Colon tumors are benign and malignant neoplasms. They grow from the tissue covering of the large intestine and are based in its various parts. The cells of the mucous layer in the intestines tend to renew themselves. But sometimes they can carry out regenerative changes unevenly, giving rise to tumors.
In terms of prevalence, after lung cancer and stomach cancer, malignant tumors localized in the large intestine are in third place in the world.
Fact. In general cancer statistics, cancer of the rectal segment of the colon occurs in 10% of cases of the total number of pathologies. According to WHO, this is about 500 thousand patients with colorectal cancer every year. Dangerous neoplasms occur mainly in the population aged 40 to 60 years. Most often, this disease affects residents of Canada. Residents of Africa and Asian countries are less susceptible to such diseases.
Risk factors
- The likelihood of detecting a tumor in yourself increases if the medical history of relatives already includes colon polyposis;
- Unbalanced diet: satiety with fatty foods, lack of vegetable and fruit components, legumes, whole grain bread, buckwheat and corn in daily dishes;
- Frequent constipation, especially those that were eliminated after the use of laxatives that irritate the mucous surface of the intestinal layer;
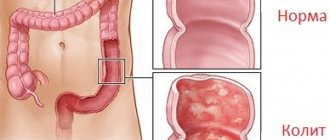
- Crohn's disease - inflammation of the colon mucosa with the appearance of numerous ulcers, diarrhea is much more pronounced than with ulcerative colitis, the presence of perianal lesions in the form of polyps and fistulas (inflammation in the recess of the anal mucosa, perirectal tissue or intersphincteric space);
- Hypodynamia - weakened motor tone;
- Age limit: over 50 years;
- Angiodysplasias are congenital malformations of blood vessels;
- Smoking;
- Nonspecific ulcerative colitis (UC) is a chronic diffuse inflammatory process of the mucous layer of the rectum and colon, which serves as an impetus for the formation of various ulcers of the mucous membrane.
Fact. The total length of the colon is approximately one and a half to two meters.
Benign tumors of the colon
- An intestinal polyp is a harmful formation that is raised above the mucous membrane in the form of a branched or rounded process located on a so-called “leg” like a mushroom, or on a broad base. They sometimes seem to “hang” into the intestinal lumen. Signs of polyps may include gastrointestinal hemorrhage or even intestinal obstruction;
- Glandular and glandular-villous adenomas of the colon - develop from intestinal epithelial cells, they are detected in 60-80% of patients with benign neoplasms of the colon;
- Cystic granulating (juvenile) - the largest polyps, can grow up to 2 cm. One of the central symptoms of these colon polyps is the presence of blood in the stool;
- Nonepithelial: lymphoid polyps, cystic pneumatosis intestinalis, carcinoid tumors, lipomas, metastatic lesions;
- Fibrous polyps of the anal canal are harmful formations of connective tissue that arise as a result of an inflammatory process or vascular dysfunction;
- Hyperplastic - occupy locations in the distal (farthest from the center) parts of the colon; they can arise as a result of a violation of the integrity of the muscle layer (when a high concentration of lymphocytes is observed in the muscle layer). They are often a continuation of the pathological development of ulcerative colitis;
- Diffuse polyposis of the colon is a hereditary lesion of the large intestine by polyposis with widespread destruction of adjacent parts of the gastrointestinal tract.
According to the areas of distribution, the following types of diffuse polyposis are distinguished:
- Classic, aimed at “disabling” the rectum;
- Associated with vascular defects;
- Gardner's syndrome, which involves the lesion not only in the intestines, but also in the soft tissues surrounding it;
- Peutz-Jeghers syndrome - completely destroys the functional abilities of the gastrointestinal tract, “gives itself away” as pigment spots on the cheeks and around the mouth;
- Villous tumors are round or oval-shaped formations, the surface of which is covered with a kind of “lint” of blood vessels and connective tissue, sometimes formed into “nodules”;
- Leiomyoma is a derivative of smooth muscle;
- Lipoma is a derivative of adipose tissue, often present in the subcutaneous tissue, but can also occur in internal organs that are supplied with a fatty layer.
COLON TUMORS
12.11.12
Diagnosis of the disease
To diagnose colon tumors, X-ray examination (irrigoscopy), endoscopic examination (colonoscopy), digital and endoscopic examination of the rectum (sigmoidoscopy) are used.
Clinical manifestations of colon cancer
Clinical manifestations of colon cancer largely depend on the location of the malignant neoplasm, the degree of spread of the tumor process and the presence of complications aggravating the course of the underlying disease.
The most common symptoms: abdominal pain, impaired motor-evacuation function of the intestine, clinically manifested by alternating constipation and diarrhea, pathological discharge with feces, changes in the general condition of the patient and, finally, a tumor palpable through the anterior abdominal wall.
