The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
Trichinosis is one of the types of helminthiasis. The disease is caused by the ingestion of a small parasite belonging to the class of nematodes. Sexually mature Trichinella lays its larvae in the human intestine, and after that, the larvae enter the muscles through the bloodstream and remain there in a dormant state. At 3-4 weeks from the start of infection, the larvae develop and become covered with a capsule. The causative agent of the disease is a roundworm up to 0.5 mm long, taking the shape of a spiral.
Prevalence of trichinosis
Trichinosis in humans belongs to the category of biohelminthiases, as it is caused by parasitic worms - Trichinella. The disease is diagnosed in both animals and humans. The main animal species most often affected by trichinosis are: wolf, fox, bear, badger, wild boar. Domestic pigs are also susceptible to this type of helminthiasis. This usually happens when pigs graze freely, when the meat of dead animals and small rodents becomes available for them to eat.
Reasons for the widespread prevalence of trichinosis:
- The pathogen's good adaptability to high and low temperatures ensured its residence in many climatic zones;
- The human body is extremely susceptible to this disease;
- Group outbreaks of helminthiasis are not uncommon among members of one team or one family who have consumed meat with Trichinella;
- Repeated cases of infection occur due to unstable immunity formed after the initial invasion.
Trichinella are modified, new forms of nematodes that do not form a capsule appear, as well as species that parasitize birds.
Classification
Depending on the clinical picture, several forms of trichinosis are distinguished:
- Atypical (erased) trichostrongyloidiasis is asymptomatic and abortive, and there are no clinical manifestations or they are mild and can be quickly stopped, for example, trichostrongyloidiasis anemia is also possible , has a favorable prognosis.
- Typical, which, depending on the severity of the course, can be mild, moderate and severe. They differ in different lengths of incubation (with mild, more protracted ones), duration of fever (less or more than 2 weeks, where persistent long-term is typical for severe cases), severity of muscle pain, type of rash and the presence of complications.
Animal trichinosis
Trichinosis occurs not only in humans, but also in animals, because these worms can infect any species of mammals. All individuals who eat meat containing cysts are at risk. To release Trichinella from the capsule, gastric juice is needed, then after entering the intestines after a couple of days, the parasites are capable of reproducing. Being viviparous, young Trichinella can penetrate any tissue, but survive exclusively in skeletal muscles, which is why high-quality testing of meat from pigs and other domestic and wild animals for trichinosis is so important in our time. This is because there are two ways of spreading parasites - primary (natural), which involves predatory mammals (wolves, foxes, wild boars, bears), pinnipeds, insectivores, etc., as well as secondary synanthropic - where connections are maintained by domestic animals, synanthropic rodents , and the person becomes the final link of the invasion - a dead end of the circulation. A mixture of synanthropic and natural distribution links is possible.
The main ways of spreading trichinosis are 1 - synanthropic, 2 - natural
Most often, local outbreaks or sporadic cases occur in such regions of the Russian Federation as the Krasnodar Territory, North Ossetia, Kamchatka, Magadan Regions, Krasnoyarsk and Primorsky Territories, as well as in Belarus, Lithuania and right-bank Ukraine and are most often associated with hunting and eating game meat.
Interesting to know! Presumably, members of Andre's Arctic expedition who ate contaminated polar bear meat died from trichinosis.
Methods of infection with trichinosis
Trichinella enters the human body orally by consuming contaminated meat. Parasites in meat are killed during heat treatment, so the main risk comes from undercooked, dried and raw meat. Infected pork, seal, bear meat, and wild boar meat are especially dangerous.
The development of trichinosis in the human body after infection:
| Time since infection | Process |
| 1-1.5 hours | The larva freed from the capsule penetrates the mucous membrane of the stomach or duodenum and the connective tissue located underneath it. |
| 1 day | The larva develops into a mature worm. |
| 3-4 days | A mature female worm lays larvae (one female is capable of producing from 100 to 2000 new worms). The larvae enter the blood vessels and are delivered through the bloodstream to the muscles. |
| 42-56 days | The time during which an adult female worm is able to lay larvae. |
| 17-18 days from the moment the female deposits larvae | The larvae mature in the muscles and become infective to a new host. |
| 3-4 weeks from the moment the female lays larvae | The larva is covered with a capsule. A year later, the capsules become calcified. |
| 10-40 years | This is the period during which the larva in the form of a capsule is able to survive in the host’s muscles. |
The first signs and symptoms of trichinosis
Trichinosis in humans does not cause visible physical harm to the body. There are no changes in muscle tissue. The proteins that make up the parasite's body are harmful to health. They are very powerful allergens, foreign substances. The severe allergic reaction caused by them leads to damage to blood vessels and joints.
