Ileitis is a disease that occurs spontaneously and is quite difficult to cure due to the symptomatic features of the disease. However, it is necessary to treat ileitis, otherwise the disease can take horrific forms.
Treatment of ileitis in clinics in Germany, Israel, Austria, the USA, Finland and Switzerland is aimed not only at eliminating the inflammatory process in the ileum of the small intestine, but also at combating such consequences of the disease as ulcers, polyps, purulent fistulas and destruction of the mucosa.
A special feature of the disease is its early manifestation, because in most cases it is young people aged 15-25 years who suffer from the disease. Chronic ileitis is very dangerous, does not allow you to eat normally and causes constant discomfort. Therefore, it is important and necessary to treat ileitis from real professionals and as soon as possible.
Ileitis - what is it?
Mostly, ileitis is diagnosed in people aged 20 to 40 years, more often in men.
It occurs two times less often in rural populations than in residents of large cities. According to scientific data, in 70% of cases, pain in the right iliac region is a symptom of chronic ileitis. In general, the described pathology accounts for 6% of all intestinal inflammation. Classification of ileitis
According to the criterion of damage to the small intestine, the following are distinguished:
- isolated ileitis;
- ileitis, combined with inflammatory processes in the stomach and colon;
- ileitis affecting the entire intestine.
Due to the occurrence of ileitis, it happens:
- parasitic;
- medicinal;
- infectious;
- enzymatic;
- nutritional;
- postoperative;
- toxic.
It can also be primary or secondary (resulting from another gastrointestinal disease).
Taking into account enzymatic activity, doctors distinguish:
- atrophic ileitis;
- non-atrophic ileitis.
According to the characteristics of the course, inflammation can occur with or without complications in three forms:
- light;
- moderate;
- heavy.
Types of ileitis
Depending on the location of inflammation, ileitis is divided into two types:
- First type. These include: - damage to only one part of the small intestine; - damage only to the ileocecal region (the zone of transition of the small intestine to the large intestine); - damage to only one segment of the colon.
- The second type includes: - damage to several parts of the small and large intestine; - simultaneous damage to the intestines and stomach, esophagus, and oral mucosa.
Forms of ileitis
Taking into account the characteristics of the course of ileitis, gastroenterologists classify it into three forms:
- Primary attack (acute symptoms dominate).
- Chronic intestinal ileitis - there are no acute symptoms, the disease lasts more than six months.
- Recurrent ileitis - symptoms often recur, exacerbations alternate with remission for more than six months.
Depending on the characteristics of the clinical picture, it happens:
- acute ileitis (inflammation of the ileum);
- chronic jejunoileitis, accompanied by impaired absorption of nutrients;
- jejunoileitis, complicated by small intestinal obstruction syndrome (the jejunum and ileum become inflamed, the process of passing feces through the intestines is disrupted);
- granulomatous proctitis (multiple small tumor-like formations form on the wall of the rectum),
- granulomatous colitis (small tumor-like granulomas form on the wall of the large intestine).
Crohn's disease (granulomatous esophagitis, gastritis, colitis; ileocolitis, terminal ileitis)
The anatomy and clinical picture of the disease in 14 patients was described in detail by the American physician Crohn in 1932, and the disease was named after him.
The author observed limited nonspecific inflammation of the terminal part of the small intestine, granulomatous ileitis, affecting all layers of the intestine, including the peritoneum. Later it turned out that with this disease, all parts of the digestive canal are involved in the process - the stomach, small intestine and large intestine. Hence the name: granulomatous esophagitis, gastritis, ileocolitis, terminal ileitis. M.X. Levitan (1974) observed 83 cases of Crohn's disease in 1000 patients with diseases of the stomach and intestines. Crohn's disease (granulomatous esophagitis, granulomatous gastritis, granulomatous colitis, ileocolitis, terminal ileitis) is a chronic nonspecific disease of the intestinal tract, characterized by inflammatory and granulomatous-ulcerative lesions of its various parts.