Abdominal pain is the most common symptom of colon cancer and is observed in almost 80% of patients. In clinical observations with right-sided tumor localization, pain, as one of the first symptoms of cancer, occurred 2-3 times more often than with cancer of the left half. This fact is explained by a violation of motor function: pendulum-like movement of intestinal contents from the small intestine to the cecum and back.
Spasmodic contractions of the intestine, pushing feces through the intestinal lumen partially blocked by the tumor, cause pain. Intratumoral and perifocal inflammation of the intestinal wall, often accompanying disintegrating infected tumors, aggravates pain.
Colon tumors can occur for a long time without pain, and only when the tumor spreads beyond the intestinal wall, when moving to the peritoneum and surrounding organs, pain appears, the intensity and frequency of which may vary. Depending on the location of the tumor, the pain syndrome can simulate chronic appendicitis, cholecystitis, gastric and duodenal ulcers, and chronic adnexitis.
Malignant neoplasms of the right half of the colon are characterized by a combination of pain, hyperthermic reaction (increase in temperature), leukocytosis and rigidity (tension) of the muscles of the anterior abdominal wall . The clinical manifestations of the disease resemble destructive appendicitis, and the correct diagnosis can only be established during an inspection of the abdominal organs during surgery. An analysis of the clinical course of cancer of the right half of the colon showed that in almost 60% of cases the presence of a tumor is accompanied by pain in the right abdomen, intestinal disorders, hyperthermia, symptoms of intoxication and anemia.
This combination of clinical symptoms is characteristic of the toxic-anemic form of colon cancer.
Violations of the motor-evacuation function of the colon lead to stagnation of intestinal contents and cause symptoms of discomfort such as a feeling of heaviness in the abdomen, loss of appetite, and nausea. An important role in the development of intestinal discomfort is played by reflex functional disorders of other organs of the digestive system. Absorption of decay products by the inflamed mucous membrane, a change in the normal composition of the intestinal microflora, accompanied by the appearance of pathogenic strains that secrete exo- and endotoxins, leads to the development of endogenous intoxication syndrome. Functional disorders of the gastrointestinal tract in patients with colon cancer are manifested by impaired passage of contents, constipation, bloating, and paroxysmal pain.
The accumulation of feces above the tumor is accompanied by increased processes of putrefaction and fermentation, leading to bloating with retention of stool and gases.
In cases where the course of the tumor process is complicated by the development of intestinal obstruction, the clinical picture of patients with colon cancer is dominated by symptoms such as bloating with difficulty passing feces and gases, nausea, belching, and vomiting. The pain is paroxysmal in nature. According to some authors, when a malignant tumor is localized in the left half of the colon, the stenotic nature of tumor growth leads to a narrowing of the intestinal lumen, as a result of which feces, accumulating above the tumor, can be palpated through the abdominal wall and are sometimes mistaken for a tumor.
One of the fairly common and relatively early clinical manifestations of colon cancer is pathological discharge from the rectum . These include mucus, blood, pus, tumor masses, etc. Most often, pathological impurities in stool are noted when the colon tumor is located on the left side, rather than when the tumor is located in the right half (62.4% and 18.5%, respectively). Discharges of pus and fragments of tumor masses, indicating the addition of an inflammatory process leading to tumor disintegration, infection and the formation of perifocal and intratumoral abscesses, are noted much less frequently. In any case, the presence of such discharge quite often indicates a widespread tumor process.
One of the symptoms indicating an advanced tumor process is a tumor palpable through the abdominal wall. The frequency of this symptom ranges from 40 to 60%.
Any of the symptoms listed above (pain, intestinal disorders, the presence of pathological impurities in the stool) can be present with any intestinal disease, not just tumors. Analysis of the clinical course of colon cancer indicates a significant percentage of diagnostic errors (up to 35%), leading to hospitalization in general therapeutic and infectious diseases clinics for the treatment of anemia of unknown etiology, dysentery, etc. The percentage of patients hospitalized in general surgical hospitals for emergency indications at altitude remains high obstructive intestinal obstruction.
The following clinical forms of colon cancer are distinguished:
- toxic-anemic, characterized by varying degrees of severity of anemia, general symptoms, intoxication;
- obstructive – characterized by the appearance of signs of intestinal obstruction and accompanied by paroxysmal abdominal pain, rumbling and increased peristalsis, stool retention and poor passage of gases;
- enterocolitic form, accompanied by bloating, alternating diarrhea with constipation, the presence of pathological impurities in the stool, dull, aching pain in the abdomen;
- pseudo-inflammatory form, characterized by low severity of intestinal disorders against the background of signs of an inflammatory process in the abdominal cavity;
- tumor (atypical) form, which is not characterized by general symptoms, intestinal obstruction, with a palpable tumor in the abdominal cavity;
- dyspeptic form, the characteristic features of which are symptoms of gastric discomfort (nausea, belching, feeling of heaviness in the epigastric region), accompanied by pain localized mainly in the upper floor of the abdominal cavity.
