Fundic gland polyps
The most common type of polyps detected during endoscopy. According to large modern studies, gastric fundic polyps are diagnosed in approximately 6% of patients undergoing endoscopy. This, in turn, accounts for about 74% of all gastric polyps confirmed by histological evaluation. Endoscopically, gastric fundic polyps are usually multiple, small (less than 10 mm), with a smooth surface, shiny and macroscopically “sessile” (0-Is according to the Paris classification 2002-2005). With chromoscopy and narrow-spectrum endoscopy (NBI), the surface is represented by a pattern of the type “honeycomb” with dense vascular architecture. Initially, fundic polyps were associated with hamartomas (formations representing a tissue abnormality of development), however, a large number of studies have confirmed that the mechanisms that suppress the secretion of hydrochloric acid by proton pump inhibitors (PPIs) may also be involved in the pathogenesis of the development of fundic polyps of the stomach.
Histologically, fundic polyps are represented by dilated (enlarged) acid-producing glands, covered with flat parietal and mucous cells without signs of dysplasia. Identification of characteristic gastric polyps in patients taking PPIs is more likely to be diagnosed as fundic gland polyps. During the initial examination, one or more polyps present after taking a biopsy are subjected to morphological evaluation to confirm the diagnosis. Large polyps (more than 10 mm), eroded, located atypically, for example, in the antrum of the stomach, should be subjected to more aggressive management tactics - endoscopic polypectomy.
Hyperplastic polyps
This is an inflammatory proliferation of gastric foveal cells (mucin-producing epithelial cells). Hyperplastic gastric polyps are associated with mucosal atrophy caused by H. pylori infection or autoimmune gastritis. However, recently there are more and more cases of detection of such polyps against the background of normal or reactive mucosa, not associated with concomitant infection. Hyperplastic polyps occur equally in men and women in the 6th to 7th decades of life. The most common location is the antrum of the stomach. Endoscopically, they are usually smooth, dome-shaped (0-Is, 0-Isp type), ranging in size from 5 to 15 mm in diameter, although they can be much larger. Large polyps become lobulated, located on a stalk (0-Ip type), the surface of the epithelium of the polyp is often eroded, which can cause chronic blood loss and iron deficiency anemia. Patients are rarely admitted with signs of high obstruction due to obstruction or prolapse of the polyp through the pylorus. Hyperplastic polyps arise as a hyperproliferative response to damage to the mucosa (erosions, ulcers). Long-term chemical exposure to hydrochloric acid and the presence of H. pylori infection may be the initial step in their development.
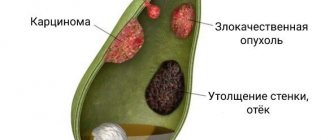
Histological characteristics include elongated, distorted, branched, dilated foveal glands with a richly vascularized stroma accompanied by chronic inflammation. It has been shown that 1 - 20% of polyps may harbor foci of dysplastic changes. In general, the prevalence of carcinoma is less than 2% and is usually found in polyps larger than 20 mm. Due to the potential risk of developing gastric cancer, all hyperplastic polyps larger than 10 mm in diameter should be completely removed. Resection of polypoid formations should always be supplemented by taking samples of intact mucosa, which contain information about the extent and severity of inflammatory and atrophic changes in the surrounding mucosa (according to the OLGA morphological classification). As a result, the stratification of the risk of developing stomach cancer is determined.
Current thinking is that H. pylori eradication should be performed followed by evaluation between 3 and 6 months after therapy to confirm successful treatment. In many cases, the small hyperplastic polyps left behind may regress or disappear altogether. Patients with OLGA stages III and IV (moderate diffuse or severe mucosal atrophy, along with widespread intestinal metaplasia) should undergo endoscopic follow-up at least once a year, since the risks of developing gastric cancer in this case increase more than 6 times .
Gastric adenoma
Most common gastric neoplastic polyp
- This is an epithelial dysplastic growth of tissue, often called an adenoma, according to the modern WHO nomenclature - intraepithelial neoplasia. In the Western, industrialized world, H. pylori-related gastric adenomas are becoming rare, accounting for less than 1%, although the incidence of gastric cancer and adenomas in East Asian regions remains high, accounting for about a quarter of all polyps. Like hyperplastic polyps, gastric adenomas occur with equal frequency in men and women, in the 6-7 decades of life. Endoscopically, they are presented as a solitary single lobular formation with a velvety surface. Although they can be found in any part of the stomach, they are most often located in the antrum of the stomach.
