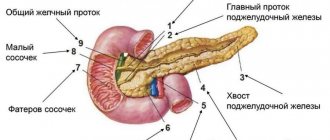
Features of the gland structure
The pancreas is an important digestive organ.
The pancreas is an elongated organ located towards the back of the abdominal cavity and extends slightly into the area of the left hypochondrium. The organ includes three parts: head, body, tail.
Large in volume and extremely necessary for the functioning of the body, the gland produces external and intrasecretory work.
Its exocrine region has classic secretory sections, the ductal part, where the formation of pancreatic juice necessary for the digestion of food, the decomposition of proteins, lipids, and carbohydrates occurs.
The endocrine region includes the pancreatic islets, which are responsible for the synthesis of hormones and control of carbohydrate-lipid metabolism in the body.
An adult normally has a head of the pancreas measuring 5 cm or more, the thickness of this area is within 1.5-3 cm. The width of the body of the gland is approximately 1.7-2.5 cm. The tail part can be up to 3.5 cm in length. 5 cm, and up to one and a half centimeters in width.
The entire pancreas is covered with a thin capsule of connective tissue.
The mass of the pancreatic gland of an adult is in the range of 70-80 g.
Endocrine system - functions. How the endocrine system works
The content of the article
The job of the endocrine system is to control all physiological functions of the body. This complex network of glands located in different parts of the body is responsible for homeostasis - internal balance.
Endocrine system
Along with the nervous system and regulation at the tissue level, the endocrine system forms a highly specialized internal “processor” that controls all our vital parameters. When any part of the hormonal computer goes wrong, we immediately feel it.
What are the symptoms of hormonal disorders? Unpleasant sensations may arise from various organs; it also happens that other glands try to take over the functions of those that have stopped working properly.
Hormone preparations
Pancreatic hormone preparations have traditionally been described for the purpose of considering treatment regimens for diabetes mellitus.
The problem of pathology is a violation in the ability of glucose to enter the body's cells. As a result, there is an excess of sugar in the bloodstream, and an extremely acute deficiency of this substance occurs in the cells.
A serious disruption occurs in the energy supply of cells and metabolic processes. Treatment with drugs has the main goal of stopping the described problem.
Classification of antidiabetic drugs
Insulin medications are prescribed by the doctor individually to each patient.
Insulin medicines:
- monosulin;
- Insulin-semilong suspension;
- Insulin-long suspension;
- Insulin-ultralong suspension.
The dosage of the listed drugs is measured in units. The dose calculation is based on the concentration of glucose in the bloodstream, taking into account that 1 unit of the drug stimulates the removal of 4 g of glucose from the blood.
Supphonyl urea derivatives:
Pituitary gland - pituitary hormones (prolactin, endorphins, ACTH hormone and TSH hormone
The pituitary gland stimulates the growth of long bones and body growth, regulates metabolism, is responsible for the secretion and maintenance of milk in nursing mothers, stimulates the breakdown of excess fat, and also influences the development and function of the testes or ovaries. The pituitary hormones it produces include prolactin, endorphins, ACTH hormone and TSH hormone.
Pituitary hormones
How to take medications correctly
There are a number of rules that are important to follow when taking medications:
- The medicine is prescribed by a doctor, indicating the individual dosage and duration of therapy.
- During the period of treatment, it is recommended to follow a diet: exclude alcoholic beverages, fatty foods, fried foods, and sweet confectionery products.
- It is important to check that the prescribed medicine has the same dosage as indicated in the prescription. It is forbidden to split pills or increase the dosage yourself.
- If side effects occur or there is no result, you must notify your doctor.
Thyroid gland - thyroid hormones (thyroxine, triiodothyronine, calcitonin)
Thyroid hormones affect the functioning of the entire body, and the most important of them are: triiodothyronine (FT3), free thyroxine (FT4), calcitonin.
The thyroid gland is regulated by thyrotropin (TSH), produced by the pituitary gland, as well as hyperthyroidism and hypothyroidism, including Hashimoto's disease, one of the most common hormonal disorders today.
Hormonal disorders
All alarming symptoms that may indicate dysfunction of one or more endocrine glands should be reported to an endocrinologist. In any case, only this doctor treats such disorders, and when contacting another specialist, he will still redirect the patient to a hormonal specialist - an endocrinologist.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
How do you donate blood for hormones?
A blood test for hormones is the most revealing and informative method for detecting any pathologies in the functioning of the endocrine glands. However, it is important to take into account that many factors influence hormonal levels: time of day, menstrual cycle in women, taking medications. For this reason, preparing for hormonal tests should be taken very seriously. If this is neglected, the result of the analysis may be incorrect and, at best, it will have to be retaken, and at worst, based on it, an incorrect diagnosis may be made and the wrong treatment may be prescribed, which can lead to irreparable consequences.