It must be emphasized that the identification of clinical forms is, to a certain extent, conditional and mainly characterizes the leading symptom complex. However, knowledge of the manifestations of colon cancer allows us to suspect the presence of a tumor even in cases where the disease occurs with mild intestinal disorders.
Complicated forms of colon cancer
Complications that quite often accompany colon cancer and have a direct impact on the course of the disease and the prognosis of the tumor process include intestinal obstruction of varying severity, perifocal inflammatory process, tumor perforation, intestinal bleeding, as well as tumor spread to surrounding organs and tissues.
According to the literature, the incidence of intestinal obstruction in patients with colon cancer ranges from 10 to 60%. Such pronounced differences in the frequency of this complication are largely due to the fact that the vast majority of patients with a complicated course of the tumor process end up in emergency surgical hospitals, and not in specialized medical institutions.
The clinical course of the disease largely depends on the severity of intestinal obstruction. In case of a decompensated form of intestinal obstruction (severe bloating with retention of stool and gases, vomiting, cramping pain throughout the abdomen against the background of severe metabolic disorders), emergency surgical intervention is indicated, the volume and nature of which depends not only on the location of the tumor, but also on the severity of the developed complications. In cases of compensated form of obstructive intestinal obstruction, conservative measures are often effective in preparing the patient for planned surgery.
The passage of liquid intestinal contents persists when the intestinal lumen narrows to 0.8-1 cm; with cancer of the right half of the colon, ileus (intestinal obstruction) usually occurs with large tumor sizes. As stenosis progresses, an expansion of the intestine above the tumor is formed, leading to the accumulation of feces and the appearance of aching pain in the abdomen, at times cramping and spastic in nature.
When the tumor is localized in the left parts of the colon, the development of intestinal obstruction is often preceded by constipation, alternating with copious foul-smelling loose stools. In cases of decompensated intestinal obstruction, the dysfunction of the gastrointestinal tract organs is quickly joined by metabolic disorders, leading to disruption of the vital functions of organs and systems.
Intratumoral and perifocal inflammatory processes pose a great danger in colon cancer. The frequency of such complications is quite high: from 12 to 35%.
Inflammatory changes in the tumor, caused by the presence of a large number of virulent microorganisms in the intestinal contents, the qualitative and quantitative composition of which changes with the disintegration of tumor tissue, lead to infection and the formation of inflammatory infiltrates and ulcers.
In most clinical observations, histological examination of removed specimens in patients with perifocal inflammatory process revealed ulceration of the tumor and signs of acute purulent inflammation with the formation of abscesses, necrosis and fistulas in the thickness of the adipose tissue, tumor stroma or lymph nodes.
Perforation of the intestinal wall and bleeding from a disintegrating tumor are the most dangerous complications of this disease. Long-term stasis of intestinal contents against the background of chronic intestinal obstruction in combination with trophic disorders of the intestinal wall lead to the formation of bedsores and perforation.
The most unfavorable prognosis is tumor perforation into the free abdominal cavity, leading to diffuse fecal peritonitis. When a segment of intestine devoid of peritoneal cover is perforated, an acute purulent focus forms in the retroperitoneal space. In a number of patients, the pinpoint perforation is covered by the omentum or a nearby organ, leading to the formation of a perifocal inflammatory process that spreads to nearby organs and tissues. Perifocal and intratumoral inflammation, complicating the course of the underlying disease on the one hand, and perforation of a colon tumor on the other, are parts of the same pathological process, which is based on infection of the affected part of the colon with conditionally pathogenic strains of microorganisms penetrating through the pathologically altered intestinal wall .
Diagnostics
Improving the methods of clinical examination of a patient using modern X-ray and endoscopic techniques, and the use of a wide arsenal of screening diagnostic methods, until recently, have not significantly improved the early detection of colon cancer. More than 70% of patients with colon cancer at the time of hospitalization had stages III and IV of the disease. Only 15% of them consulted a specialist within 2 months from the onset of the first symptoms of the disease. In less than half of the examined patients, the diagnosis was established within 2 months from the onset of the disease, and in every fourth case it took more than six months to determine the nature of the disease. Quite frequently occurring diagnostic errors led to unnecessary surgical interventions and physiotherapeutic procedures leading to dissemination of the tumor process.
The diagnosis of colon cancer is made on the basis of x-ray and endoscopic examinations. An equally important method of physical examination of the patient is palpation of the abdomen, which allows not only to identify a tumor in the abdominal cavity, but also to evaluate its consistency, size, and mobility.