Terminal ileitis is a lesion of the terminal ileum.
Granulomatous colitis is a lesion of parts of the colon.
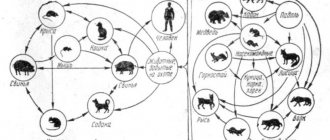
Etiology. The etiology of granulomatous enteritis has not been fully studied. It is believed that the disease is determined by infectious inflammation of intestinal tissues caused by streptococci, enterococci, and saprophytes. Infectious agents become aggressive or become more active due to a decrease in immunological reactivity in the intestine. Recently, there have been reports that granulomatous enterocolitis develops as a result of yersinia infection. In such patients, the causative agents of yersiniosis were isolated from the feces, and serological reactions with yersiniosis antigens were found to be positive. However, the role of yersinia infection in the etiology of Crohn's disease has not been definitely established.
Pathogenesis. The bacteria appear to enter the intestinal tissue through the intestinal mucosa. Bacteria can be introduced into the intestine by hematogenous route. Injuries and circulatory disorders contribute to intestinal inflammation. The occurrence of inflammation and the course of the disease is associated with immunity disorders and is accompanied by hyperergic reactions, damage to the lymphatic tract and lymph nodes. The generalization of the inflammatory reaction is evidenced by the frequent involvement in the process of not only the small intestine, but also the large intestine and esophagus, and in some patients, joint damage. Such reactions are observed more often with yersinia infection.
Pathological anatomy . Nonspecific granulomatous terminal ileitis or ileocolitis is accompanied by a nonspecific inflammatory reaction. It is found in various parts of the gastrointestinal tract.
The morphological picture depends on the localization of the process, the stage of development of the disease and the presence of complications:
- The area of the affected large intestine turns into a thick tube, the mucosa of which can be hyperemic, the tissues are infiltrated, thickened, the lumen is narrowed, and the walls are severely deformed. Ulcerative defects on the mucous membrane in Crohn's disease are deep, reach the subserous layer, are usually localized transversely, and have a slit-like shape. Their surface is covered with mucus. The remaining areas of the mucous membrane are covered by inflammatory granulomas located in the submucosa, as a result of which the inner surface of the small intestine resembles a cobblestone street. Various areas of the colon are also affected, most often the anular region. Ulcers, cracks, and fistulas are revealed here.
- Ulcers and inflammatory infiltrates are also found in the small intestine. The inflamed area turns into a tube that has lost the shape of a healthy intestine. Microscopic histological examination of such tissue reveals signs of nonspecific inflammation: inflammatory cellular infiltration, distributed to all layers of the intestinal wall. Often these inflammatory infiltrates are covered by normal mucous membrane. The infiltrates contain a large number of lymphocytes, plasma cells, histiocytes with an admixture of eosinophils. Most lymphocytes belong to the T system population. In some cases, there are clusters of epithelioid cells, some of which resemble Langhans cells. Granulomas, however, do not undergo caseous decomposition. Granulomatous tissue is found around the edges of the ulcers. Adhesions are observed in the area of the affected area of the intestine. Interintestinal and external fistulas have been described. Perforation into the abdominal cavity is rare due to the development of adhesive serositis. Lymphatic vessels are dilated, the tissues around them are rebuilt (lymphangitis). Inflammation is observed in the regional lymph nodes (mesadenitis).
Clinical picture. The leading signs of Crohn's disease are fever, moderate abdominal pain, inflammatory infiltrates found in the right iliac region, or mesogastrium, or in other parts of the large intestine. There is diarrhea. The clinical picture is variable. In some, the disease proceeds with pronounced inflammatory activity and is severe, in others it is sluggish and latent. The acute form of the disease is accompanied by diarrhea, intestinal bleeding, fever, flatulence, and abdominal pain. Palpation in the mesogastrium (with damage to the small intestine) reveals signs of peritoneal irritation (positive Shchetkin-Blumberg sign), painful tumor-like formations in the abdomen. In some patients, the acute inflammatory process that begins quickly becomes chronic. In other patients, the inflammatory process develops slowly, imperceptibly and is chronic. Diarrhea in such patients is replaced by constipation, low-grade fever is often not noticed. Palpation reveals dense inflammatory infiltrates localized in the mesogastrium or right iliac region.