Incubation period of trichinosis. Lasts from 5 to 30 days, more often – 10-25 days. There are no symptoms of the disease. There is a pattern - the more severe the form of helminthiasis, the longer the latent (hidden) period.
High period. A long period of development of symptoms indicates the development of a severe form of trichinosis.
Mild and moderate form - symptoms:
- Hyperthermia. The temperature rises slightly, more than 37°C, the daily amplitude fluctuates within 1°C.
- Swelling on the body and limbs. Its cause is an allergic reaction to the introduction of a foreign protein. A characteristic symptom is a “frog face” in the patient.
- Muscle pain in the upper and lower extremities, muscles of the back, neck, eyes, pharynx, peritoneum. Intense pain begins in the calf muscles, affecting the cervical and chewing muscles. The pain intensifies with palpation and movement. They may begin to bother the patient from 1-3 days of introduction of the parasite into the body. The early appearance of muscle pain is a sign of a severe form of trichinosis.
Skin rash. Has different forms:
- In the form of allergic urticaria - pink blisters of various sizes that turn pale when pressed;
- Itchy blisters raised above the surface of the skin (utricar rash);
- Groups of plaques merging with each other (papular rash).
Complications in severe forms of trichinosis:
- Meningoencephalitis is an inflammation of the membranes of the brain.
- Pneumonia (eosinophilic pneumonia). The disease is caused by an increased concentration of eosinophils, products of an allergic reaction, in the lung tissue. Pleurisy and symptoms of bronchial asthma may develop.
- Myocarditis is inflammation of the myocardium due to allergies and excessive immune response. More often than other complications it causes death in patients.
- Nephritis is inflammation of the kidney tissue.
- Hepatitis is inflammation of the liver.
- Intense pain in the muscles leads to partial or complete impairment of mobility.
Mortality in severe forms of the disease is 10-30% of the total number of patients. The most common period for deaths to occur is 4-8 weeks from the onset of infection. In milder forms, patients recover after 5-6 weeks.
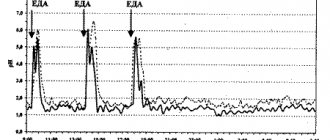
Symptoms of trichinosis depending on the stage of the disease
The manifestation of trichinosis at an early stage of infection depends on the concentration of parasites in the body. Further development of the disease depends on the spread of larvae in the muscles and the state of the patient’s immune system. The most severe complications of helminthiasis are associated with the body’s inadequate response to the introduction of a foreign protein into the body, and not to the activity of Trichinella and its larvae.
| Stage | Time since infection | Symptoms |
| Trichinosis invasion (penetration into the body) | 7 days | Trichinella larvae that enter the body orally are found in the small intestine. They become attached to the mucous membrane, causing inflammation of the intestinal wall. Within 55 days, the development of larvae into sexually mature individuals occurs in the small intestine, their fertilization and the emergence of a new generation of larvae. One female Trichinella produces up to one and a half thousand individuals. Symptoms of the early stage of trichinosis:
|
| Dissemination (spread of larvae throughout the body) | 2-4 week | The larvae begin their migration in the tissues of the body, penetrating into the muscles. They make their way from the intestines through blood and lymphatic vessels. After penetration into the blood, Trichinella larvae become attached to muscle fibers. They develop and grow, releasing allergens into the blood. Intoxication begins in the body, allergic reactions develop.
|
| Encapsulation stage | 6 weeks to 6 months after infection | During this period, tissue regeneration occurs. The larvae reach a size of 0.8 mm and take on a spiral shape. The foreign inclusion (larva) is fenced off by the capsule from the muscle tissue and stops its development. Trichinella toxins do not enter the body, the symptoms of the disease become less intense and gradually cease. The capsule becomes calcified, these salts can destroy the larva. Sometimes the Trichinella larva remains viable for up to 25 years, without affecting a person’s well-being. Symptoms of the regeneration phase:
Symptoms of the disease can be blurred and disguised as other diseases. There are three signs of trichinosis that are always recorded by a doctor after eating contaminated meat:
|
Symptoms of trichinosis in humans may be similar to manifestations of myositis, allergies, or infectious diseases. This picture leads to the fact that the patient does not suspect that he has helminthiasis.