According to a number of authors, in 60-70% of cases, a colon tumor is palpable.
Types of studies
- X-ray examination, along with colonoscopy, is leading in the diagnosis of colon cancer.
- Irrigoscopy allows you to obtain information about the localization of the tumor, determine the extent of the lesion, determine the form of tumor growth, assess its mobility, and sometimes judge the relationship with other organs. When performing irrigoscopy, it is also possible to identify synchronous tumors of the colon. The last circumstance is also important because with the stenosing nature of the growth of the neoplasm, endoscopic examination does not allow assessing the condition of the overlying parts of the colon before surgery.
- Endoscopic examination, along with visualization of a malignant tumor, allows one to obtain material for histological examination, which is a necessary attribute of the preoperative diagnosis of a malignant neoplasm.
- The simplest and most widespread method of endoscopic examination of the colon is sigmoidoscopy, in which it is possible to assess the condition of the lower part of the intestinal tube. When performing sigmoidoscopy, the researcher assesses the condition of the colon mucosa, vascular pattern, the presence of pathological impurities in the intestinal lumen, elasticity and mobility of the intestinal wall. When a colon tumor is detected, its size, appearance, consistency, mobility during instrumental palpation are studied, and a biopsy is performed.
Determining the degree of spread of the tumor process
The program for examining the patient before surgery, in addition to the traditional methods already listed, includes special x-ray and radioisotope studies.
Hematogenous metastasis is based on the process of embolization by cancer cells of the venous outflow pathways from the organ affected by the tumor process. Penetration of tumor cells into venous vessels occurs as a result of invasion and destruction of the vessel wall by the tumor. The bulk of venous blood in patients with colorectal cancer enters the portal vein through the system of the inferior and superior mesenteric veins, which explains the fact that distant metastases are mainly localized in the liver.
Ultrasound examination is widely used to assess the extent of tumor spread. It is based on the principle of recording a reflected ultrasonic wave from the interfaces of tissues that differ in density and structure. Having high resolution and information content, ultrasound is a practically harmless diagnostic method that allows you to visualize tumor nodes measuring 0.5-2.0 cm.
The anatomical and topographic structure of the liver and the good propagation of ultrasound in it determine the high information content of the study. It is important that ultrasound helps to determine not only the nature of pathological changes in the liver, but also to establish the localization and depth of focal changes. When performing ultrasound tomography, a layer-by-layer image of the internal structure of the liver is obtained and pathological space-occupying formations or diffuse changes are identified. Ultrasound of the liver can be repeated quite often without harm to the patient’s body, which makes it possible to evaluate the results of the treatment.
The use of X-ray computed tomography (CT) in medicine has contributed to significant improvements in the diagnosis of various pathological conditions.
Computed tomography has the following important advantages over other examination methods:
- presents an image of anatomical structures in the form of a cross section, excluding the combination of their images;
- provides a clear image of structures that differ slightly in density from each other, which is extremely important for diagnosis;
- provides an opportunity to quantitatively determine tissue density in each image area of the organ under study for differential diagnosis of pathological changes;
- It has a non-invasive diagnostic method, safety and low radiation exposure to the patient’s body.
According to the researchers, when analyzing the CT images of metastatic tumors of colorectal cancer, in 48% of cases the tumor nodes contained calcifications, and sometimes total calcification of metastatic tumors was revealed.
Radionuclide (isotope) methods for diagnosing and assessing the extent of colorectal cancer spread are used quite rarely in the daily practical work of medical institutions. One of these methods is positive scintigraphy, based on the use of specific drugs such as gallium in the form of a citrate complex, as well as bleomycin labeled with an indium isotope.
TREATMENT OF COLON CANCER
Choosing the type of surgical intervention and justifying its scope
The history of surgical treatment of colon cancer goes back more than 150 years. Reybard in 1833 performed the first resection of the colon for a malignant tumor with the formation of an interintestinal anastomosis. In Russia in 1886 E.V. Pavlov performed the first resection of the cecum for a malignant tumor with an anastomosis between the ascending colon and ileum . In contrast to manipulations on the small intestine, resection of the colon, according to V. Schmiden (1910), is one of the most important surgical interventions associated with the existence of such features as the presence of pathogenic microflora in the contents of a hollow organ, the absence of a mesentery in fixed areas of the colon intestines, a thinner layer of muscular tissue. These features of the colon predetermine increased demands on the reliability of the formation of interintestinal anastomoses, taking into account the anatomical features of various parts of the colon and the adequacy of the blood supply to the anastomosed segments.
The main disadvantage of these surgical interventions is the presence of a temporary colostomy - the removal of the intestine to the anterior abdominal wall. Therefore, in specialized oncoproctology clinics, the indications for performing two-stage surgical interventions are being rethought, considering them justified only in weakened patients with symptoms of decompensated intestinal obstruction.
