Adenocarcinoma is a malignant formation that arises from epithelial glandular cells. As for such a subtype of pathology as well-differentiated adenocarcinoma, it is considered the mildest form, almost easily treatable. Pathology is formed from the epithelial cellular components of the upper skin layer, the epithelium itself, which covers the internal organic surfaces (stomach, uterus, intestines, and some other organs). There are almost no visible differences between pathogenic and normal cells. The most obvious change concerns only the cell nucleus, which lengthens.
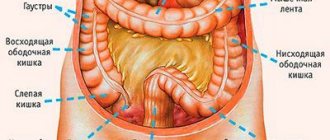
Based on the degree of cellular differentiation, several types of such cancer lesions can be distinguished. Also, when classifying the disease, the location of the cancer focus can be taken into account (for example, adenocarcinoma of the colon, uterus, stomach, etc.).
What should you pay attention to?
In oncological practice, the criterion of five-year survival is taken into account. To understand whether a person will live to this point, you need to consider:
• tumor dimensions (the larger, the lower the chance of survival); • depth of tumor growth (here, accordingly, the deeper, the worse the prognosis); • the presence of metastases – when these components are detected, the prognosis is poor, because this indicates the late stages of the pathological process.
It should be noted that well-differentiated adenocarcinoma itself is considered a factor affecting survival. This type of cancer lesion is the easiest to cure (in comparison with defects of moderate or low differentiation).
The main methods of therapy to successfully combat adenocarcinoma of the large intestine
Fortrans is a means for cleaning the gastrointestinal tract.
Surgical removal of the tumor. This method is the most effective, since during surgery the tumor is removed, which is essentially the source of the disease.
Tissues affected by metastases are also removed. It is very important to adhere to all preparation rules before the operation, namely:
- follow a slag-free diet, the nuances of which are explained to the patient by the doctor;
- carry out (on your own or with the help of medical personnel) manipulations related to cleansing the intestines of feces. This is usually done 3-5 days before surgery through enemas and laxatives;
- do (as prescribed by a doctor) gastrointestinal tract lavage using modern, improved means. The optimal ones for this are “Fortrans” and “Lavage”.
Chemotherapy therapy is also effective. In particular, drugs such as Raltitrexide, Ftorafur and Capecitabine, Leucovorin, Irinotecan and 5-fluorouracil are used. When these drugs are combined, treatment becomes more effective.
Causes of adenocarcinoma
Doctors still don’t know exactly what causes a malignant lesion. Medicine identifies only risk factors. Such provoking prerequisites often include: heredity, old age, the influence of external factors (poor environment, harmful working conditions), abuse of alcohol and tobacco products, frequent use of strong medications, systematic stress, obesity, defects of a specific organ (for example, stomach ulcers), increased concentration of estrogen, poor nutrition (abuse of fast foods, fatty foods, etc.).
Treatment
Intestinal adenocarcinoma is treated with three methods:
- surgical removal;
- chemotherapy;
- radiation therapy.
Most often you have to mix and match all available methods. To select the method of operation, the following are taken into account:
- localization;
- dimensions;
- nature of cell differentiation;
- classification according to the international system.
During the period of preparation for the operation, special nutrition is used with mixtures without toxins, a system of laxatives and cleansing enemas, and Fortrans to remove harmful substances.
Fortrans is taken according to the regimen specified in the instructions.
The following is carried out surgically:
- resection (excision) of the affected limited area;
- extirpation (removal) of the intestine, lymph nodes and neighboring organs when metastases grow in them.
The operation usually ends with the formation of an artificial stool outlet on the anterior abdominal wall (colostomy). Radiation therapy is carried out 5 days before surgery and a month after it. The irradiation zone is determined by the location of tumor growth.
For chemotherapy, combinations of drugs are used in repeated courses:
- 5-fluorouracil;
- Ftorafur;
- Adriamycin;
- Mitomycin-C.
The drugs have pronounced negative properties, so the effect is monitored by blood and urine tests.