Gastric adenomas are composed of dysplastic epithelial cells that often appear in association with mucosal atrophy and intestinal metaplasia naturally associated with H. pylori infection. Adenomas can be considered as part of a sequential chain from dysplasia to gastric cancer. There is a directly proportional relationship - the larger the adenomatous polyp, the higher the likelihood of having an adenocarcinoma focus in it. Considering the fact that an adenoma that occurs against the background of chronic atrophic gastritis is a precursor of adenocarcinoma, complete removal (resection) of all adenomatous polyps should be recommended with an assessment of the severity of inflammatory and atrophic changes in the gastric mucosa. It is important that an adenoma is a neoplastic formation, and therefore all patients with identified adenomas must be placed under endoscopic observation, despite the stage of mucosal atrophy. Eradication therapy for H. pylori followed by confirmation of treatment effectiveness should also be assessed by histological examination.
Neuroendocrine tumors (NET)
Carcinoids are neuroendocrine tumors arising from enterochromaffin-like (EC) cells. NETs make up less than 2% of polypoid formations of the stomach and are divided into three main types.
- Type I NETs
account for 70-80% of all neuroendocrine tumors. They are associated with hypergastrinemia due to autoimmune atrophic gastritis; moreover, they occur in elderly patients, more often women with atrophic gastritis against the background of pernicious anemia. These formations are discovered by chance, they are small (less than 10 mm), multiple, morphologically consisting of endocrine cells with a low proliferative index (not prone to malignancy). - Type II NETs
are associated with hypergastrinemia due to a gastrin-secreting tumor. It is one of the components of such syndromes as MEN-1 and Zollinger-Ellison. This type of tumor is quite rare, accounting for only 5–8% of all NETs. In this case, the tumor is less than 1 cm, without characteristic infiltrative changes, the surrounding mucous membrane is either normal or moderately inflamed, but without atrophic phenomena. Gastric NETs of types I and II can be removed endoscopically, followed by suppression of gastrin secretion with medication. - Type III NETs
occur sporadically. They make up about 20% of all NETs and are usually detected when clinical symptoms appear (epigastric pain) or when mucosal erosion occurs (manifested by bleeding), or when metastases are detected (presence of carcinoid syndrome - skin hyperemia, diarrhea, bronchospasm, pathology of the heart valve system). This type of tumor tends to reach sizes greater than 1.5 cm, with polymorphic changes in the mucosa (erosion, areas of necrosis, infiltration of the mucosa). The proliferative index (KI-67, mitotic activity index) is more than 20%, which indicates a malignant course of the disease requiring surgical treatment.
Treatment of stomach polyps
As stated earlier, all adenomatous and large polyps larger than 10 mm should be removed. How is endoscopic polypectomy or mucosal resection performed?
After clearly defining the boundaries of the formation, an injection of saline solution colored with indigo carmine blue dye is performed under its base into the submucosal layer in order to prevent perforation and clearly visualize the vascular structures. Then the endoscopic loop is positioned on the unchanged mucosa around the formation and is gradually tightened. Next, electrocoagulation is performed using an electrosurgical knife/block. A post-resection defect with a white scab without “plus tissue” indicates the radicality and reliability of the surgical intervention, thereby eliminating possible complications. The stages of the operation are presented in the pictures (in our Clinic we use a knife - ERBE VIO 300D).
Large exophytic (protruding) polyps on a wide base or flat formations that cannot be removed with endoloops are subjected to a technically more complex version of endoscopic removal - dissection in the submucosal layer. This type of operation is aimed at radical removal of the formation as a single block: after creating a “hydrostatic cushion”, a circular incision is made around the formation with special instruments, after which the connective tissue plexuses of the submucosal layer are dissected with complete elimination of the pathological focus.
Postoperative follow-up
The first day after polypectomy, a gentle regimen of activity and nutrition is recommended. As mentioned earlier, a post-resection defect of the mucous membrane remains at the site of the polyp, and therefore an anti-ulcer diet is prescribed - table No. 1 according to Pevzner. Its essence is to limit foods that stimulate secretion in the stomach, long-lasting and difficult to digest foods (spicy, fatty, fried foods). This diet and restriction of physical activity are followed for a month. It is also necessary to remember not to take anticoagulants for 3 days both before and after surgery, in order to prevent early and delayed bleeding.
According to modern concepts, the most rational is to monitor patients after polypectomy after 1 year. At the same time, the condition of the mucous membrane is assessed for the appearance of new formations or relapse at the site of a previously performed operation. If, after resection of the formations, the histological response confirms the presence of high-grade dysplasia or early cancer, then control gastroscopy should be carried out in the interval: 1.5 months - 3 months - 6 months. – 1 year and every year thereafter.