The volume and nature of surgery for colon cancer depends on a number of factors, among which the most important are the location, extent of tumor spread, the presence of complications of the underlying disease, as well as the general condition of the patient.
Choosing the type of surgical intervention for complicated colon cancer
Most patients with colorectal cancer are admitted to specialized medical institutions in stages III and IV of the tumor process. Many of them experience various complications (obstructive form of intestinal obstruction, tumor perforation, bleeding and perifocal inflammatory process), often requiring emergency surgical intervention.
The results of surgical interventions in patients with complicated colorectal cancer depend to a certain extent on the qualifications of the operating surgeon, his ability to assess the degree and severity of the pathological process complicating the course of the underlying disease, and taking into account the general condition of the patient.
When choosing the type of surgical intervention, they strive not only to save the patient from an acute surgical complication, but also, if possible, to perform a radical operation.
One of the most dangerous complications of colon cancer is perifocal and intratumoral inflammation, often spreading to surrounding tissues. The frequency of this complication is quite high and ranges from 6% to 18%. This complication is manifested by the clinical picture of acute inflammation and intoxication, and the spread of the process to neighboring organs and surrounding tissues contributes to the formation of infiltrates, abscesses, and phlegmons. Often, a pronounced inflammatory process in the tumor and surrounding organs is interpreted as tumor infiltration, which is the reason for the inadequate scope of surgical intervention.
The presence of perifocal and intratumoral inflammation in colon cancer has a significant impact on the choice of the volume and nature of surgical intervention only in cases where the inflammatory process spreads to surrounding organs and tissues, and forces the use of combined surgical interventions.
Combined operations for colon cancer
Expanding the scope of surgical intervention due to the spread of a malignant tumor to nearby organs and tissues increases the duration of the operation, trauma and blood loss. Extension of the tumor beyond the intestinal wall indicates an advanced neoplastic process, but the absence of distant metastases makes it possible to perform a combined operation, which, while improving the quality of life of patients, eliminates severe complications of the tumor process and creates real preconditions for the use of specific methods of antitumor treatment.
Palliative surgical interventions in patients with colon cancer
Almost 70% of patients with colon cancer at the time of surgical intervention are diagnosed with stages III and IV of the disease, and in every third patient among those operated on, distant metastases are diagnosed, mainly in the liver and lungs. The development of intestinal obstruction forces one to resort to symptomatic surgical interventions - colostomy, formation of bypass anastomosis in patients with stage IV of the disease. However, more and more surgeons for advanced colorectal cancer prefer palliative resection or hemicolectomy .
Palliative resection of the colon or hemicolectomy significantly improves the quality of life, relieving the patient of such complications of the tumor process as purulent-septic complications, bleeding, tumor disintegration with the formation of a fecal fistula.
A comparative analysis of the immediate and long-term results of treatment of patients with colon cancer who underwent resection or hemicolectomy, regardless of whether the operation was radical or palliative, showed that the frequency and nature of postoperative complications were approximately the same.
Palliative surgical interventions in the form of resection or hemicolectomy are finding more and more supporters and are increasingly the operation of choice for metastatic colon cancer. This was facilitated by a decrease in the incidence of postoperative complications and mortality, and an expansion of indications for resection of organs affected by metastases (liver, lungs). When determining indications for palliative surgical interventions such as colon resection or hemicolectomy, both the general condition of the patient and the degree of tumor dissemination are taken into account.
One of the important factors influencing the prognosis of the disease in patients undergoing liver resection for metastases is the time interval between treatment for the primary tumor and detection of liver metastases. It has been established that the longer the duration of the relapse-free course of the tumor process, the more favorable the prognosis for surgical treatment of liver metastases.
When determining the extent of surgical intervention for metastatic colorectal cancer, studying the functional state of the liver plays an important role. Liver failure itself is one of the main causes of postoperative mortality in major liver resections. The liver is an organ with great compensatory capabilities. 10-15% of its healthy parenchyma is enough for the full functioning of the organ.
An important issue for determining surgical tactics is the number of metastatic nodes in the liver. Multiple nodes significantly worsen the prognosis and are one of the main reasons for refusing active surgical tactics. However, the presence of multiple nodes localized in one anatomical half of the liver is not a contraindication to surgical treatment, although, of course, the prognosis in such patients is much worse than with a single and single (2-3 nodes) metastases.
Combination treatment of colon cancer
The reasons for failure of surgical treatment of patients with colon adenocarcinoma are local relapses and distant metastases. Unlike rectal cancer, with this disease local relapses are relatively rare, and liver metastases predominate. In patients with stage III colon cancer, local relapses occur in 7% of cases, and distant metastases in 20%. The occurrence of these unfavorable secondary tumor formations is due to the dissemination of tumor cells during surgery. Preoperative radiation therapy, which has recently begun to be introduced into the practical activities of oncoproctology clinics, can increase the ablasticity of surgical interventions.
