Rectal prolapse (rectal prolapse, pelvic floor prolapse)
Rectal prolapse is a condition when the rectum or part of it loses its proper position inside the body, becomes mobile, stretches and comes out through the anus.
Rectal prolapse is divided into two types: internal (hidden) and external. Internal rectal prolapse differs from external rectal prolapse in that the rectum has already lost its position, but has not yet come out. Rectal prolapse is often accompanied by weakening of the anal canal muscles, which leads to incontinence of gas, feces and mucus. The problem of rectal prolapse occurs quite often in our patients. This condition is also known as rectal prolapse or pelvic floor prolapse and is more common among women than men.
In women, the main factors for the development of rectal prolapse are pregnancy and childbirth. The prerequisites for the appearance of the disease in men may be regular physical activity or the habit of strong straining.
Rectal prolapse usually does not cause pain at the very beginning of the disease. The main problems with rectal prolapse for patients are a feeling of discomfort and a foreign body in the anus, as well as an unaesthetic appearance, which significantly worsens a person’s quality of life.
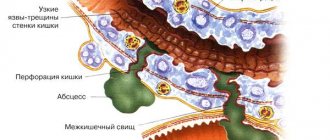
Rectal prolapse usually responds well to treatment and has a low recurrence rate (recurrence of the disease)—only about 15%. Complications in treatment usually arise when the patient seeks specialized help late and attempts to self-diagnose and treat. The result of these actions is lost time for success in treatment. If no treatment is taken, part of the prolapsed intestine will gradually increase, in addition, the anal sphincter will stretch, and the likelihood of damage to the pelvic nerves will also increase. All this entails the following complications:
- Ulcers of the rectal mucosa.
- Tissue death (necrosis) of the rectal wall.
- Bleeding.
- Incontinence of gas, mucus and feces.
The length of time over which these changes occur varies widely and differs from person to person; no doctor will give an exact time frame for how long these serious problems can occur.
Normal condition
With loss
Symptoms and signs of dolichosigma
Symptoms of dolichosigma in children are expressed depending on the degree of progression of the disease and depend on the degree of progression of the disorder of morphological and functional signs of the intestine. The main symptom is constipation, persistent or chronic. Intestinal dysfunction is accompanied by pain and swelling. Feces change their shape and size, become dense, voluminous and have a foul odor.
Due to indigestion, there is a deterioration in the absorption of minerals and vitamins, which leads to a deterioration in the body's protective functions. In children with dolichosigma, the abdomen protrudes with severe thinness. There is a coating on the tongue and an unpleasant smell of breath. As a rule, such children are pale, their hair is dull, their nails are brittle, and they also have dark circles under their eyes.
Additional symptoms of an elongated sigmoid colon in children:
- headaches and irritability;
- rapid heartbeat, pain in the shoulder girdle;
- worsening of the condition with physical activity and consumption of large portions;
- improvement in the supine position.
Pain and pressure in the iliac region periodically appear. On palpation, severe discomfort occurs. The pain syndrome is accompanied by flatulence and spasms. Nausea indicates intoxication of the body. Develops when a child does not have bowel movements for 3-4 days or more.
As a result of the accumulation of feces in the intestines, toxins accumulate and the processes of fermentation and putrefaction develop. If primary signs of dolichosigma occur, immediately contact a gastroenterologist or proctologist for diagnosis and treatment.
Rectal prolapse and hemorrhoids
One of the common reasons why a patient does not see a doctor immediately after a problem arises is the external similarity of the manifestation of the disease with hemorrhoids, which they try to cure on their own - with suppositories and ointments. In fact, rectal prolapse and hemorrhoids are completely different diseases, which may actually appear similar in appearance due to the influx of tissue from the anal canal. Only with hemorrhoids does the hemorrhoidal tissue fall out, and with rectal prolapse does part of the rectum fall out. Also, both diseases have some similar symptoms, such as bleeding.