Features of nursing
In the postoperative period, patients are severely weakened. Due to the use of chemotherapy and radiation, the immune status drops sharply. They are at risk of infection by any pathogen. Therefore it is recommended:
- change your underwear more often;
- Perform daily hygiene procedures (brush your teeth, rinse your mouth, wipe your body);
- prevent the formation of bedsores (change body position, smooth out folds of linen, lubricate the skin with camphor alcohol, massage);
- in the first days feeding is carried out using a tube and intravenous mixtures;
- the use of incontinence diapers should be considered;
- when replacing a colostomy bag, treat the skin around the colostomy with warm water and wipe dry;
- Perhaps the doctor will recommend lubrication with cream.
What nutrition is needed?
Food must support the patient’s strength, have sufficient calories, do not contain irritating elements, and be easy to digest. Strictly contraindicated:
- fatty foods;
- spicy seasonings;
- fried and smoked meat products;
- alcohol;
- legumes;
- fresh vegetables in salads.
The patient should be fed 6 times a day, in small portions. Useful:
- steamed cutlets, meatballs from lean meats, poultry;
- mild seafood;
- low fat fermented milk products;
- liquid porridge with a teaspoon of butter;
- soups made from milk, vegetables;
- boiled fruits and vegetables;
- berry jelly, compotes, teas with herbs.
The patient will have to monitor his diet throughout his life.
Diagnosis
The process of identifying highly differentiated carcinoma includes collecting anamnesis and carrying out standard diagnostic measures: detailed blood and urinary analysis, stool analysis, ultrasound examination of the area of possible localization of the lesion, removal of biomaterial for subsequent laboratory study. If there is a suspicion of intestinal cancer, a digital examination of the rectum is performed. In addition, a colonoscopy is performed to assess the condition of the mucous membrane of the inner border of the large intestine. Another important procedure is irrigoscopy (x-ray of the large intestine).
Types of tumor depending on cell changes
Tumor growth changes the appearance of glandular cells. The least dangerous cells are those that differ little from normal ones. They can be differentiated (distinguished) by the degree of deviation by cytological examination of the biopsy material. The more pronounced the distinctive features, the less degree of differentiation the cancer cells have.
Among neoplasms such as intestinal adenocarcinoma, the following are distinguished:
- A well-differentiated tumor - under high magnification of a microscope, in contrast to normal ones, enlarged cell nuclei are visible, there are no functional changes, so timely treatment is effective. Therapy for elderly patients is especially effective. It is possible to achieve long-term remission. In young patients, the likelihood of relapses in the next 12 months does not disappear.
- Moderately differentiated adenocarcinoma - reaches a large size, the cells grow strongly, causing intestinal obstruction, bleeding, and wall rupture. The clinical course is complicated by peritonitis and the formation of fistula tracts. There is a high risk of transition to a low-differentiated species. However, after surgical removal and subsequent treatment, five-year survival is observed in 70–75% of patients.
- Poorly differentiated - the tumor is characterized by polymorphism (a diverse composition of cells), grows very actively, quickly spreads to other organs, and affects the lymph nodes. Has no clear boundaries. The operation is indicated at an early stage; it is difficult to predict the duration of remission in advance. In late stages, treatment is ineffective.
Depending on the type of glandular cells, intestinal adenocarcinoma is divided into:
- Mucinous tumor (mucous) - consists of epithelium, mucus with mucin, no clear boundaries, metastasizes mainly to neighboring lymph nodes. It is important that this variety is not sensitive to the effects of radiation therapy. Therefore it gives frequent relapses.
- Signet ring cell – characterized by significant malignancy, often detected with multiple metastases. Especially in the liver and lymph nodes. It affects young people more and is localized in the colon mucosa.
- Squamous cell – has a high degree of malignancy, the most common localization is the rectum. Grows into the bladder, vagina, prostate, ureters. The results of treatment are characterized by frequent relapses and low survival (no more than 1/3 of patients live up to five years, the rest die in the first 3 years).