Symptoms of trichinosis in children
To become infected, it is enough for a child to eat a small piece of meat with Trichinella weighing 10-15 g, which has not undergone full heat treatment. The latent period lasts from 5 to 45 days. The shorter this period, the more severe the form of the disease in the child.
- Symptoms at an early stage. Lasts 7-14 days, after recovery there are minor symptoms for 7-10 days.
- Hyperthermia up to 38.5°C:
- Slight puffiness of the face;
- Mild muscle pain;
- Swelling of the eyelids;
- Increase in eosinophil concentration by 10-12%.
- Symptoms are at a moderate stage. The acute period lasts up to 3 weeks, rehabilitation – 2-3 weeks after recovery.
- Hyperthermia up to 40°C, antipyretic drugs reduce it by no more than 1°C;
- Pain in muscles, joints, stomach and throat;
- Skin rash;
- Swelling of the face;
- Results of a general blood test: ESR is increased (above 17 mm/h), leukocytes are increased (up to 8.8·109/l), the concentration of eosinophils is increased to 25-40%.
- Symptoms at a severe stage. He is being treated in the infectious diseases department of the hospital; without therapy, the child may die.
- Hyperthermia up to 41°C;
- Enlarged liver and spleen;
- Central nervous system disorders: delirium, agitation, epileptic seizures;
- Attacks of severe abdominal pain;
- Diarrhea, nausea, vomiting;
- Severe muscle pain complicated by cramps;
- Subcutaneous hemorrhages and rash;
- General blood test indicators: Leukocytes up to 30-40x109/l; ESR up to 50-60 mm/h; eosinophil concentration up to 80 - 90%;
- Casts and proteins in the urine.
Treatment of trichinosis in children is carried out with anthelmintic drugs (Tiabendazole, Vermox) in accordance with the body weight and age of the child.
Drugs for the symptomatic treatment of trichinosis:
- Ibuprofen, Paracetamol - to reduce temperature, relieve pain;
- Cetrin, Loratadine - antihistamines to reduce intoxication and allergy symptoms;
- Papaverine, No-shpa - antispasmodics to reduce pain;
- Vitamins C and B to improve immunity.
Rehabilitation after illness is carried out with the help of massage sessions, baths with sea salt and medicinal herbs, and a complex of therapeutic exercises.
Pathogenesis
To become infected with trichinosis, a person only needs to eat bacon, bacon or meat, most often pig, that has been infested with Trichinella larvae. The infection process does not cause discomfort or symptoms during the initial penetration of Trichinella into the intestines. There, sexually mature individuals are located between the villi of the lining mucous membrane and penetrate it with the anterior end.
Fertilization and release of live larvae takes a couple of days. They are no more than 100 microns long and are able to penetrate the lymphatic and then the circulatory system and spread with its current. The larvae usually settle in the most actively working striated muscles, well supplied with blood and saturated with oxygen, that is, in the legs of the diaphragm, intercostal and abdominal muscles, in the tongue, in the muscles of the larynx and masticatory muscles. A week later, they reach other muscle fibers, breaking through the sarcoma with a stylet. Then comes the invasive stage - the parasite curls up into a spiral and forms around itself a small capsule measuring no more than 0.4 X 0.25 mm, which subsequently calcifies within two years. There, many larvae die, but some of them can remain viable for more than 25 years.
Life cycle inside a person
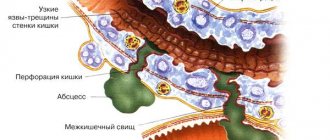
Living larvae secrete metabolic products that are sensitizing and toxic to the human body, therefore the development of catarrhal-hemorrhagic inflammation in the intestinal walls and general allergic reactions of the body. Trichinosis can also lead to damage to internal organs and tissues of the central nervous system, including myocarditis, myocardial dystrophy, vasculitis, meningoencephalitis, pneumonia .