It is important to remember that incorrect diagnosis and incorrect treatment will never lead to the expected positive effect, and in some cases will worsen the problem.
Prevention measures
As a preventive measure for a healthy child, and especially babies born early with low birth weight and with congenital anomalies, doctors advise:
- do not allow early potty training under the pretext of preparing for kindergarten;
- do not allow sitting on the potty for a long time to no avail “with fairy tales” and songs;
- take the problem of constipation or diarrhea seriously, and for nursing mothers to control their diet;
- consult a pediatrician more often, do not apply treatment without examination by a doctor.
Unlike the problem of intestinal prolapse in adults (especially in old age), childhood diseases are usually caused by acute causes. Seeing a doctor in a timely manner means preventing an advanced case. The future of their heirs depends on attentive parents.
Causes of the disease
What causes rectal prolapse?
- Anything that increases pressure inside the abdomen can cause rectal prolapse to develop. Constipation, diarrhea, prostatic hyperplasia (straining when urinating), pregnancy and childbirth, persistent cough.
- Damage to the anus, pelvic floor muscles, back nerves, pelvic nerves during previous surgery or injury.
- Intestinal infections with certain types of germs called parasites (such as amoebiasis and schistosomiasis).
- Some diseases of the nervous system, such as multiple sclerosis.
- Mental health conditions associated with constipation such as: depression, anxiety, side effect of medications used to treat mental disorders.
Symptoms of rectal prolapse
- The most common symptom that should alert you is the sensation of a foreign body in the anus coming out of the anus. In the early stages, this may happen when straining, but as the condition progresses, it can happen when coughing, sneezing, standing up, or walking. In the early stages, when the prolapse is relatively minor, manual assistance (using the fingers to move the intestines inward) will be successful, but over time this will also become impossible.
- The feeling of incomplete bowel movement usually occurs in the case of hidden (internal) rectal prolapse.
- Fecal incontinence leading to soiled clothing. Incontinence of gas, loose and hard stools, or mucus/blood may also occur.
- Constipation is noted in up to 30-50% of patients with rectal prolapse. Constipation can occur due to congestion in the rectum, creating a blockage that gets worse with strain.
- Pain and discomfort in the anus.
- Bleeding – Over time, the prolapsed mucosa can become thick and ulcerated, causing bleeding.
Functional bowel diseases in children
F
Functional disorders (FD) of the gastrointestinal tract occupy one of the leading places in the structure of the pathology of the digestive organs. For example, recurrent abdominal pain in children is functional in 90–95% of children and only in 5–10% is associated with an organic cause. In approximately 20% of cases, chronic diarrhea in children is also based on functional disorders. Diagnosis of FN often causes significant difficulties for practitioners, leading to a large number of unnecessary examinations and, most importantly, to irrational therapy. At the same time, one often has to deal not so much with ignorance of the problem, but with its lack of understanding.
According to modern concepts, FN is a multivariate combination of gastrointestinal symptoms without structural or biochemical disorders (DA Drossman, 1994).
FN is most often caused by a violation of the nervous and humoral regulation of the digestive tract. They have different origins and can occur as a result of diseases or pathological conditions of the nervous system: immaturity of neuromuscular transmission, damage (ischemia or hemorrhage) to the brain stem and upper cervical spinal cord, trauma to the upper cervical region, intracranial hypertension, myelodysplasia, infection, tumor, vascular aneurysm and etc.
An attempt to create a classification of functional disorders in childhood was undertaken by the Committee on the Study of Functional Disorders in Children and the International Working Group on the Development of Criteria for Functional Disorders (Rome Group II) together with the staff of the University of Montreal Clinic (Committee on Childhood Functional Gastrointestinal Disorders, Multinational Working Teams to Develop Criteria for Functional Disorders, University of Montreal, Quebec, Canada). This classification is based on clinical criteria, depending on the prevailing symptoms:
- disorders manifested by vomiting
- regurgitation, rumination and cyclic vomiting; - disorders manifested by abdominal pain
- functional dyspepsia, irritable bowel syndrome, functional abdominal pain, abdominal migraine and aerophagia; - defecation disorders
- childhood dyschezia (painful defecation), functional constipation, functional stool retention, functional encopresis.