- Tubular - a tumor with unclear outlines consists of tube-like formations in the form of cubes or cylinders. The size can be small, grows gradually and is prone to massive bleeding. Occurs in half of patients with bowel cancer.
Pulmonary adenocarcinoma
Progresses in lung tissues. Its components differ slightly from the healthy components of the lung. The appearance of such a disease can be stimulated by excessive smoking, systematic exposure of harmful substances to the lungs (this applies to a greater extent to residents of industrial cities), and chronic pulmonary pathologies. Metastasis with such cancer is extremely dangerous: metastases penetrate into nearby and distant organs, as well as into bone tissue. The most characteristic sign of the oncological defect in question is a cough, accompanied by active secretion of mucous sputum. Cancer cells are detected by bioexamination of sputum and using x-rays.
Classification by stages
In order to create a unified approach to assessing the severity of adenocarcinoma, an international classification has been adopted. It divides all intestinal adenocarcinomas into 5 stages. For each the following are defined:
- acceptable size of tumor growth;
- the presence of near and distant metastases.
In stage 0, the tumor is minimal, does not grow anywhere and has no metastases. In stage I-II – sizes are acceptable from 2 to 5 cm or more, but there are no metastases. The third stage is divided into:
- IIIa – germination into neighboring organs and the presence of metastases in the lymph nodes are allowed;
- IIIc – combines large size and the presence of metastasis only in neighboring organs.
Stage IV – is diagnosed for distant metastases, even if the size of the tumor itself is relatively small.
There is a classification of intestinal cancer, which includes such a feature as differentiation of cellular composition. It means that:
- Gx - diagnosed if the cells cannot be differentiated;
- G1 – the degree of differentiation is assessed as high, the cells are similar to normal epithelial ones;
- colon cancer grade G2 - shows an average degree of degeneration;
- G3 – tumor cells are little similar to normal;
- G4 – cell type is low differentiated and is characterized by the highest malignancy.
Outdated, but very bright classification
Elimination of high-grade adenocarcinoma
Therapeutic tactics depend on the stage of oncological pathology and the presence of metastases. The location of the lesion determines the specific features of the therapy performed. Usually they involve radiation treatment, chemotherapy procedures, neutron therapy, and surgery. The rays are designed to slow down the progression of the cancer focus and its decay; in addition, with their help they destroy metastases. As for neutron therapy, this technique is new. The principle of action is similar to radiation therapy, although neutrons are used instead of rays. These elements penetrate into the deep layers of the cancer focus, which have absorbed a specific microcomponent (for example, boron). Once in the deep layers, neutrons begin to destroy cancer cells. At the same time, healthy tissue remains intact.
Diagnosis of the disease
Colon adenocarcinoma is a common cancer. It is quite well studied and easy to diagnose. To identify this pathology, the following screening options are used:
- Examination of stool for fecal DNA. Conducted at the time of application.
- Analysis of feces for occult blood. Rented once a year.
- Virtual colonoscopy of the intestines. Performed once every five years.
- Conventional colonoscopy. It is done once every ten years.
Screening is carried out for patients 45 years of age and older. The frequency and age of completion (80-85 years) depend on the individual characteristics of the patient’s body, his state of health, heredity and a number of other factors.
If during screening the proctologist finds a tumor in the patient, he takes samples of it and sends them for a biopsy (laboratory test). In addition, to clarify the stage of development of adenocarcinomas, the following diagnostic procedures are used:
- Osteoscintigraphy.
- Ultrasound.
- Chest X-ray.
- MRI of the liver.
- Computed tomography of the abdominal cavity.
If, in addition to surgery, the patient is indicated for conservative treatment (with the help of medications), he additionally undergoes a molecular genetic test. Samples are collected and subsequently tested for microsatellite instability, BRAF, RAS and other mutations. Based on the results of the check, the treatment plan is adjusted.
