An important symptom demonstrating problems with the gastrointestinal tract and productive absorption and processing of food is tenesmus. They are characteristic of various diseases and require medical attention. Periodic pain syndrome and poor health force the patient to resort to the services of a doctor. Treatment is dictated by the causes of the disorder, the main emphasis is on eliminating the leading disease. General indications are the use of antispasms to relieve pain.
general characteristics
Tenesmus is a subjective discomfort that is described by patients as a sudden painful urge to defecate, not accompanied by the release of feces.
Sometimes there is a small amount of mucus, blood or pus coming out of the rectum. The pain usually increases within a few minutes and subsides almost completely after visiting the toilet. The pain is localized in the area of the anus, sacrum, perineum, but can also radiate to the overlying parts of the abdomen. False urges have no physiological basis and always indicate the presence of pathological damage to the abdominal or pelvic cavity. Tenesmus is usually combined with other dyspeptic disorders: changes in the frequency and consistency of stools, constant abdominal pain, flatulence, nausea, and vomiting. Bleeding or purulent discharge after painful contractions of the rectal muscles indicates a serious illness and requires mandatory consultation with a doctor.
Prevention
Intestinal problems, including tenesmus and constipation, are caused by eating disorders and lack of a healthy image. It is much easier to prevent a problem than to later treat a full-fledged illness.
To do this, you must follow the following recommendations from experts:
- minimize nervous shock, avoid overexcitation (it has been proven that it is stress and exhaustion that lead to exacerbations);
- Healthy food;
- food should be rich in fiber;
- eat often, but little by little;
- food should be warm;
- exclude alcohol, tobacco, drugs;
- engage in dosed physical activity.
Maintaining the correct regime will prevent a number of unpleasant ailments. If you feel unwell, you should seek medical help rather than carry out treatment at your own discretion.
Causes of tenesmus
The appearance of painful spastic contractions of smooth rectal muscles and perineal muscles, accompanied by an imperative urge to defecate, often develops with various acute and chronic inflammatory diseases of the gastrointestinal tract and urogenital pathology. Tenesmus can occur with tabes dorsalis as one of the manifestations of tabetic visceral crisis. Unpleasant sensations in the anus are sometimes associated with partial strangulation of the hernia.
Diseases of the rectum
Pain, burning and urge when the anal area is affected are associated with increased sensitivity of the rectal membranes to irritants. In such a situation, the ingress of even a small amount of feces or mucus causes sharp spastic muscle contractions. Violation of the coordinated contraction of the anal sphincters leads to retention of contents and the appearance of severe pain. Among the causes of tenesmus are:
- Proctitis
. Inflammatory damage to the rectum occurs with pronounced dyspeptic symptoms, the main of which are false urges, discomfort and itching in the anal area. Pain is associated with constant irritation of the mucous layer and the influence of pro-inflammatory mediators. Proctitis is characterized by the release of a small amount of mucopurulent rectal contents. - Rectal prolapse
. Tenesmus, which develops due to displacement of a section of the intestine beyond the external anal muscular sphincter, is provoked by mechanical irritation of the mucous membrane and compression of the intramural ganglia in the thickness of the rectal wall. In this condition, there is sharp pain in the anus and perineum, a feeling of incomplete emptying after defecation, and a sensation of a foreign body. - Anal polyp
. The urge to defecate occurs only when the size of the benign neoplasm is impressive. Tenesmus is caused by constant pressure and irritation of nerve receptors on the surface of the rectal mucosa. Painful sensations are sometimes accompanied by the release of a few drops of blood during bowel movements, alternating constipation and diarrhea. With a long course of the disease, signs of anemia appear. - Anal fissure
. Rupture of the mucous membrane of the lower rectal sections is manifested by severe pain that occurs during defecation, and may also be accompanied by tenesmus. False urges are caused by the presence of an organic defect in the intestinal wall and a change in the mechanisms of reflex regulation of the act of defecation. With an advanced version of anal fissure, patients are bothered by constant severe pain radiating to the perineal area.