Some patients have granulomatous formations:
- in the esophagus - granulomatous esophagitis,
- in the stomach – granulomatous gastritis,
- in the large intestine - granulomatous enterocolitis.
In some patients, anal fissures, pararectal fistulas, granulomas and dense infiltrates in the pararectal area are the first signs indicating damage to the small intestine.
A slow-moving inflammatory process often leads to damage to the peritoneum. Acute manifestations of the inflammatory reaction are often perceived as signs of appendicitis, and therefore surgical treatment is used. During surgery, inflammatory changes in the intestines are detected. The same changes are described in yersiniosis (B.E. Strelnikov, 1977). The reason for surgical intervention may be intestinal perforation in the area of ulcers and the occurrence of peritonitis, intestinal bleeding and abdominal adhesions, which cause intestinal obstruction or volvulus and its paralytic dilatation.
Crohn's disease is accompanied by heart damage (tachycardia, extrasystoles, ECG reveals signs of impaired myocardial repolarization, which are caused by intoxication, an allergic reaction or autoallergic myocardial lesions). Liver lesions are often regarded as reactive hepatitis, which usually occurs without jaundice. Anemia is caused by several mechanisms: a decrease in the intensity of iron absorption in the intestine and the occurrence of its deficiency in the body as a result of chronic blood loss, bacterial intoxication leading to hypoplasia of the erythropoietic germ of the bone marrow, and deficiency of vitamins, especially vitamin B12. Arthralgia or polyarthritis are observed, which generally do not lead to ankylosis of the joints. Keratitis, corneal ulcers, iridocyclitis, purulent and granulomatous skin lesions, eczema, furunculosis, erythema nodosum have been described. Most patients exhibit an increase in body temperature in the range of 37-37.6°C. For some, the fever reaches 38-40°C, accompanied by chills and sweats. Incorrect type of temperature curve.
Neutrophilic leukocytosis is observed during exacerbation of inflammation, in most cases it lasts a long time. ESR is increased. Blood clotting is increased. In the blood - dysproteinemia with an increased content of gamma, alpha-1 and alpha-2 globulins, sialic acids, seromucoids and a slightly reduced cholesterol content.
The course of Crohn's disease is long: there are periods of improvement and exacerbation. Deterioration is provoked by infection and nutritional disorders.
Diagnosis . The diagnosis of Crohn's disease is usually made late. In the early period, with the acute onset of terminal ileitis, we are talking about the diagnosis of acute appendicitis.
In chronic cases, endoscopic examination - colonoscopy and laparoscopy - provides significant assistance in diagnosis.
Colonoscopy reveals ulcers, severe intestinal destruction, and tumor-like granulomatous formations.
Laparoscopy reveals signs of limited peritonitis, inflammatory bowel disease and adhesions.
Granulomatous tumor-like formations in Crohn's disease are detected in the esophagus and stomach.