Information about the structure and life cycle of Trichinella
Trichinella parasitizes the small and initial sections of the large intestine and is characterized by sexual dimorphism. Mature females are usually 1.5 mm long - no more than 1.8 mm, while males can be from 1.2 to 2 mm, but a fertilized female can reach 4.4 mm.
The structure of the intestinal form of Trichinella
The life cycle of males ends immediately after fertilization, while females, after a couple of days, begin to release larvae (on average 0.2-2 thousand), which can take 4-6 weeks and also ends with their death. The produced larvae are able to penetrate through the thickness of the intestinal mucosa into the vessels of the circulatory and lymphatic systems, spreading throughout the body and settling in the tissues of the striated muscles.
Forms of existence of trichinas
Young larvae penetrate the cell membranes of myocytes and reach muscle fibers. In this case, the muscle fibers are partially destroyed and a cellular infiltrate is formed around the larvae, as well as the gradual formation of a fibrous capsule over 3-4 weeks, which has its own network of blood vessels and allows maintaining the exchange of substances between the parasite and the host. The viability of the larvae persists for many years, with gradual thickening of the capsule walls and their impregnation with calcium salts.
Diagnosis of trichinosis
General blood analysis. With trichinosis in a person, the content of eosinophils, a type of white blood cell, increases significantly in the blood. The concentration of white blood cells most often increases with severe allergic reactions, including allergies that accompany trichinosis.
Changes in blood composition diagnosed with trichinosis:
- The number of eosinophils reaches from 50 to 80% of the total number of leukocytes;
- An increase in the concentration of leukocytes is a sign of activation of the immune system and the presence of an inflammatory process in the body.
These symptoms appear immediately after infection and persist 2-3 months after recovery.
Serological diagnosis. An analysis of the blood reaction to the addition of antigens obtained from nematode larvae is carried out. Antibodies to them are formed as a reaction to the introduction of helminths.
Types of serological diagnostics:
| Abbreviation | Decoding | The essence |
| RSK | Complement fixation reaction | If there are antibodies in the patient’s blood, they combine with the antigen and attach a complement molecule, a special substance involved in immune reactions. In this case, the reaction will be considered positive. |
| RNGA | Indirect hemagglutination reaction | It is based on the ability of red blood cells to stick together when there is an antibody and antigen on their surface. |
| ELISA | Linked immunosorbent assay | A reaction is carried out between antibodies and antigens. Special enzymes serve as a marker to evaluate the result. |
| REEF | Immunofluorescence reaction | The material contains a special label that causes it to glow after the antibody reacts with the antigen. |
| REMA | Reaction of enzyme-labeled antibodies. | A special label, which is an enzyme, allows you to evaluate the result. |
Intravenous allergy test. It is carried out to provoke an allergic reaction in response to the introduction of trichinosis antigen. A portion of the antigen solution is injected under the skin. The presence of the disease is diagnosed by the appearance of hyperemia and redness at the injection site. This method can diagnose trichinosis starting from 2 weeks of nematode infection. A positive allergy test result lasts for 5-10 years.
Muscle biopsy. It is carried out in the absence of a positive result from other research methods. The biomaterial obtained with a needle from the patient’s muscle is examined under a microscope.
Study of meat from sick animals. At multiple magnification, the meat of the animal, the suspected source of infection, is examined. Using a microscope, capsules with larvae are detected in the tissues of a sick animal.
Cause
The causative agent in all cases is Trichinella spiralis or Trichinella nativa. A nematode up to 0.5 cm long is a female, up to 0.2 cm long is a male.
You can become infected with the parasite by eating contaminated meat. The main source is predatory animals: bears, foxes, wolves, and wild boars. Animals that have reached 7-8 years of age are carriers, about 90% are infected.
Quite often, domestic pigs can also become a source if they have eaten contaminated meat from dead animals, including dead rats.
Treatment of trichinosis
Anthelmintic drugs (treatment aimed at combating the causative agent of the disease):
- during the first three days; 100 mg 3 times a day;
- next 10 days; 500 mg 3 times a day.
Children under 7 years of age: 25 mg of the drug 3 times a day. Children aged 7; 9 years: 3 times a day, 50 mg. Over 10 years old:
- during the first three days; 100 mg 2 – 3 times a day;
- then for 10 days, 500 mg 3 times a day.