Possible complications
Complications can occur with any type of highly differentiated adenocarcinoma lesion. The appearance of complications is primarily due to the impact of the lesion as it grows. Large tumors can damage organs. Thus, a rupture of the intestinal wall is possible, leading, in turn, to intestinal bleeding. In addition, the specific stage of the oncological process also has a negative impact. Everything is simple here: the further the tumor has gone in its development, the higher the likelihood of damage to nearby organs. The growth of oncological components also plays a detrimental role. For example, increased pathogenic cells in colorectal cancer lead to intestinal obstruction. Also, it is worth remembering concomitant pathologies that can complicate the course of cancer.
A little about the nuances of the operation
Surgery is the treatment method for this disease.
When performing surgery, oncologists try not to touch the tumor, but rather clamp the blood vessels and cut off the affected area of the intestine.
This is done to prevent tumor cells from being carried through the bloodstream throughout the body. In a situation where metastases are located at a considerable distance from the malignant formation, surgery is ineffective.
However, in some cases the intervention is still carried out. This allows you to avoid even greater complications, pain coming from the source, as well as inflammation. If the disease is at an extreme stage, then surgery is necessary in order to normalize the functioning of the intestines and form a so-called colostomy (tube with a hole).
The most common form of colon cancer is adenocarcinoma (75-80% of cases) [2, 4]. Much less common (10-12%) is mucinous adenocarcinoma, characterized by hyperproduction of mucus by tumor cells [5]. Mucinous adenocarcinoma is one of the histological variants of adenocarcinoma of the gastrointestinal tract. The prognosis for mucinous adenocarcinomas is less favorable than for conventional adenocarcinomas that secrete small amounts of mucus. Such tumors are diagnosed mainly after the occurrence of complications: intestinal bleeding, partial or complete intestinal obstruction. The diagnosis can usually only be made through emergency surgery. Often tumors are detected by palpation only when they reach a large size and become inoperable.
In prognostic terms, mucinous cancer of the small intestine is much worse than malignant tumors of the colon. The reason for this is partly the late appeal of patients for help, as a result of which operations are performed on the verge of operability. Extensive resection of the affected colon is part of the conditionally radical treatment of these patients. The rare nature of mucinous adenocarcinoma of the colon has resulted in insufficient research into the benefits of adjuvant chemotherapy [1,6]. Neuroendocrine colon cancers are more often diagnosed in the cecum and ascending colon, large cell morphology of neoplasms - in the colon and rectum, small cell cancers - in the anal canal [8].
We present a clinical case of a patient who was operated on twice over a 9-year period for extensive (T4M0Nx) lesions by a malignant combined tumor—mucinous adenocarcinoma and neuroendocrine colon cancer.
Patient L., 53 years old, was treated for iron deficiency anemia for 3 years and was admitted to the State Research Center in 2001 with complaints of periodic hyperthermia, weight loss, and a tumor formation in the left hypochondrium.
He considers himself sick since the summer of 1998, when shortness of breath, sweating, and a feeling of suffocation at night began. For the first time, profound iron deficiency anemia was identified in 1998, ROE acceleration up to 60 mm/h. An examination of the colon and stomach carried out at that time revealed no pathological changes. The hemoglobin level increased from 56 to 98 g/l. In September 1999, during a colonoscopy in a city clinical hospital, three polyps were identified and removed. Therapy with iron supplements had a positive effect.
Since April 2000, signs of anemia reappeared and a tumor-like formation was discovered in the left hypochondrium. However, the patient was admitted to the Department of Surgical Hematology of the State Research Center only on May 28, 2001 with a referral diagnosis: chronic posthemorrhagic iron deficiency anemia, undifferentiated tumor of the abdominal cavity. Complains of nausea, abdominal pain, and discomfort. The condition is relatively satisfactory. The family history is burdened: the mother died from intestinal cancer, the father from lung cancer. After lengthy preparation, an operation was performed on June 21: laparotomy and revision revealed a dense, tuberous tumor, which was a conglomerate involving loops of the jejunum, transverse colon, root of the mesentery of the small intestine, mesocolon
(Fig. 1, a).