Acute intestinal infections
The development of painful sensations preceding the act of defecation is characteristic of all microbial or parasitic invasions that involve the intestinal mucosa in the process. Pain appears due to the influence of microbes on the intramural autonomic nerve plexuses, which regulate the intensity and sequence of contraction of the smooth muscles of the colon, sigmoid, and rectum. The occurrence of tenesmus is often associated with intestinal infections such as:
- Dysentery
. The disease occurs with damage to the entire large intestine, the formation of ulcers and erosions of the mucous membrane. Dyspeptic syndrome is the leading one in the clinical picture; painful tenesmus is detected against the background of diffuse abdominal pain, nausea and vomiting. Feces during dysentery quickly lose their fecal character, and a small amount of mucus and blood mixed with pus are released from the anus. - Salmonellosis
. Tenesmus is an important sign of the gastroenterocolitic variant of the disease, in which all parts of the digestive tract are affected. Patients also experience diffuse abdominal pain and cramps, nausea, and repeated vomiting. During defecation, a small amount of feces with inclusions of mucus and blood streaks is often released. - Intestinal form of plague
. This form of plague has a severe course, accompanied by a significant deterioration in general condition and severe symptoms of intoxication. Patients complain of sharp, unbearable pain along the intestines and high fever. Spasmodic contractions of the rectal muscles cause intense tenesmus. Other dyspeptic disorders are also typical: nausea, vomiting, diarrhea. - Protozoal infections
. Two diseases occur with predominant damage to the colon and the occurrence of tenesmus - amoebiasis and balantidiasis. With amebiasis, after painful urges, scanty stool is observed in the form of a mucous mass with inclusions of blood (“raspberry jelly”). With balantidiasis, painful urges are combined with scanty bowel movements consisting of feces, mucus and blood. - Parasitic infestations
. Severe colitis with abdominal pain, painful contractions of the rectal muscles, and other dyspeptic symptoms may indicate cavitary myiasis. This disease develops when fly larvae are ingested. Gastrointestinal disorders are common symptoms of chronic schistosomiasis. Tenesmus is often combined with constipation, pain, and decreased appetite.
Chronic bowel diseases
Long-term inflammatory and destructive processes in the intestines inevitably lead to the appearance of unproductive, painful urges to pass feces. Tenesmus develops as a result of disturbances in nervous regulation, which normally realizes its effects through the autonomic ganglia. The condition is aggravated by the destruction of the intestinal mucosa and the appearance of pathological discharge, leading to constant irritation of the rectum. Complaints of tenesmus include:
- Diabetic enteropathy
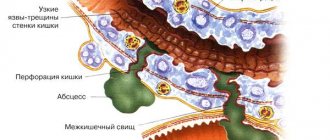
. Dyspeptic symptoms in patients with diabetes are associated with polyneuropathy, in which damage to the autonomic nerve plexuses of the intestinal wall is observed. Tenesmus is more common at night; patients note increased frequency of stools and changes in the consistency of stool. In severe cases, painful urges may develop in combination with intestinal pseudo-obstruction. - Crohn's disease
. Painful contractions of the rectal muscles and anal sphincters are more often observed in advanced forms of the disease. At this stage, patients develop anal fissures and rectal fistulas, through which blood and mucus are released. Tenesmus is usually combined with paroxysmal pain in the right iliac region, nausea, vomiting, and severe weight loss. - Nonspecific ulcerative colitis
. Tenesmus, as a rule, occurs with ulcerative-destructive lesions of the distal parts of the large intestine. Painful urges are associated with the presence of deep defects in the mucous membrane, disorders of innervation and coordinated work of muscle sphincters. Ulcerative colitis is manifested by sharp paroxysmal abdominal pain, scanty bowel movements, and bleeding from the anus. - Chronic colitis
. Pathological urges to pass stool are potentiated by the influence of three factors: bacterial damage to the colon wall, disorders of local immunity, and incoordination of muscle contractions in different parts of the intestine. The most pronounced unpleasant symptoms are with sigmoiditis and left-sided colitis. Tenesmus is combined with cramping pain in the lower abdomen, scanty bowel movements mixed with blood. - Radiation sickness
. Radiation damage to the intestines develops during simultaneous exposure to high doses of radiation and is manifested by dyspeptic symptoms: vomiting, severe abdominal pain, diarrhea. In severe situations, when the cells of the intestinal wall die, painful tenesmus without stool discharge is observed, which is often accompanied by rectal bleeding.