Symptoms of the disease
Sometimes polyposis occurs unnoticed by a person and is discovered by chance during an endoscopic examination of the gastrointestinal tract. However, large polyps in the stomach most often cause symptoms. The main ones include:
- Soreness and cramping in the upper abdomen, especially in the left and center;
- Repeated vomiting after eating or taking medications;
- Nausea;
- Increased salivation;
- Long-term severe loss of appetite, weight loss;
- Vomiting mixed with blood and black feces are the most dangerous signs indicating bleeding from injured polyps.
Causes of the disease
The causes of the disease include all damaging factors affecting the gastric mucosa:
- Helicobacter pylori infection (bacterium H. pylori);
- Chronic gastritis, especially with high acidity;
- Peptic ulcer;
- Excessively long-term use of proton pump inhibitor drugs (Omeprazole, Pantoprazole);
- Hereditary predisposition;
- Abuse of alcohol, spicy foods;
- Smoking.
Some of these factors provoke the development of polyps of a specific type: Helicobacter pylori infection leads to hyperplastic ones, excessively long-term use of Omeprazole leads to polyps of the fundic glands.
The severity of the disease depends on the number of tumors, their size and location in the stomach. Multiple or large ones can interfere with the normal passage of food; their constant trauma can lead to the appearance of dysplasia - this is the first step in the degeneration of body tissue into malignant. The greatest danger in terms of oncology is adenomatous and some types of hyperplastic.
Sign up for a consultation
Prevention of stomach polyps
The goal of prevention is to identify gastric formations in the early stages of development. It is recommended to perform an endoscopic examination for persons over 45 years of age as a screening test, even in the absence of clinical symptoms, since the disease manifests itself only at a late stage, when surgical treatment is already required. Following the principles of oncological vigilance, patients with a burdened hereditary history, that is, in the presence of oncological diseases of the gastrointestinal tract in close relatives, require an immediate preventive examination of the stomach and colon.
How to get a service at the Clinic
Our Clinic conducts all types of endoscopic examinations using high-quality equipment, both under local anesthesia and general anesthesia. All identified pathological formations are subject to histological verification. Material is also taken to check for the presence of H. pylori infection and to determine the stage and severity of inflammatory and atrophic changes in the gastric mucosa (OLGA class), which indicates, as mentioned earlier, the risk of developing an oncological process.
As for surgical endoscopic treatment, the clinic can perform it on an outpatient and inpatient basis. The decision is made by the attending physician, based on the size of the pathological lesions, their number, histology results and concomitant pathology.
Diagnostics
Diagnosis of stomach tumors consists of three main stages: history taking, examination, radiographic and endoscopic examination. A blood test is also prescribed, which can detect a decrease in hemoglobin levels, that is, anemia, characteristic of tumors that cause bleeding. The benign quality of a neoplasm is determined by the following characteristics: size, presence of peristalsis (during instrumental examination), shape. Fuzzy contours, rapid growth and lack of peristalsis indicate that the polyp is malignant.
To clarify the diagnosis, endoscopy is used - esophagogastroduodenoscopy, which allows you to visually assess the condition of the mucosa and see in real time the shape and size of tumors localized on the mucosa. This method allows you to assess the risk of malignancy - it is visually impossible to distinguish an early-stage malignant tumor from a benign one; a biopsy is required. If oncology is suspected, during FGDS, a sample is taken for histological examination in the laboratory - a biopsy allows you to accurately determine the nature of the neoplasm.
Since non-epithelial tumors come in a wide variety, it is often possible to make a final diagnosis only after surgery.
The study of tumors located outside the mucosa is possible using the same means: contours are visible on radiography, and endoscopic examination in combination with ultrasound (endo-ultrasound) allows us to determine areas of compression that appear when tumors grow inside the walls of the stomach or towards internal organs.
What is a polyp?
The term “polyp” is translated from ancient Greek as “many-legged.” In medicine, it is used to identify tumors in various organs. If we talk about the gastrointestinal tract, then we are talking about a benign tumor that protrudes into the lumen of a hollow organ and is connected to it either by a stalk or a wide base. Polyps are found in both the upper gastrointestinal tract (stomach) and the colon. Their size can vary from a few millimeters to 5–8 centimeters.
When performing gastroscopy in people over 50 years of age, polyps are found in up to 6% of cases, and during colonoscopy - up to 40% of patients.