Figure 1. Operation diagram. a - the boundaries of organ resection are indicated by shading.
The tumor was removed en bloc, along with loops of the small and jejunal intestines, the greater omentum, part of the transverse colon and splenic angle of the colon, and the spleen. In addition, due to the presence of stones in the gallbladder, a cholecystectomy was performed. Anastomoses were performed: small-intestinal end to side at the level of the ligament of Treitz and ascendo-descendo end to end (see Fig. 1, b).
Figure 1. Operation diagram. b - reconstruction of the intestine.
Upon urgent histological examination of the biopsy specimen, the nature of the tumor was unclear.
Macroscopically: the tumor was located in the center of the resected area of the colon, the border between the colon wall and the tumor was clear both from the proximal and distal ends (Fig. 2).
Figure 2. Specimen: removed tumor with resected loops of the jejunum (JJ), colon (TlC) and greater omentum (Gal). In an area of about 12 cm, the intestinal wall is sharply thickened (up to 2 cm), cartilaginous density, white in section, translucent. The bottom of the tumor is uneven, lined with blood clots. The greater omentum and a loop of the ileum were fused to the intestinal wall in the area of tumor degeneration, and the spleen was fused to a limited area.
Microscopically: the tumor had a combined structure, poorly differentiated G3 neuroendocrine cancer with infiltration of the submucosal layer (Fig. 3, a),
Figure 3. Micrographs of the tumor.
a — neuroendocrine cancer. Hematoxylin and eosin staining. Uv. 100. tumor emboli in the lymphatic vessels of the submucosal layer, partially - mucinous adenocarcinoma with infiltration of the muscular layer (see Fig. 3, b).
Figure 3. Micrographs of the tumor. b — mucinous adenocarcinoma. Hematoxylin and eosin staining. Uv. 200. Neuroendocrine cancer is represented by large cells with frequent mitoses (2-3 in one field of view, magnification 400), areas of trabecular, organoid structure, and the presence of pseudorosettes.
In satisfactory condition, the patient was discharged under outpatient observation by an oncologist. Three courses of polychemotherapy were carried out at the place of residence: leucovorin + 5-fluorouracil, 6 five-day courses with a break of 20 days.
After 2.5 years, the condition is satisfactory. There is no relapse of the tumor. Normal body weight (60 kg) was restored. On January 26, 2004, the patient underwent plastic surgery for an incisional hernia.
In March 2010, the patient began to complain of pain in the epigastric region and signs of partial intestinal obstruction. Re-hospitalized at the State Scientific Center on 04/01/10. CT scan in the area of the previously applied ascendo-descendo anastomosis shows a tumor measuring 79×55×65 mm, narrowing the intestinal lumen, not differentiated from the left lumbar muscle and the lower pole of the left kidney (Fig. 4).
Figure 4. CT scans. a - frontal section.
Figure 4. CT scans. b - axial section.
On March 13, laparotomy was performed. A tumor conglomerate involving the left kidney and the splenic angle of the colon was detected in the left half of the abdominal cavity. Upon further inspection and in the process of isolation from the adhesions of the colon, two tumor nodes were discovered by palpation: 5 cm from the bauhinium valve in the cecum and 3 cm to the right of the previously imposed colonic anastomosis. The tumor conglomerate was isolated as a single block. The descending colon was cut off at the point of its transition to the sigmoid colon, 12 cm below the tumor. The ileum was transected 15 cm from the ileocecal angle. The tumor along with the left kidney was removed en bloc.
There is no tumor growth into the iliopsoas muscle. A side-to-side anastomosis was performed between the ileum and sigmoid colon.