To prepare for donating blood for hormones, you must follow the following general rules:
- On the eve of the test, you should avoid physical activity, try to avoid stressful situations, stop any physiotherapeutic procedures, avoid taking oral contraceptives, drinking alcohol, fatty foods and foods containing iodine. It is also recommended to reschedule ECG, ultrasound, and x-ray examination until after the test.
- An important point is taking medications - you must notify the doctor who prescribed the hormonal blood test about the fact that you are taking medications. He will decide whether to stop or continue taking medications during the test.
- A hormonal test is taken strictly on an empty stomach. Therefore, it is recommended to refrain from eating 12 hours before blood collection.
- In the morning, before the analysis, it is forbidden to chew gum, drink tea and smoke.
- Immediately before donating blood, you should rest for 15-10 minutes.
- Women need to take into account their menstrual cycle, because... It is possible to test blood for some hormones only during certain periods of this cycle.
- To track the dynamics of the levels of certain hormones, a repeat analysis is required. It is handed over at approximately the same time as the previous one, in compliance with all the above rules.
Blood sampling for analysis is carried out in the morning. The biomaterial is taken from the ulnar vein.
DIAGNOSTICS OF PANCREAS FUNCTION
LIST OF STUDIES:
- Insulin (IRI)
- Autoantibodies to insulin A-IAA
- C-peptide
- Leptin (eating behavior hormone)
- Glycosylated hemoglobin (HbA1C)
- Cholesterol
- Cholesterol-HDL
- LDL cholesterol
Leptin
Hormone that regulates energy metabolism and body weight
Leptin is a peptide hormone that is secreted by fat cells and is thought to be involved in the regulation of body energy metabolism and body weight. It reduces appetite, increases energy expenditure, alters fat and glucose metabolism, and neuroendocrine function either by direct influence or by activation of specific structures in the central nervous system.
The level of leptin in the blood increases with increasing obesity and decreases with a decrease in the amount of adipose tissue. Normally, an increase in leptin levels suppresses the secretion of neuropeptide Y in the hypothalamus, which is involved in the formation of hunger, and stimulates the activity of the sympathetic nervous system. A decrease in leptin levels after significant weight loss causes an increase in appetite and subsequent weight (body weight) restoration.
Changes in leptin levels are associated with the mechanisms of development of amenorrhea caused by anorexia nervosa, bulimia nervosa, as well as excessive physical activity in female athletes. In these situations, leptin levels are reduced.
It is assumed that leptin concentration plays the role of a physiological signal about the sufficiency of the body's energy resources to perform the reproductive function and affects steroidogenesis in the ovaries. During puberty, the concentration of leptin in the blood increases.
Genetic deficiency of leptin (the synthesis of which is associated with the ob-gene - the obesity gene) in rare cases of hereditary leptin deficiency in humans causes morbid obesity, which can be treated with the use of exogenous leptin.
In other cases, obese people are characterized, on the contrary, by an increase in leptin concentration, which is not accompanied by a corresponding change in eating behavior and energy metabolism. Presumably, this is due to “leptin resistance,” which is associated with impaired transport of the hormone by transport proteins or soluble leptin receptors. Currently, it is considered as one of the factors in the pathogenesis of non-insulin-dependent diabetes mellitus. Excess leptin leads to suppression of insulin secretion, causes resistance of skeletal muscles and adipose tissue to its effects, suppresses the effect of insulin on liver cells, which leads to an even greater increase in glucose levels in type II diabetes.
However, obesity itself does not lead to diabetes with normal pancreatic function.
In addition, high leptin levels create a high likelihood of thrombosis. Research shows that a blood clot begins to form as a result of a special interaction between leptin and its receptors located on platelets, the cells responsible for blood clotting.
It has been established that the connection between the amount of leptin and diseases of the cardiovascular system exists regardless of other risk factors such as smoking, high cholesterol and high blood pressure.
Indications for the purpose of analysis:
- Suspicion of genetic leptin deficiency (previous occurrence of severe obesity);
- In a complex of studies on the problems of weight gain or loss;
- Reproductive function disorders due to reduced nutrition and excessive physical activity;
- In a complex of studies related to the identification of risk factors for cardiovascular diseases;
- Differential diagnosis of type II diabetes mellitus and obesity;
- Recurrent thrombosis.
Preparing for analysis:
At least 8 hours pass between the last meal and blood collection (preferably at least 12 hours). Juice, tea, coffee (especially with sugar) are not allowed. You can drink water.
Material: serum or blood plasma (without hemolysis and lipemia).
Units of measurement: Units of measurement in BioTest: ng/ml.