Take after meals. (;Complete reference book of an infectious disease specialist; edited by DMN, prof., corresponding member of RAE and REA Eliseeva Yu.Yu.,; Eksmo;, 2007)
| A drug | Indications and effects | Mode of application |
| Mebendazole | It disrupts the absorption of glucose by worms and the synthesis of ATP, the main carrier of energy, in their body. As a result of metabolic disorders, the worms die. Mebendazole is contraindicated in pregnant and nursing mothers. | 0.3 – 0.6 g (1 – 2 tablets of 0.1 g three times a day) for 10 – 14 days. (Reference Vidal, 2010) |
| Albendazole | It works almost the same way as Mebendazole. Most active against larval forms of worms. Available in the form of tablets of 0.2 grams. Contraindicated in pregnancy and retinal diseases. | Take at the rate of 10 mg per kilogram of the patient’s body weight for 10 to 14 days. (Reference Vidal, 2010) |
| Vermox | Active substance; mebendazole. Efficiency is 90% | Adults take 100 mg 3 times a day for the first three days. The next 10 days – 500 mg 3 times a day Children under 7 years of age: 25 mg of the drug 3 times a day. Children aged 7 – 9 years: 3 times a day, 50 mg. Children over 10 years old: take 100 mg 2-3 times a day for the first three days, then 500 mg 3 times a day for 10 days. Take after meals. (“Complete reference book of an infectious disease specialist”, edited by DMN, prof., corresponding member of RAE and REA Eliseeva Yu.Yu., “Eksmo”, 2007) |
| Thiabendazole | Efficiency is 90%. | Dose for children and adults – 25 mg per kg body weight (dose (mg) = body weight (kg) * 25). Divide into 2 doses every 12 hours. The course of treatment is continued for 3–5 days, after which, according to indications, it is repeated after 7 days (as prescribed by a doctor). Take one hour after meals. (“Complete reference book of an infectious disease specialist”, edited by DMN, prof., corresponding member of RAE and REA Eliseeva Yu.Yu., “Eksmo”, 2007) |
Treatment of trichinosis symptoms
| Anti-inflammatory drugs (Voltaren, Diclofenac, Diclogen, Ortofen) | They help cope with inflammation that was caused by allergic reactions in the patient’s body. | As prescribed by a doctor. |
| Antipyretics (Paracetamol, Aspirin, Acetylsalicylic acid, Nurofen, Ibuprofen) | Indicated when body temperature rises above 38;C. | As prescribed by a doctor. |
| Preparations of hormones of the adrenal cortex - glucocorticoids | Hormonal agents that suppress the immune system and allergic reactions. | Hormonal drugs are used only strictly as prescribed by a doctor. |
A high probability of death, frequent progression of the disease to a severe form, and a large number of complications are good reasons for treating trichinosis exclusively in a hospital setting. Despite this, from 10 to 30% of cases of the disease are fatal.
Patients with severe muscle damage require careful care, as patients are completely immobilized and bedridden. To restore mobility, patients are rehabilitated using massage and physiotherapeutic methods.
Symptomatic treatment of trichinosis in humans is supplemented with vitamin therapy, drugs to stimulate blood circulation, to protect the liver and brain (if these organs are affected).
Diagnosis
The diagnosis is established on the basis of a characteristic wedge, picture, epidemiol. medical history (eating raw or insufficiently heat-treated animal meat, which is a possible source of infection). The most difficult diagnosis is severe forms of T., which appear during epidemic outbreaks earlier than other forms, and often begin atypically - with diarrhea. Confirmation of the diagnosis is the detection of Trichinella larvae in meat, which is considered the cause of infection. In case of single diseases, in the case of an unclear source of invasion, a diagnostic muscle biopsy is performed (see Helminthological research methods). Serological reactions are used - RSK, indirect hemagglutination reaction with antigen (see Serological tests).
Differential diagnosis during outbreaks of T. is carried out with acute respiratory viral diseases (see), typhoid fever (see), paratyphoid fever (see), food toxic infections (see Food toxic infections), in children - with measles (see), rubella (see), scarlet fever (see). The main distinguishing features of T. are pronounced eosinophilia, decreased ROE, and high aldolasemia. In case of single diseases, trichinosis is differentiated from Quincke's edema (see Quincke's edema), an allergic reaction to drugs (see Drug allergy), dermatomyositis (see). Granulomatous changes in muscle tissue during dermatomyositis can be interpreted as trichinosis, but unlike T., the skin itself is affected.