Macroscopically: in the cecum, 5 cm from the bauginian valve, there is a saucer-shaped tumor with a diameter of 3 cm with an ulcer, 6 cm proximal to the anastomosis, a tumor with a diameter of 4 cm, 9 cm from the resection edge, a tumor measuring 8×7.5×7 cm, growing through all layers of the wall intestines, perinephric fiber, kidney capsule. On the section, most of the tumor is represented by interconnected cavities, up to a maximum of 5 cm in diameter (Fig. 5).
Figure 5. A specimen of the removed colon (opened longitudinally) en bloc with the left kidney. X - sites of tumor recurrence, SA - old anastomosis. The inner surface of the cavities is lined with soft pinkish mucous-like structures. Microscopically: in all foci of the tumor there is a picture of mucous cancer with damage to all layers of the intestinal wall.
The course of the postoperative period was complicated by postoperative pancreatitis, perforation of the small intestine with limited peritonitis. On April 18, a relaparotomy was performed, resection of a loop of the small intestine with the formation of a small-intestinal anastomosis, and sanitation of the abdominal cavity. During therapy, peritonitis regressed and amylase levels returned to normal. However, as a result of swelling of the pancreas and adhesions in the abdominal cavity, paresis of the upper parts of the digestive tract (gastrostasis) was observed for a long time. Up to 1500 ml of stagnant discharge was evacuated from the stomach every day. On May 31, an endoscopic gastrostomy tube was placed and an enteral tube was inserted. With antibiotic therapy and enteral tube feeding, the patient's condition improved. The passage of food has been partially restored naturally. On June 21, the patient was discharged for outpatient observation. With tube feeding, the patient's condition improved; after 3 months, during a follow-up examination, restoration of food passage was noted. The gastrostomy tube has been removed. 24 months after the operation, the patient’s condition is satisfactory, has no complaints, and nutrition is not impaired.
In this observation, there was a combination of two forms of malignant tumors of epithelial and neuroendocrine origin and received the name combined adenoneuroendocrine cancer (MANEC) in the new WHO classification (2010) [9]. It is characterized by a combination of adenogenic and neuroendocrine components, provided that the severity of each component is at least 30%. MANEC of the colon, in particular combined mucinous adenocarcinoma and neuroendocrine carcinoma, is an extremely rare malignant tumor, and therefore the course of the disease and prognosis are poorly studied.
Contrary to the popular belief that mucinous adenocarcinoma of the colon tends to grow faster and metastasize earlier, in our observation the disease was relatively benign. This, on the one hand, prevented early diagnosis, but on the other, did not prevent complete removal of the tumor. Timely radical surgical treatment and subsequent chemotherapy allowed us to hope for a favorable prognosis [3].
According to the literature, the prognosis of the disease is closely related to the prevalence of the process. In the presence of only the primary tumor (neuroendocrine tumor - NET), the 5-year survival rate averages 94% (from 75% for neuroendocrine tumors of the small intestine to 99% for appendix lesions). When regional lymph nodes are involved in the process, the 5-year survival rate is 64%; with a neuroendocrine tumor of the stomach, this figure is much worse - 23%. In the presence of distant metastases, survival rate on average does not exceed 18% [7]. For mucinous cancer, the 5-year survival rate after radical surgical treatment is 61.4%; with combined treatment, this figure reaches 78.4%. The main reasons for failure of both surgical and combined treatment methods are locoregional relapses and metastases to distant organs, most often observed in the first 2 years after radical surgery. After extensive surgical interventions, 3- and 5-year survival rates reach 72.4±6.4 and 65.6±8.2%, respectively [4], which is undoubted evidence of the feasibility of these interventions.
Adenoma
Adenoma is an optional precancer and can appear as a pedunculated polypoid, a short-pedunculated lesion, or a sessile lesion associated with the mucosa. The mass is characterized by homogeneous contrast enhancement and usually does not cause obstruction. Spread beyond the serous layer indicates malignant degeneration.
This example presents a patient with Peutz-Jeghers syndrome, with multiple polyps, mainly located in the jejunum.