Volumetric neoplasms of the intestine
The development of painful contractions of the intestinal muscles and false urge to go to the toilet in tumor formations is associated with two main reasons: mechanical obstacles to the movement of feces and the germination of tumor tissue into the nerve plexuses of the intestine. With benign neoplasms, the general condition of patients suffers slightly; with malignant tumors, a large complex of extraintestinal pathological symptoms is observed. The most common types of formations in the gastrointestinal tract, in the clinic of which tenesmus is observed, are:
- Anorectal melanoma
. The initial sign of the disease is the appearance of bright red blood on the surface of the stool during bowel movements. As the formation progresses, other signs are also noted: pain in the anus, sensation of a foreign body in the rectum. The cause of painful contractions of the rectal muscles is constant irritation of the mucous membrane and a mechanical barrier to the movement of feces. - Colon adenocarcinoma
. Initially, the tumor has no specific signs and is manifested by dull pain in the abdominal cavity and periodic dyspeptic disorders. As the formation increases, tenesmus is observed associated with partial blockage of the lumen of the colon. Patients are concerned about the passage of small amounts of dark blood in the stool. In severe cases, bleeding from the gastrointestinal tract occurs. - Intestinal polyps
. These neoplasms are benign; unpleasant symptoms are mainly caused by the existence of a mechanical obstruction to the movement of feces and partial intestinal obstruction. Dyskinesia of different parts of the colon is detected, accompanied by a false urge to go to the toilet. Pseudopolyposis of the colon has a similar clinical picture.
Urogenital pathology
The appearance of unpleasant symptoms from the digestive system with lesions of the genitourinary tract is due to the proximity of these organs, general innervation and the presence of pathological viscero-visceral reflexes. Painful sensations are often poorly localized; patients describe them as diffuse pain in the pelvic area. The following urogenital diseases most often lead to the appearance of painful tenesmus:
- Acute prostatitis
. With purulent inflammation of the prostate gland, sharp pain occurs in the pelvic cavity, which radiates to the sacrococcygeal area and rectum. Severe pain syndrome causes pathological spasm of the anal sphincters, which leads to the impossibility of defecation and tenesmus. The disease is always accompanied by dysuric disorders. - Injuries to the genital organs
. When the perineal area is damaged, combined injuries often occur involving nearby anatomical structures. Hematomas and ruptures of the mucous membrane lead to increased irritability of the rectal walls, sharp pain and fecal retention, which is accompanied by a false painful urge to defecate. - Renal colic
. The first sign of the disease is a sharp, cramping pain in the lumbar region, which can radiate to the leg, perineum or anorectal area. The development of tenesmus is caused by a reflex spasm of the entire smooth muscle of the intestine in response to a strong painful stimulus during an attack of renal colic. The condition is accompanied by anuria, vomiting, and tachycardia. - Diseases of the uterus
. Painful contractions of the rectal muscles more often occur with uterine-intestinal fistulas, through which purulent contents enter the rectum and have an irritating effect. Tenesmus and chronic constipation are sometimes a symptom of malignant tumors of the uterus that are located close to the intestinal wall or grow into it.
Purulent inflammation
For abscesses of the abdominal cavity and pelvis, general manifestations are more typical: hectic fever, nausea, tachycardia. Against the background of general intoxication, intense pain occurs in the abdominal area, which intensifies with changes in body position. False urges to defecate develop secondarily as a consequence of reflex irritation of the walls of the rectum and sigmoid colon. With abscesses of the pouch of Douglas, tenesmus can be combined with incontinence of stool and intestinal gases.
Treatment
Treatment of tenesmus includes a set of measures consisting of etiotropic therapy (elimination of the causative disease) and symptomatic therapy, which directly eliminates the patient’s unpleasant clinical manifestations.
A mandatory component of treatment is dietary nutrition, which reduces the load on the intestines and helps normalize peristalsis.
Etiotropic therapy (elimination of causes)
Etiotropic therapy depends on the cause that caused the appearance of tenesmus.