Prevention of trichinosis
Measures to prevent trichinosis:
- Cooking meat (especially pork) should be done at a high temperature - at least 74°C inside the piece of meat for at least 15 seconds. Under such conditions, the Trichinella larvae will certainly die if they have not yet become covered with a calcified capsule. Otherwise, the larvae will not be harmed even with such heating. The larvae manage to become covered with a capsule during a long course of the disease in an animal that carries Trichinella.
- An effective way to destroy Trichinella is freezing for 20 days at -15°C, or holding for three days at -20°C.
- When breeding pigs, they should not be allowed to graze freely to prevent animals from eating contaminated carrion. It is necessary to regularly destroy rats in the place where the animals are and in the farmyard.
- Eating meat from wild animals infected with trichinosis is especially dangerous. The types of nematodes that parasitize the muscles of bears, badgers and seals are noticeably different from Trichinella pigs. They do not die even after prolonged freezing. Long-term thermal cooking of such meat is required. Wild bird meat can also be dangerous in this regard.
Mass events to prevent outbreaks of trichinosis
Rospotrebnadzor systematically monitors the living conditions of animals intended for breeding for meat. Meat cannot be sold without testing it for trichinosis. Such control is carried out at the market and in specialized stores. The safety of meat sold in spontaneous retail outlets is not guaranteed.
Geographical distribution
T. is ubiquitous in nature. In the last 20-30 years, the distribution of human T. incidence in the world has changed. The incidence has decreased significantly in Eastern European countries and the USA. Thanks to the improvement of the pig breeding system, T. is practically not registered in Romania, Hungary, and Bulgaria. A stable focus still remains in the east. parts of Poland. Individual diseases and outbreaks are recorded in northern Italy, on the island. Sicily, in France, Spain, the Netherlands. The incidence of trichinosis has increased in Asian countries, on the Pacific Islands, Mexico, and Chile. T.'s diseases began to be recorded in Africa. In Asia, the greatest prevalence of T. is noted in Lebanon; individual diseases are recorded in Iran, Iraq, and India; outbreaks of T. are observed in Indonesia, Thailand, and Laos.
In the USSR, T. has been registered in 65 species of wild animals. By 1978, the incidence of T. in pigs had sharply decreased. The incidence of trichinosis in the BSSR, which was the main focus of T. in our country, has decreased 38 times over the past 15 years. In connection with the development of the territories of the North and East of the country, the number of T. diseases in people who eat wild animal meat increased, so in 1975 in the RSFSR it accounted for up to 96% of all T. diseases, while in 1946-1967 - only 24.4%.
How to test meat for trichinosis?
Trichinella larvae are found in many animal species. Meat consumed by humans must undergo epidemic control. The most dangerous types of meat are pork, bear meat, and wild boar meat.
The appearance of contaminated meat is practically no different from that of a healthy carcass. The concentration of trichinella in the affected tissue reaches 200 pieces per 1 gram. Meat examination is carried out in a laboratory using a microscope. After analysis, a special mark is placed on the carcass.
Where can a test for trichinosis be done?
At the sanitary and epidemiological station or at the veterinary laboratory of the food market, samples are taken from the animal carcass. Samples of no more than 5 g are taken from areas of increased blood supply: masticatory muscles, tongue, intercostal muscles, diaphragm.
Even one detected trichinella is a reason for the destruction of the entire carcass, which from now on is considered unfit for food.
There is no veterinary laboratory control in spontaneous markets, during mass slaughter of livestock, or when eating hunting trophies. Unfortunately, Trichinella can be found in 30% of meat considered edible. Prevention of infection is thorough cooking of meat. This is especially true when eating game in regions where trichinosis is endemic.
Immunity
After suffering from T., due to the presence of parasite larvae in the body of the recovered person, non-sterile immunity remains for life. Its intensity depends on the intensity of the invasion, the frequency of infection, the characteristics of the pathogen strains, and the constitutional characteristics of the patient’s body. The local residents of the north. districts of the USSR, Canada, USA, who constantly eat meat of wild animals that have not undergone heat treatment and are affected by T., the disease manifests itself clinically extremely rarely.