Diet
Diet for polyps in the stomach
- Efficacy: therapeutic effect after 30-60 days
- Timeframe: 1 month
- Cost of food: 1350-1520 rubles per week
Diet table No. 1
- Efficacy: therapeutic effect after 3 weeks
- Terms: 2 months or more
- Cost of products: 1500 - 1600 rubles. in Week
Dietary table No. 1a
- Efficacy: therapeutic effect after a week
- Terms: 3-10 days
- Cost of food: 900-1100 rubles per week
An addition to drug treatment is following the Table No. 1 for normal and increased secretion of gastric juice. It involves moderate chemical and mechanical sparing of the entire gastrointestinal tract. In terms of the content of basic nutrients, it is physiologically complete. It is important to follow a diet - frequent meals in small portions. The products are consumed boiled and stewed. These can be steamed and boiled dishes from pork, chicken, beef, turkey, and rabbit.
Meat is used to prepare cutlets, quenelles, soufflés, meatballs, meat puree and zrazy. Garnish includes boiled pureed vegetables, boiled porridge (oatmeal, buckwheat, semolina or rice), thin noodles. Puree vegetable soups with the addition of meat and porridge are seasoned with butter. Fruits are also consumed after heat treatment. Dried wheat bread is allowed.
Excluded from the diet:
- Strong meat and fish broths, cabbage soup, borscht, okroshka.
- Rye bread, baked goods.
- Spicy and salty cheeses.
- Stringy varieties of meat, fatty and difficult to digest meat of duck and goose.
- Canned food, smoked meats.
- Millet, barley, corn and pearl barley, legumes.
- White cabbage, turnips, sorrel, rutabaga, radishes, onions, garlic, cucumbers, mushrooms.
- Pickled and pickled vegetables.
- Sauces and marinades.
- Chocolate, ice cream.
- Strong coffee and tea.
- Alcohol.
Diet after polyp removal
After endoscopic intervention, in the first 10-12 hours the patient is advised to refuse to eat. In the future, the diet gradually expands to include boiled semi-liquid porridges, pureed soups, mashed potatoes, meat and fish soufflés. Patients are prescribed Diet No. 1A , which is based on maximum mechanical and chemical sparing of the mucous membrane, which helps reduce inflammation and heal the postoperative defect. Meals include:
- Slimy soups made from oatmeal, buckwheat and rice with the addition of beaten eggs, butter or cream.
- Boiled meat and fish are passed through a meat grinder and then added to soups or porridges.
- Steam omelette.
- Semi-liquid porridge from buckwheat and oatmeal, cereal flour.
- Milk, cream, soufflé made from non-acidic pureed cottage cheese, milk porridge.
Classification
These formations that grow in the stomach can be divided into two large groups.
Hyperplastic polyps are the most common. They consist of epithelial tissue, which for some reason has grown and increased in volume. They cannot be considered a true tumor. In the stomach, such formations usually do not degenerate into malignant ones.
Adenomatous polyps arise from glandular cells. They are true tumors and have a high risk of developing into cancer. Especially if such a formation is larger than 20 mm.
Gastric polyps of this type can be divided into tubular, papillary and papillotubular. Their type can be determined only after a biopsy and histological examination of the tissue.
Also, these formations can be single or multiple, and are classified by size.
Complications
Polyps in the gastrointestinal tract left untreated can cause serious complications. It could be:
- Degeneration into a malignant tumor.
- Decreased gastric permeability.
- Ulceration of the surface of the growth.
- Exit of a pedunculated polyp into the intestine.
- Intestinal obstruction.
- Development of mucosal dysplasia, which is a precancerous condition.
- Bleeding.
All this can be life-threatening and requires immediate treatment to prevent death.
Why do they appear?
Most often, the growth is diagnosed at the age of 40–50 years.
The pathology is rare in young people. If we talk about gender, patients are usually men - the disease is detected in them 2 times more often than in women. The majority of all diagnosed formations are found in the pyloric (outlet) section, less often in the body of the stomach. Single polyps occur in 47% of cases, multiple polyps in 52%. Polyposis occurs in 2% of all patients.
The exact reason for the formation of polyps in the stomach is not yet known. There are many factors that can trigger the appearance of a benign tumor in this organ.
- Age over 40 years.
- Gastritis of any type.
- The bacterium Helicobacter pylori, which lives in the stomach.
- Genetic predisposition.
However, a stomach polyp does not always appear precisely for these reasons. Sometimes it is impossible to establish a connection with any provoking factor and then it is customary to talk about an idiopathic disease.