Depending on the sequence of application of ionizing radiation and surgical intervention, pre-, post- and intraoperative radiation therapy is distinguished.
Preoperative radiotherapy
Depending on the purposes for which preoperative radiation therapy is prescribed, two main forms can be distinguished:
- irradiation of operable forms of colon cancer;
- irradiation of inoperable (locally advanced) or doubtfully operable forms of tumors.
The death of tumor cells as a result of radiation exposure leads to a decrease in tumor size and separation from surrounding normal tissues due to the proliferation of connective tissue elements (in cases of prolonged preoperative irradiation and delayed operations). The realization of the positive effect of preoperative radiation therapy is determined by the magnitude of the radiation dose.
Clinical studies have shown that a dose of 40-45 Gy leads to the death of 90-95% of subclinical growth lesions. A focal dose of no more than 40 Gray, administered at 2 Gray daily for 4 weeks, does not cause difficulties in performing subsequent surgery and does not have a noticeable effect on the healing of the postoperative wound.
Postoperative radiotherapy
Certain advantages of postoperative radiotherapy are:
- planning the volume and technique of irradiation is carried out on the basis of data obtained during surgery and after a thorough morphological study of the removed tissues;
- there are no factors that have a negative impact on the healing of postoperative wounds;
- surgical intervention is performed as quickly as possible from the moment of clarifying diagnosis of the disease.
To achieve a therapeutic effect during postoperative radiation therapy, high doses are required - at least 50-60 Gray.
The presence of inflammatory phenomena in the surgical area, disruption of blood and lymph supply leads to a delay in the supply of oxygen to tumor cells and their complexes, which makes them radioresistant. At the same time, normal tissues in a state of regeneration become more radiosensitive, namely, they must be included in a larger volume in the target for postoperative irradiation, because it is necessary to influence the tumor bed, the entire postoperative scar and areas of regional metastasis.
Colon cancer
The following types of colon oncology are distinguished:
- Adenocarcinoma - originates in glandular cells that produce mucus to lubricate the inner surface of the intestine;
- Carcinoid tumor - arises from hormone-producing cells of the intestine;
- Lymphoma is a cancer directly related to disorders of the immune system;
- Squamous cell carcinoma develops from mucous membranes and epithelial tissue. Quickly grows into adjacent tissues and organs;
- Angiosarcoma - formed from fragments of the wall of blood vessels (hemangiosarcoma) or lymphatic vessels (lymphangiosarcoma).
Symptoms of colon tumors
Benign tumors can be asymptomatic; doctors often discover them during a general diagnostic examination.
Also signs of benign tumors of the large intestine are diarrhea, pain in the abdomen, and blood in the stool. Villous tumors can provoke changes in the protein composition of the blood and lead to anemia. Large benign formations also cause intestinal obstruction, the invasion of one section of the intestine into another.
A tumor of the distal sigmoid colon manifests itself as scarlet blood in the stool without mucous admixture. Pathology in the descending colon is indicated by dark blood with a mucous extract. With malignant formations in the proximal intestine, bleeding, often hidden, is expressed only in anemia. Also, symptoms of colon cancer can include tenesmus - a false urge to have a bowel movement, which is caused by spasms of the anal sphincters. In the later stages of tumor formation, constipation and intestinal obstruction appear. There may be a feeling of incomplete bowel movement. Patients with colon cancer also experience symptoms such as decreased appetite, weakness, and sudden weight loss. As the disease progresses, the liver enlarges and abdominal hydrops (fluid accumulation in the abdominal cavity) appears.
Stages of cancer development
Colon cancer occurs in four stages.
The development of a cancerous tumor usually occurs in several stages. If we talk specifically about colon tumors, there will be four such stages:
- First (initial) stage. At this stage, the tumor is very small in size and is localized strictly within the boundaries of the intestinal mucosa and submucosa.
- Second stage. The tumor increases in size. At this stage, malignant neoplasms can still be successfully treated with chemotherapy due to the absence of metastases.
- Third stage. The tumor spreads across the entire width of the intestinal wall and begins to metastasize to the nearest lymph nodes.
- Fourth stage. The malignant neoplasm is acquiring alarming proportions. Its metastases spread far beyond the intestines. Not only nearby organs and lymph nodes are affected, but also those located at a sufficient distance from the source of the disease. Due to the large number of metastases, treatment of cancer at this stage with chemotherapy is usually considered ineffective.
Interestingly, according to the described scenario, any malignant tumors develop, regardless of their shape (endophytic, exophytic or saucer-shaped) and cellular structure. However, this does not mean that the mentioned signs do not play any role in diagnosing cancer.