Reference values: Adults: Women – 1.1 – 27.6 ng/ml; Men – 0.5 – 13.8 ng/ml.
Increased leptin values:
- Obesity, non-insulin-dependent diabetes mellitus;
- Enhanced nutrition.
Decreased leptin values:
- Starvation;
- Weight loss; (body weight);
- Obesity associated with genetic leptin deficiency.
C-Peptide
Biologically inactive marker of carbohydrate metabolism, an indicator of endogenous insulin secretion.
C-peptide is a stable fragment of endogenously produced proinsulin, “cut off” from it during the formation of insulin. The level of C-peptide corresponds to the level of insulin produced in the body.
In the proinsulin molecule between the alpha and beta chains there is a fragment consisting of 31 amino acid residues. This is the so-called connecting peptide or C-peptide. During the synthesis of the insulin molecule in the beta cells of the pancreas, this protein is excised by peptidases and, together with insulin, enters the bloodstream. Until the C-peptide is removed, insulin is not active. This allows the pancreas to store insulin in the form of a pro-hormone. Unlike insulin, C-peptide is biologically inactive. C-peptide and insulin are secreted in equimolar quantities, so determining the level of C-peptide allows assessing insulin secretion.
It should be noted that although the amount of C-peptide and insulin molecules formed during secretion into the blood is the same, the molar concentration of C-peptide in the blood is approximately 5 times higher than the molar concentration of insulin, which is apparently due to different rates of elimination of these substances from the bloodstream . Measuring C-peptide has several advantages over measuring insulin: The half-life of C-peptide in the circulation is longer than that of insulin, so C-peptide levels are a more stable indicator than insulin concentrations. In immunological analysis, C-peptide does not cross-talk with insulin, so measurement of C-peptide makes it possible to assess insulin secretion even while taking exogenous insulin, as well as in the presence of autoantibodies to insulin, which is important when examining patients with insulin-dependent diabetes mellitus.
The level of C-peptide changes in accordance with fluctuations in the level of insulin produced endogenously. The ratio of these indicators may change against the background of liver and kidney diseases, since insulin is metabolized primarily by the liver, and the metabolism and excretion of C-peptide is carried out by the kidneys. In this regard, the determination of this indicator may be useful for the correct interpretation of changes in insulin levels in the blood in cases of liver dysfunction.
Indications for the purpose of analysis:
- Differential diagnosis of diabetes types 1 and 2;
- Prediction of the course of diabetes mellitus;
- Infertility, polycystic ovary syndrome;
- Differential diagnosis of hypoglycemic conditions;
- Suspicion of artificial hypoglycemia;
- Assessment of residual beta cell function in diabetics during insulin therapy;
- Detection and control of remission (juvenile diabetes);
- Diagnosis of insulinoma;
- Assessment of possible fetal pathology in pregnant women with diabetes;
- Assessment of insulin secretion in liver diseases;
- Control after removal of the pancreas.
Preparation for the study: on an empty stomach.
- Material for research: serum.
- Determination method: solid-phase chemiluminescent immunoassay.
- Units of measurement and conversion factors: Units of measurement in the BioTest laboratory - pmol/l
- Alternative units of measurement are ng/ml; Unit conversion: ng/ml x 331 ==> pmol/l
Reference values: 298-1324 pmol/l
Increased C-peptide levels:
- Beta cell hypertrophy;
- Insulinoma;
- Antibodies to insulin;
- Non-insulin-dependent diabetes mellitus (IDDM type II);
- Hypoglycemia when taking oral hypoglycemic drugs (sulfonylurea derivatives);
- Somatotropinoma;
- APUDhome;
- Kidney failure; 9. Eating; 10. Taking medications containing estrogens, progesterone, glucocorticoids, chloroquine, danazol, ethinyl estradiol, oral contraceptives.
Decrease in C-peptide levels:
- Insulin-dependent diabetes mellitus (IDDM type I);
- Insulin therapy (normal reaction of the pancreas in response to the administration of exogenous insulin);
- Alcoholic hypoglycemia;
- State of stress;
Antibodies to insulin receptors (for insulin-resistant type II diabetes mellitus).
Glycated hemoglobin (HbA1c)
A combination of hemoglobin with glucose, which allows one to assess the level of glycemia 1-3 months prior to the study.
It is formed as a result of the slow non-enzymatic addition of glucose to hemoglobin A contained in red blood cells. Glycated (the term “glycosylated” is also used) hemoglobin is present in the blood of healthy people.
The rate of this reaction and the amount of glycated hemoglobin formed depend on the average level of glucose in the blood over the life of red blood cells. As a result of the reaction, several variants of glycated hemoglobins are formed: HbA1a, HbA1b, HbA1c. The latter form predominates quantitatively and gives a closer correlation with the severity of diabetes mellitus.