Irritable bowel syndrome
Intestinal functional disorders according to ICD-10 include irritable bowel syndrome
(IBS).
Domestic authors include functional flatulence, functional constipation, and functional diarrhea in the same group. According to ICD-10, intestinal functional disorders include (IBS).
Domestic authors include functional flatulence, functional constipation, and functional diarrhea in the same group. IBS is a functional intestinal disorder manifested by abdominal pain and/or defecation disorders and/or flatulence. IBS is one of the very common diseases in gastroenterological practice: 40–70% of patients visiting a gastroenterologist have IBS. It can manifest itself at any age, incl. in children. The ratio of girls to boys is 2–4:1.
The following are symptoms that can help diagnose IBS:
(Rome, 1999):
- Stool frequency less than 3 times a week;
- Stool frequency more than 3 times a day;
- Hard or bean-shaped stool;
- Loose or watery stool;
- Straining during the act of defecation;
- Urgent urge to defecate (inability to delay bowel movement);
- Feeling of incomplete bowel movement;
- Discharge of mucus during bowel movements;
- Feeling of fullness, bloating, or transfusion in the abdomen.
The pain syndrome is characterized by a variety of manifestations: from diffuse dull pain to acute, spasmodic pain;
from constant to paroxysmal abdominal pain. The duration of pain episodes ranges from several minutes to several hours. In addition to the main “diagnostic” criteria, the patient may experience the following symptoms: increased urination, dysuria, nocturia, dysmenorrhea, fatigue, headache, back pain. Changes in the mental sphere in the form of anxiety and depressive disorders occur in 40–70% of patients with irritable bowel syndrome. In 1999, diagnostic criteria for irritable bowel syndrome were developed in Rome. This is the presence of abdominal discomfort or pain for 12 non-consecutive weeks in the last 12 months, combined with two of the following three symptoms:
- Stopped after defecation and/or
- Associated with changes in stool frequency and/or
- Associated with changes in the shape of feces.
IBS is a diagnosis of exclusion, but for a complete diagnosis the patient needs to undergo a lot of invasive studies (colonoscopy, cholecystography, pyelography, etc.), so it is very important to carefully collect the patient’s history, identify symptoms and then carry out the necessary studies.
Functional abdominal pain
This diagnosis occupies a different place in different classifications. According to DA Drossman, functional abdominal pain (FAP) is an independent variant of GIT FN. Some doctors consider FAB as part of an ulcer-like type of functional dyspepsia or as a variant of IBS. According to the classification developed by the Committee for the Study of Functional Disorders in Children, FAD is considered a disorder characterized by abdominal pain, along with functional dyspepsia, irritable bowel syndrome, abdominal migraine, and aerophagia.
This disease is very common. Thus, according to HG Reim et al., in children with abdominal pain in 90% of cases there is no organic disease. Transient episodes of abdominal pain occur in children in 12% of cases. Of these, only 10% manage to find an organic basis for these abdominalgia.
The clinical picture is dominated by complaints of abdominal pain, which is most often localized in the umbilical region, but can also be observed in other regions of the abdomen. The intensity, nature of pain, and frequency of attacks are very variable. Associated symptoms are loss of appetite, nausea, vomiting, diarrhea, headaches; Constipation is rare. These patients, just like patients with IBS, experience increased anxiety and psycho-emotional disturbances. From the entire clinical picture, characteristic symptoms can be identified, based on which a diagnosis of FAB can be made:
- frequently recurring or continuous abdominal pain for at least 6 months;
- partial or complete lack of association between pain and physiological events (ie, eating, defecation, or menstruation);
- some loss of daily activities;
- absence of organic causes of pain and insufficiency of signs for the diagnosis of other functional gastroenterological diseases.