After all, it is the classification of tumors by cellular structure that allows doctors to choose the most competent strategy for getting rid of a particular malignant neoplasm. What is cancer like? Based on their cellular structure, doctors divide all malignant tumors into the following groups:
- adenocarcinomas;
- mucocellular cancer;
- undifferentiated neoplasms;
- unclassifiable cases.
If we talk specifically about tumors affecting the large intestine, then in approximately 80% of cases the patient has to deal with adenocarcinoma of the mucous or non-mucosal type.
Diagnosis of precancerous diseases
A number of methods are used to detect precancerous diseases and even to diagnose colon cancer:
- Sigmoidoscopy - examination of the rectum and final sections of the colon. Using this method, polyps and tumors can be detected in the rectum and distal sigmoid colon;
- Irrigoscopy (link to x-ray page);
- Videocolonoscopy;
- Radiography;
- Ultrasound examination of the abdominal organs;
- CT (computed tomography);
- Complete blood test to determine the level of red blood cells and white blood cells;
- Endoscopy.
How is cancer diagnosed?
A general blood test will help detect a tumor in time.
Due to the non-specificity of the symptoms of intestinal cancer, it is very difficult to detect it in the early stages. That is why it is so important to promptly contact specialists at the first signs of dysfunction of the gastrointestinal tract.
This is especially true for people for whom the risk of tumor formation is considered increased (we are talking, in particular, about people over 50 years of age).
One way or another, if during a conversation with the patient the doctor has reason to suspect the visitor has cancer, he will refer the patient for additional diagnostic examinations. To detect a malignant tumor in a timely manner, doctors carry out a number of research procedures. Among them:
- visual examination of the patient;
- taking anamnesis;
- examination of the intestine by palpation;
- sigmoidoscopy;
- general blood analysis;
- stool occult blood test;
- colonoscopy.
All of the above studies are carried out strictly in the order described above. Usually, the procedures mentioned are enough to confirm or refute the diagnosis of colon cancer. In other cases, the doctor may refer the patient for other, more detailed examinations:
- Ultrasound of the abdomen;
- Ultrasound of the pelvic organs;
- endorectal ultrasound;
- intestinal biopsy.
It is worth noting that a tumor formed in the lower intestine can usually be detected by palpation. However, with neoplasms that have spread to the upper part of the mentioned organ, everything is not so simple.
Often, to detect them, it is necessary to conduct more than a dozen different tests and examinations. That is why, if you discover one or more alarming symptoms that may indicate intestinal cancer, you should not neglect any of the available diagnostic procedures.
Treatment of colon tumors
In the treatment of colon tumors, including cancer, surgery provides the most reliable results. Let's list their varieties.
- Resection of the large intestine - truncation, partial removal of a section of intestine;
- Hemicolectomy is the resection of one half of the colon followed by the application of an interintestinal anastomosis (artificial connection). This type of operation is prescribed mainly for significant damage to parts of the colon (Crohn's disease, colon cancer, large benign formations, etc.);
- Colproctectomy - complete removal of the colon + creation of an intestinal fistula on the anterior abdominal wall (a hole in the intestinal wall connecting it to the surface of the body);
- A total colectomy is the complete removal of the large intestine while preserving the rectum. There are clear indications for this operation: multiple common polyposis, nonspecific ulcerative colitis, diverticulosis (the muscular layer of the intestinal wall weakens and so-called “pockets” of diverticula form in it, where feces can accumulate), chronic protracted coprostasis (stagnation of feces);
- Abdominoanal resection is the elimination of part of the rectum followed by a colostomy (the surgeon brings the end of the sigmoid or colon to the abdominal wall). The anal canal is sutured;
- Ileorectal anastomosis is the restoration of the continuity of the intestinal tract after radical colectomy (absolute removal of the colon) by forming an intestinal anastomosis between the ileum and rectum;
- Transanal excision is appropriate when the tumor is about 10 cm from the edge of the anus and if the tumor is mobile and can be “cut off” by moving it into the anal canal.
During the postoperative period, patients recovering their health stay in the hospital for about a day or two.
Causes of intestinal tumor development, risk factors
Scientists have still not been able to reliably establish the cause of colon tumors.
However, over the course of many years of research and systematization, doctors were able to identify risk factors that contribute to the development of the disease:
- polyposis, including hereditary ones. The presence of benign neoplasms in the large intestine often leads to the development of a tumor. Every seven years, the risk of cancer increases by 10%;
- hereditary predisposition. In half of the cases, the disease diagnosed in parents is found in children. Moreover, adenomatous polyposis and non-polyposis cancer caused by gene mutations are also taken into account;
- long-term course of ulcerative colitis, Crohn's disease;
- chronic constipation;
- long-term use of anti-inflammatory drugs.