Glycated hemoglobin reflects hyperglycemia that occurred during the life of red blood cells (up to 120 days). Red blood cells circulating in the blood have different ages. Usually they focus on an average period of 60 days. The level of glycated hemoglobin is an indicator of compensation of carbohydrate metabolism during this period. Normalization of the level of glycated hemoglobin in the blood occurs 4-6 weeks after reaching normal glucose levels. In patients with diabetes mellitus, the level of this compound can be increased by 2-3 times.
In accordance with WHO recommendations, this test is considered optimal and necessary for the control of diabetes mellitus. Patients with diabetes are recommended to test their glycated hemoglobin levels at least once a quarter.
Values may vary between laboratories depending on the analytical method used, so monitoring over time is best done in the same laboratory or at least using the same method. When monitoring diabetes treatment, it is recommended to maintain glycated hemoglobin levels below 7% and review therapy when glycated hemoglobin levels exceed 8% (these values apply only to certified methods for determining glycated hemoglobin with reference limits of 4-6%).
Clinical studies using certified methods show that a 1% increase in glycated hemoglobin is associated with an average increase in plasma glucose levels of approximately 2 mmol/L. Glycated hemoglobin is used as an indicator of the risk of developing diabetes complications. It has been proven that a decrease in glycated hemoglobin values by 1/10 is associated with an approximately 45% reduction in the risk of progression of diabetic retinopathy.
Test results may be falsely affected by any condition that affects the average lifespan of red blood cells. Bleeding or hemolysis causes a false decrease in the result; blood transfusions naturally distort the result; in iron deficiency anemia, a false increase in the result of determining glycated hemoglobin is observed.
Indications for the purpose of analysis
Long-term monitoring of the course and control over the treatment of patients with diabetes mellitus to determine the degree of compensation of the disease.
Preparing for the study
It is advisable to take blood samples on an empty stomach. The study is not advisable to conduct after bleeding or blood transfusions.
- Material for research: whole blood with anticoagulant (EDTA).
- Determination method: borate method.
- Execution time: 1 working day.
- Units of measurement and conversion factors: units of measurement in the BioTest laboratory are % of the total amount of hemoglobin.
- Reference values: 4.5-6.5% of the total hemoglobin content.
Increased HBA1c values:
- Diabetes mellitus and other conditions with impaired glucose tolerance.
- Iron deficiency.
- Splenectomy. A false increase may be due to a high concentration of fetal hemoglobin (HbF).
Decrease in HBA1c values:
- Hypoglycemia.
- Hemolytic anemia.
- Bleeding.
- Blood transfusion.
Acute pancreatitis.
Acute pancreatitis is an acute inflammation of the pancreas.
Acute pancreatitis usually appears against the background of a person’s abuse of alcoholic beverages and previous alcohol poisoning.
Acute pancreatitis can also be caused by:
- improper or poor quality nutrition (eating fatty, spicy foods, frequent overeating);
- urolithiasis – the presence of kidney stones;
- heredity;
- trauma to the pancreas: previous operations, injuries, mechanical damage;
- uncontrolled use of medications, antibiotics;
- endocrine diseases, hormonal disorders.
- infections and viruses.
Symptoms of acute pancreatitis in Nizhny Novgorod.
The main symptom of pancreatitis is acute pain in the epigastric region, hypochondrium (right and left). Over time, the pain begins to become encircling, affecting the back, lower and lateral areas of the abdomen.
Detection of acute pancreatitis in Nizhny Novgorod.
If you suspect the development of pancreatitis in the body, the gastroenterologist prescribes the following set of examinations:
- a general blood test, which allows you to find out about the presence of an inflammatory process;
- Ultrasound of the abdominal cavity, which allows you to see changes in the internal organs;
- a general urinalysis to detect amylase in the urine, the presence of which indicates the development of pancreatitis;
- FGDS.
Adrenal glands
The adrenal glands are paired organs of the endocrine system located directly above the kidneys. The main hormones synthesized by them are:
- Adrenaline is a fear hormone that is synthesized when a person finds himself in a stressful situation and also feels a threat to life. It provides instant mobilization of the body, which leads to a short-term increase in physical capabilities.
- Aldosterone - is involved in the regulation of water-salt metabolism, as it promotes the retention of sodium and water, but stimulates the excretion of potassium.
- Corticosteroids are represented by cortisol, cortisone and corticosterone. All of them have a powerful anti-inflammatory effect and can affect the entire body. They also take part in maintaining normal blood sugar levels, due to its breakdown and storage by the body in the liver in the form of glycogen, as well as muscle tone and blood pressure.
The functioning of the adrenal glands is controlled by the pituitary gland and hypothalamus.