In terms of diagnosis, it should be noted that this, like other gastrointestinal FN, FAB, is a diagnosis of exclusion, and it is very important to exclude not only other pathologies of the patient’s digestive system, but also pathologies of the genitourinary and cardiovascular systems.
In children of the first year of life, a diagnosis of functional abdominal pain is not made, and a condition with similar symptoms is called infantile colic
, i.e. an unpleasant, often discomforting feeling of fullness or compression in the abdominal cavity in children of the first year of life.
Clinically, infantile colic occurs as in adults - abdominal pain of a spastic nature, but unlike in adults, in a child this is expressed by prolonged crying, restlessness, and wiggling of the legs.
Abdominal migraine
Abdominal pain with abdominal migraine most often occurs in children and young people, but is often detected in adults. The pain is intense, diffuse, but sometimes can be localized in the navel area, accompanied by nausea, vomiting, diarrhea, paleness and coldness of the extremities. Autonomic accompanying manifestations can vary from mild, moderately pronounced to severe vegetative crises. The duration of pain ranges from half an hour to several hours or even several days. Various combinations with migraine cephalgia are possible: the simultaneous appearance of abdominal and cephalgic pain, their alternation, the dominance of one of the forms with their simultaneous presence. When diagnosing, it is necessary to take into account the following factors: the relationship of abdominal pain with a migraine headache, provoking and accompanying factors characteristic of migraine, young age, family history, the therapeutic effect of anti-migraine drugs, an increase in the speed of linear blood flow in the abdominal aorta during Doppler ultrasound (especially during paroxysm) .
Functional stool retention and functional constipation
Constipation is caused by disruption of the processes of formation and movement of feces throughout the intestine. Constipation is a chronic delay in bowel movement for more than 36 hours, accompanied by difficulty in defecation, a feeling of incomplete evacuation, and the passage of a small (<100 g) amount of high-density feces. In the absence of the listed criteria for constipation and irregular bowel movements, we can talk about functional stool retention.
One of the most common causes of constipation is dysfunction and uncoordinated work of the muscular structures of the pelvic floor and rectum.
. In these cases, there is no or incomplete relaxation of the posterior or anterior levators and puborectal muscles. Constipation is caused by intestinal motility disorders, most often increased non-propulsive and segmenting movements and a decrease in propulsive activity with increased sphincter tone - “drying out” of the feces, discrepancy between the capacity of the large intestine and the volume of intestinal contents. The occurrence of changes in the structure of the intestines and nearby organs can interfere with the normal movement of feces. Functional constipation can also be caused by suppression of the defecation reflex, which is observed in shy children (conditioned reflex constipation). They most often occur when the child begins attending preschool institutions, with the development of anal fissures and when the act of defecation is accompanied by a pain syndrome - “fear of the potty.” Constipation can also occur when getting out of bed late, morning rush, studying in different shifts, poor sanitary conditions, and a feeling of false shame. In neuropathic children with prolonged stool retention, defecation is a pleasure. Diagnosis of constipation is based on the analysis of clinical and anamnestic data, morpho-functional, instrumental and laboratory research methods.
Treatment
In the treatment of all of the above conditions, an important role is played by the normalization of the diet, a protective psycho-emotional regime, and explanatory conversations with the patient and his parents. The appropriate choice of medications is the main task of a gastroenterologist for functional bowel diseases.
Despite the variety of pathological processes presented in the article, one can note the similarity of the clinical picture of all these diseases, pathogenetic and etiological processes.
One of the leading pathological mechanisms in functional bowel diseases is excessive contraction of the smooth muscles of the intestinal wall and associated abdominal pain.
. Therefore, in the treatment of these conditions, it is rational to use drugs with antispasmodic activity.
Numerous clinical studies have proven the effectiveness and good tolerability of myotropic antispasmodics in functional bowel diseases. However, this pharmacological group is heterogeneous, and when choosing a drug, the mechanism of its action should be taken into account, since abdominal pain is very often combined with other clinical symptoms, primarily flatulence, constipation and diarrhea.