According to statistics, colon tumors occur in approximately equal proportions in men and women. With age, the risk of developing the disease increases. The likelihood of cancer is also affected by lifestyle, in particular, the nature of nutrition - an excessive amount of fatty meat and baked goods in the diet, a lack of plant foods, cereals. The risk group includes people with obesity and impaired metabolism of fats and carbohydrates.
Treatment of all colon tumors should begin as early as possible, because even benign tumors can develop into malignant tumors over time. The earlier therapy is started, the more effective it will be.
Prices for services Get a consultation
| Service | Price |
| Sigmoidoscopy with a rigid rectoscope | 880 rub. |
| Total video colonoscopy | 4,500 rub. |
| Colon biopsy using endoscopy Without the cost of the main study | 440 rub. |
| Resection of the transverse colonHistological examination is paid additionally | RUB 20,900 |
| Right-sided, left-sided hemicolectomyHistological examination is paid additionally | RUB 25,300 |
| Hartmann's operation (resection of the sigmoid colon with colostomy) Histological examination is paid additionally | RUB 23,100 |
| Formation of the anus praeternaturalis | 19,800 rub. |
| Anterior rectal resectionHistological examination is paid additionally | RUB 24,200 |
| Abdominal-anal resection of the rectum with reductionHistological examination is paid additionally | RUB 25,300 |
| Abdominoperineal extirpation of the rectumHistological examination is paid additionally | 33,000 rub. |
| Application of bypass interintestinal anastomosis | 16,500 rub. |
| Reconstructive surgery on the intestines, category 1 of complexity | 27,500 rub. |
| Reconstructive surgery on the intestines, category 2 of complexity | RUB 38,500 |
Oncological diseases of the large intestine often have a similar course, which complicates the diagnosis and treatment of this pathology. At the same time, there are many differences between them:
- by quantity and concentration, multiple and single formations are distinguished;
- location: tumors of the cecum, colon, sigmoid and rectum;
- cellular structure: adenomas, adenopapillomas, squamous cell carcinoma, etc.;
- growth pattern:
- exophytic - protrude into the intestinal lumen;
- endophytic - grows into the intestine;
- saucer-shaped - combines the characteristics of exophytic and endophytic growth.
Types of tumors
The most important classification is the division into malignant and benign.
Neoplasms of the first type include adenocarcinomas, squamous cell and basal cell carcinomas, etc. Malignant tumors grow rapidly, and they destroy healthy tissue, blood vessels and nerves. Cancer cells are very different from healthy cells in the intestinal tube and do not perform normal functions.
Benign neoplasms: polyps, diffuse polyposis, vascular pathologies. They grow slowly, do not invade normal tissue, and do not metastasize. Tumor cells are not very different from healthy cells.
It should be remembered that the concept of “benign” is relative. The disease must be considered as a precancerous condition. If the tumor reaches a large size, it compresses healthy tissue and closes the intestinal lumen, which leads to intestinal obstruction.
Treatment of both benign and malignant intestinal tumors should be carried out in a timely manner.
Symptoms of malignant and benign neoplasms are varied. They depend on the number and location, speed and nature of growth, and the presence of metastases.
You should be alert to the following symptoms:
- prolonged discomfort and pain in the abdominal area;
- diarrhea, alternating diarrhea and constipation;
- blood in the stool;
- general weakness and fatigue;
- anemia;
- weight loss.
Question answer
How much does the food we eat affect the formation of tumors?
Yes, the risk of developing tumors increases if you have food in your daily diet that is low in fiber, but rich in animal proteins and fats. In this situation, a person may experience frequent constipation, and an imbalance of intestinal flora is likely. The content of bile acids and carcinogenic phenols increases in the intestines. And this harms the mucous membrane. Smoked foods and preservatives also cause harm. They also contain predominant carcinogens. Fact. A person is able to eat food even when placed upside down, since special peristalsis muscles “turn on” in time. This explains why astronauts eat in a weightless state.
Can anal sphincter insufficiency predict the appearance of a colon tumor?
Mostly no. Colon incontinence is associated primarily with obstetric trauma and muscle dysfunction as a result of nervous disorders. This is also a reaction to various inflammatory diseases, to prolapse of hemorrhoids or the rectum itself.
Is it possible to perform sphincter-sparing surgery for familial adenomatosis (a hereditary disease that is accompanied by the formation of many polyps on the mucous membrane) of the colon?
If the polyps have not progressed to the stage of cancer, then the probability remains approximately 85%. If the polyps have become malignant, then this kind of sparing surgery is permissible only in 30% of cases of the total number of cases. But removal of polyps in the affected parts of the intestine is mandatory, since cancer appears from them one way or another.