X-ray examination reveals changes in the intestine characteristic of Crohn's disease - the affected part of the intestine takes on the appearance of a “cord” or “rope”. If the terminal ileum and cecum are affected, it is difficult to establish the area of the bauhinian valve - its contours disappear. The altered fragment is usually not filled with a tightly contrasting mass. The relief of the mucous membrane is polypoid in nature, the haustra smooth out or disappear. The contours of the affected area of the intestine are often marked finely or coarsely toothed, often with pointed protrusions characteristic of this disease, which are a reflection of rough slit-like ulcers. Sometimes ulcers, located deep in the intestinal wall, cause on radiographs a peculiar picture of “nail heads” running in regular rows along the contour of the affected intestine. The boundaries with healthy areas are often sharply defined. Granulomatous changes in the intestine are characterized by alternation of affected areas with normal ones. On an x-ray, the mucous membrane acquires a coarse or fine-mesh structure, reminiscent of a cobblestone pattern. Against the background of the reconstructed relief of the mucous membrane, persistent contrasting spots of different sizes are found - longitudinal and transverse erosions and ulcers. With tight contrasting of the intestine, narrowing of the affected area, pseudodiverticulous protrusions, rigidity of the walls, sharpness of the boundaries of the affected and normal areas are revealed, the cellular structure of the relief of the mucous membrane is well defined. Crohn's disease is differentiated from chronic secondary enteritis with gastritis, pancreatitis, hepatitis, chronic ulcerative colitis, intestinal tumors, intestinal polyposis. Each of these diseases is characterized by characteristic clinical, endoscopic and radiological signs. Thus, ulcers in chronic ulcerative colitis are located randomly, have an irregular shape and unclear outline, and are often localized in the distal part of the intestine. In the cicatricial-stenotic form of intestinal tuberculosis, significant wrinkling of the affected area of the intestine is noted, the presence of pronounced adhesions is recorded, the mesenteric lymph nodes are enlarged, the mucous membrane of the colon is restructured without structure during the pathological process.
Treatment . There are no specific treatments for Crohn's disease. The following antibiotics and sulfa drugs are used primarily to combat infection: ampicillin or oxacillin - 2-3 g per day orally or intramuscularly, streptomycin - 1 g per day, neomycin sulfate - 0.1 g 2 times a day, chloramphenicol - 0.5 g 4 times a day, tetracycline - 0.25 g 4 times a day. In Crohn's disease, sulfonamide preparations are advantageous, which are well absorbed in the intestine: biseptol - 2 tablets 2 times a day, sulfalen - 1 g during the first day, and then 0.2 g 1 time per day for 7-10 days and etc. Intestopan (0.24 g) is also used - 2 tablets 3 times a day for 5 days, enteroseptol - 0.25 g 1-2 tablets 3 times a day. If yersiniosis is detected, tetracycline or sulfonamide drugs are used.
For anemia, blood products, plasma, multivitamin preparations, polyglucin, and saline solutions are used. In some cases, in order to influence immunological processes and anti-inflammatory, prednisolone is indicated - 20-40 mg per day or other corticosteroid drugs.
Surgical treatment is used for peritonitis (perforation of an intestinal ulcer), cicatricial narrowing of the intestine and in the presence of abdominal adhesions that stenose the intestines.
Diet . The diet for diseases of the small intestine should be easily digestible, high-calorie, gentle, contain a large amount of vitamins and a sufficient amount of liquid.
Physiotherapy. Reducing the clinical signs of inflammation allows the use of physiotherapy: thermal procedures, inducto therapy, UHF therapy, etc. The procedures have an anti-inflammatory effect and normalize the function of the intestines, stomach, liver and other organs. Salt, carbon dioxide, radon baths are indicated; for constipation - subaqueous, mud intestinal tampons, mud therapy.
Spa treatment is carried out at resorts where there are sources of drinking mineral water and mud therapy: Essentuki, Pyatigorsk, Zheleznovodsk, Borjomi, Truskavets, Morshyn, Druskininkai, Birshtonas, in Belarus - Zhdanovichi, Bobruisk.
If you have any questions, you can get advice from leading clinic specialists.
Causes of ileitis
The most common cause of infectious ileitis is Yersinia infestation. Less commonly, inflammation in the ileum is caused by:
- salmonella;
- coli;
- staphylococci.
Viral acute ileitis is a consequence of the negative effects of rotoviruses and enteroviruses. Giardiasis and helminthic infestations lead to a chronic form of the disease.
