Malt and maltodextrose are widely used in the food industry (confectionery, dairy products, sauces), and their glycemic index is higher than sugar. If carbohydrate metabolism is impaired, carbohydrates should be evenly distributed throughout the day to avoid sudden fluctuations in glucose levels. Sources of carbohydrates for such patients are whole grain cereals (buckwheat, oatmeal), bran and whole grain bread, unsweetened berries and fruits, baked apples.
The third main point of nutrition is to avoid drinking alcoholic beverages!
Prevention
Primary prevention of this disease includes:
- A balanced diet that prevents weight gain.
- Elimination of alcohol, which is one of the risk factors for steatosis of the liver and pancreas.
- An active lifestyle, which is the prevention of obesity and metabolic syndrome.
- If the disease occurs, it is important to adhere to a low-calorie diet that promotes weight loss. A weight loss of even 8% leads to a significant reduction in pancreatic fat. A healthy lifestyle and avoiding alcohol consumption are also important.
Pancreatic fibrolipomatosis: defining terms
Fibrolipomatosis is one of the diseases that are combined under the general term “pancreatitis”. However, this condition cannot be clearly called a disease, even though doctors enter it in the “diagnosis” column. Why does such an incident arise? Let's try to figure this out without delving into medical terminology and speaking in a language understandable to non-medics.
Ultrasound diagnostics is aimed primarily at checking and assessing several mandatory organ parameters:
- location in the abdominal cavity (if we are talking about this type of ultrasound);
- shapes and sizes;
- structure and degree of tissue homogeneity, that is, the so-called echogenicity.
If the background of the last parameter deviates in any direction, this gives the specialist reason to talk about diffuse changes. Consequently, such a conclusion cannot be called a diagnosis, since it is only a kind of guideline for the doctor and allows him to determine the uniformity of pathological changes. Thus, pancreatic fibrolipomatosis can in no way be considered either a diagnosis itself or a sign or symptom of another disease. Its main task is only to indicate the presence of changes in the tissues of the organ, respectively, of a fibrous nature.
Consequences and complications
The following complications of pancreatic lipomatosis are possible:
- Development of insulin resistance and metabolic syndrome.
- High risk of diabetes mellitus , since the accumulation of fat in the islets of the gland reduces the number and functional activity of β-cells, which leads to impaired carbohydrate metabolism.
- Generalized atherosclerosis .
- Acute pancreatitis .
- Development of adenocarcinoma of the gland. Many scientists believe that it is likely that cancer of this organ will develop as a result of fatty infiltration. They draw an analogy with fatty liver, the outcome of which is hepatocellular carcinoma .
Forecast
Lipomatosis is a chronic, slowly progressive disease that ends with fibrosis of the gland tissue. The danger of the disease lies in the reduction of functional cells. The main goal of treatment is to stop progression. With adequate treatment, elimination of risk factors and lifestyle changes, the prognosis is favorable. If the recommendations are followed, the progression of fatty changes in the gland often stops and does not reach pronounced changes in the organ.
List of sources
- Ivashkin V.T. Pancreatic steatosis and its clinical significance // Ros. Journal of gastroenterology, hepatology, coloproctology. 2006. T. 16. No. 4. P. 32–37.
- Bokova T. A., Ursova N. I. Morphofunctional state of the pancreas in children and adolescents with obesity and metabolic syndrome // Experimental and clinical gastroenterology. 2008. No. 7. pp. 24–29.
- Ivashkin V.T., Shifrin I.A., Sokolina I.A. Chronic pancreatitis, pancreatic steatosis and steatopancreatitis. M.: Litterra, 2014. 240 p.
- Kucheryavyi Yu.A., Moskaleva A.B., Maev I.V. Baranskaya E.K., Sviridova A.V. The relationship of chronic pancreatitis with fatty liver disease and carbohydrate metabolism disorders in obese patients // Effective pharmacotherapy. 2011, no. 6. pp. 44–48.
- Kosyura S.D., Pavlovskaya E.V., Starodubtseva A.V. Damage to the pancreas in obesity // Medical Affairs. 2006. No. 3 P.23-26
Intraductal papillary mucinous tumor
According to the diagnostic criteria established by the World Health Organization, intraductal papillary mucinous tumor resembling pancreatic polyp is an intraductal mucin-producing neoplasm that affects the main pancreatic duct or branches of the organ. Its epithelial lining is formed by tall columnar epithelium with or without papillary projections.
The tumor grows intraepithelially along the pancreatic ducts. The neoplasm is characterized by segmental or diffuse expansion of the ductal system of the organ. It marks the proliferation of mucin-producing cells that form papillae on the surface of the epithelial plate, which externally resemble a polyp. The size of the papillae can range from microscopic forms to large nodular masses. When polyp-shaped papillae-polyps reach a size of 4 mm or more, pancreatic cancer develops in 88% of cases.