- If this is an infectious process (proctitis or paraproctitis), the patient is given antibiotic therapy.
- In the case of an autoimmune disease (for example, ulcerative colitis), therapy with immunosuppressants (glucocorticoid drugs) is carried out.
- If tumors are present, treatment includes chemotherapy or surgery.
Be sure to read:
Why does pain occur during bowel movements and how to diagnose the cause?
The full range of procedures for each patient is selected individually.
Symptomatic therapy
Symptomatic therapy is aimed directly at eliminating tenesmus. It includes antispasmodics - drugs that relieve spasm of the intestinal muscles, thereby reducing the severity of pain and restoring normal peristalsis. The most common drugs from this group are Drotaverine and No-shpa .
You can also relieve the symptoms of the disease using folk remedies. Patients are often prescribed sitz baths with herbal solutions. They help relieve pain and intestinal spasms. However, such treatment should be carried out exclusively in combination with drug therapy under the supervision of a physician. Self-medication in the event of tenesmus is unacceptable, since the cause of its occurrence may be serious illnesses, without etiotropic treatment of which the patient’s condition will worsen.
Survey
Diagnostic measures are aimed at studying the functional and morphological state of the digestive tract to clarify the cause of false urge to defecate. The examination usually includes laboratory and instrumental methods and helps to identify gastrointestinal diseases at an early stage. The most valuable for making a clinical diagnosis in patients with tenesmus are:
- X-ray examination
. For a detailed study of the structure of all parts of the intestine, radiography of barium passage through the small and large intestines is used. Clearer images of the internal state of the colon wall can be obtained by irrigography with double contrast. - Rectal examination
. Quite informative and accessible methods include digital examination of the internal surface of the organ and anoscopy, which are carried out to clarify proctological pathology, which often leads to the development of tenesmus. - Endoscopy
. Colonoscopy is the main and most diagnostically valuable study, during which it is possible to assess in detail the condition of the mucous layer of all parts of the large intestine, visualize signs of inflammatory lesions and tumor formations. According to indications, a biopsy of individual areas is taken during the examination. - Ultrasonography
. Abdominal ultrasound is a non-invasive method often used as a screening tool to identify patients with gastroenterological pathology. Survey sonography of the abdominal cavity helps to detect signs of inflammation, voluminous neoplasms, against which tenesmus is noted. - Coprogram
. In diseases where tenesmus is a symptom, changes in stool tests are often detected. All patients are prescribed a standard stool examination; if an infectious etiology of the disease is suspected, an extended bacteriological culture and stool analysis for helminth eggs are performed.
To clarify the diagnosis, computed tomography, anorectal manometry, and laboratory blood tests for specific antibodies can be performed. A gastroenterologist or proctologist examines a patient with tenesmus. After ruling out diseases of the digestive tract, additional examinations of the genitourinary organs may be prescribed, aimed at identifying the causes of the disorder.
Colonoscopy
General information
The name of the symptom comes from the Greek word teinesmos, which translates as “futile urge.”
This symptom without a pain reaction is called a false urge.
Both false and unsuccessful urges accompanied by pain arise as a result of a specific reaction of the rectum or bladder to various stimuli.
The origin of tenesmus was studied by M.I. Pevzner, the founder of clinical gastroenterology and dietetics of the USSR, as well as the German doctor H. Strauss, who studied the digestive system.
Pathogenesis
The mechanism of development of tenesmus is associated with spastic contraction:
- intestinal smooth muscles (mainly the rectum and sigmoid colon);
- Bladder.
Spastic muscle contraction leads to voluntary contractions of the abdominals, muscles of the pelvic floor and perineum.
As a result of the simultaneous spastic contraction of this muscle group without concomitant relaxation of another muscle group (especially the sphincters), it becomes difficult to remove the contents of the bladder or rectum, or a jerky ejection of small portions of excrement occurs.
The release of mucus, pus or blood during tenesmus depends on the pathological process that caused the tenesmus.
Muscle hypertension underlying tenesmus depends on irritation:
- nerve plexuses of the muscle wall;
- irritation of the hypogastric nerves and pelvic plexus coming from the central nervous system.