Common causes of ileitis include:
- allergic reactions;
- alcoholism, smoking;
- constant consumption of fatty and spicy foods;
- poisoning with heavy metals, poisons, chemical reagents;
- hereditary predisposition;
- intestinal surgery;
- taking certain medications.
Ileitis can also be a symptom of typhoid fever, tuberculosis, and ulcerative colitis.
Symptoms of intestinal ileitis
Acute ileitis manifests itself:
- pain in the iliac region;
- bloating and rumbling stomach;
- loose stools (up to 10 times a day);
- nausea, vomiting;
- high temperature;
- weakness;
- severe headaches.
Due to a disorder of the digestive system, dehydration may occur, which can lead to convulsions, blood coagulation disorders, and hypovolemic shock.
Chronic ileitis is characterized by:
- moderate pain in the right iliac region, around the navel;
- bloating and rumbling stomach;
- watery stools containing undigested food;
- weight loss (due to impaired absorption of vitamins, minerals and nutrients supplied with food);
- osteoporosis;
- hypovitaminosis.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Organization of treatment of ileitis abroad
For several years now it has been helping everyone who wants to receive high-quality diagnosis and treatment of gastroenterological diseases, including treatment of ileitis in leading clinics around the world. We organize and support the treatment of each of our clients on an individual basis.
It is important to understand that each of the following medical institutions has its own characteristics of the range of services provided, as well as location. Therefore, when choosing the best gastroenterology center in your case, you should contact specialists, that is, us!
Diagnosis of ileitis
Since the distal small intestine is almost impossible to examine with an endoscope, the diagnosis of ileitis is based on laboratory methods. The patient is prescribed:
- CBC (increased ESR, leukocyte formula shift to the left, leukocytosis);
- biochemical blood test (lack of microelements and protein is diagnosed);
- bacteriological and virological examination of stool;
- stool occult blood test.
An informative diagnostic method for suspected ileitis is radiography of barium passage through the small intestine. The study makes it possible to detect intestinal motility disorders and intestinal obstruction. The images may also reveal fistulas, strictures, and areas of ileal spasm.
If pancreatitis and cholelithiasis are suspected, the patient is prescribed an abdominal ultrasound.
Terminal ileitis
Share information with your Facebook friends
VK
Question:
Good afternoon.
Please comment on my examinations.
According to colonoscopy from October 2022: terminal ileitis, the ileum is hyperemic, red, the vascular pattern is not visible, hyperplasia. The rest of the intestine is normal.
According to the biopsy, “the picture corresponds to terminal ileitis.”
Since October 2022, treated as Crohn's disease. “Pentas” 4 g per day, the stool returned to normal (before that there was constipation), but as for the other symptoms (pain above the navel, bloating, epigastric pain) - nothing changed, both with and without the diet.
According to the MRI dated January 2022, the conclusion on the sacroiliac joints “the picture may correspond to sacroiliitis.”
The sacrum hurt very badly, the pain was in the left leg and under the shoulder blades. The diagnosis made by a rheumatologist was “Left-sided sacroiliitis FC 1.” Azathioprine was added in March (3 days 50 mg). Then she took tests. There was a norm for ESR, leukocytes, hemoglobin).
On the 4th day I began to feel sick on any food, but especially on meat. The doctor said that this could lead to an exacerbation. I had loose stools with mucus 4 times in a couple of days. I stopped Azathioprine for a week, and after 3 days my condition returned to normal. Then, at the insistence of the attending physician, I began a second round of the same drug. The first analysis after 3 days - everything is normal, except for hemoglobin - 112, lymphocytes - 39.9 (they have been frozen at this indicator for a year already), according to CRP 0.4 (normal up to 5), iron 5.27 (normal 9.0 – 30.4), ferritin – 6 (normal range from 10 to 120). Liver parameters and lipid profile are all normal.
I started taking 100 mg per day on the recommendation of my doctor. On the 10th day of treatment after this analysis, my health began to deteriorate. Nausea, nausea from some smells, severe pain between the navel and stomach and constant bloating. “Duspatalin” does not stop it, “Espumizan” does not help with bloating. Today is the 14th day that I have been taking 2 tablets of Azathioprine and the 17th day of taking it on the second go. My abdominal wall is tense, my stomach hurts and the pain radiates under my shoulder blades - on Mesalazine my stomach didn’t hurt so much, and I ate everything at all. There was only a slight background dull ache, but the joints ached with it. With Azathioprine, as I understand it, until it accumulates, it is useless to wait for the pain in the joints to stop. But I understand that this drug makes me feel bad. The doctor said that if nausea and abdominal pain are difficult to bear, then it should be replaced with Mercaptopurine. In this regard, I have questions.
1) I know that Mercaptopurine is also used in the treatment of malignant tumors. I have a mild form of Crohn's disease, no fever, blood in the stool, diarrhea, fistulas, ulcers, etc. Is it advisable for me to take cytostatics at all due to the addition of sacroiliitis? Maybe you can deal with it somehow locally, considering that on Mesalazine I felt relatively well in the intestines.
2) If yes, does it make sense to replace “Azathioprine” with “Mercaptopurine”, since it has exactly the same side effects? And is it normal to continue taking the drug and ignore the side effects that appear?
3) I have practically no reaction to food (only to very fatty foods, and not always), nothing changes from diets like SUD, FODMAP, tests are mostly normal, CRP, ESR and leukocytes have never increased during the year of illness , according to the biopsy, no one wrote to me that it was Crohn’s disease, only about terminal ileitis, but the doctor told me that these are synonyms, and therefore I would like to ask: this may not be Crohn’s disease based on all the symptoms that I described? I have already been checked for parasites, infections (except for Yersinia) - there is nothing, hidden blood in the stool (no), and sometimes I have doubts whether this is Crohn's disease at all... Thank you!
Answer:
Greetings! I do not comment on treatment; I am not certified to treat gastroenterological pathologies. For endoscopy and biopsy of the small intestine, you need to read the entire pathohistological report. Based on what data is terminal ileitis diagnosed? In the literature, this is indeed equated to Crohn's disease, but there must be inevitable signs in histology. If these signs are not present, but there is no conviction to either make or remove the diagnosis of Crohn’s disease, because They set it not only on the basis of a biopsy, but on the totality of data - endoscopy, CT - enterography, clinic. And tests - you didn’t say anything about specific tests - stool for calprotectin, blood for ASCA IgA/IgG, ANCA and, in rare cases, anti-OmpC antibodies, which increase the likelihood of Crohn’s disease. And in 98% of cases, high calportectin removes the diagnosis of IBS.
print version
TagsCrohn's disease Health ileitis
Treatment of ileitis
All patients who present with symptoms of ileitis should consult a gastroenterologist. The acute form of the disease can only be treated in a hospital. Bacterial inflammation after determining the sensitivity of the microflora to antibiotics is eliminated with the help of antibacterial drugs. For persistent vomiting and diarrhea, infusion therapy with saline solutions and glucose is used. To normalize the absorption of food, enzyme medications are prescribed.
Treatment of chronic ileitis involves following a gentle diet, taking enzymes and medications that help normalize intestinal motility, vitamins, minerals, probiotics, and herbal astringents.
Diet for ileitis
Patients with ileitis are prescribed diet No. 4 according to Pevzner. They can eat:
- yesterday's wheat bread;
- lean meats;
- soft-boiled eggs;
- cereals, pasta;
- porridge with water;
- meat broths.
The following are prohibited:
- raw, fried and hard-boiled eggs;
- fatty meat, smoked meats;
- grape juice, carbonated drinks;
- cabbage, mustard, horseradish, cucumbers;
- milk, cheese.