The active ingredient of the drug Duspatalin
is mebeverine hydrochloride, a methoxybenzamine derivative. A feature of the drug Duspatalin is that smooth muscle contractions are not completely suppressed by mebeverine, which indicates the preservation of normal peristalsis after suppression of hypermotility. Indeed, there is no known dose of mebeverine that completely inhibits peristaltic movements, i.e. would cause hypotension. Experimental studies show that mebeverine has two effects. First, the drug has an antispastic effect, reducing the permeability of smooth muscle cells to Na+. Secondly, it indirectly reduces the outflow of K+ and, accordingly, does not cause hypotension.
The main clinical advantage of the drug Duspatalin is that it is indicated for patients with irritable bowel syndrome and abdominal pain of functional origin, which is accompanied by both constipation and diarrhea, since the drug has a normalizing effect on intestinal function.
| Dosage | Patient age |
| 25 mg | 3 years |
| 50 mg | 4–8 years |
| 100 mg | 9–10 years |
| 150 mg | over 10 years old |
If necessary, antidiarrheal and laxative drugs are included in the treatment of functional intestinal disorders, but in all cases these drugs cannot be used as monotherapy.
The role of Helicobacter pylori (HP) in the pathogenesis of chronic abdominal pain is debated. Studies have shown that HP infection does not play a significant role, but some authors provide data on some reduction in pain intensity after HP eradication. It is recommended to examine patients with abdominal pain only if structural changes in the organs are suspected.
The use of prokinetics in the treatment of functional disorders occurs, but their effectiveness is not very high, and they cannot be used as monotherapy.
Considering that in almost all of the above diseases, the psycho-emotional status of the patient plays an important role, it is necessary, after consulting a neuropsychiatrist, to resolve the issue of prescribing psychotopic drugs (antidepressants).
Literature:
1. Pediatric gastroeterology. Manual on CD. Under the general editorship of S.V. Belmera and A.I. Khavkina. Moscow, 2001, 692 MB.
2. Vein A.M., Danilova A.B. Cardialgia and abdominalgia of breast cancer, Volume 7 No. 9, 1999.
3. Autonomic disorders. Clinic, diagnosis, treatment. Edited by A.M. Veina. Moscow, 1998
4. Ryss E.S. Modern ideas about IBS. Gastrobulletin No. 1 2001
5. IBS. Practical guide for doctors. Moscow1999.
6. Functional diseases of the intestines and biliary tract: issues of classification and therapy. International Bulletin: Gastroenterology, 2001, No. 5
7. Drossman DA The Functional Gastrointestinal Disorders. Diagnosis, Pathophysiology, and treatment. A Multinational Consensus. Little, brown and Company. Boston/ New York/ Toronto/ London. 1994. 370 p.
8. Drossman DA, Whitehead WE, Toner BB, Diamant N, Hu YJ, Bangdiwala SI, Jia H. What determines severity among patients with painful functional bowel disorders? Am J Gastroenterol. 2000 Apr;95(4):862–3
9. Farfan Flores G, Sanchez G, Tello R, Villanueva G. Estudio clinico y etiologico de 90 casos de diarrea cronica.// Rev.Gastroenterol.Peru – 1993.– Vol.13.– N1.– P.28–36 .
10. Forbes D. Abdominal pain in childhood. Aust Fam Physician 1994 Mar;23(3):347–8, 351, 354–7.
11. Gorard DA, JEGomborone, GWLibby, MJGFarthing. GUT 39:551–555. 1996
12. Gottrand F. The role of Helicobacter pylori in abdominal pain in children. Arch Pediatr 2000 Feb;7(2):197–200
13. H.G.Reimm, M.Koken. Functional abdominal pain in childhood. Medical treatment with mebeverine (DuspatalR suspension).
14. Scott RB. Recurrent abdominal pain during childhood.// Can.Fam.Physician.– 1994.– Vol.40.– P.539–547.
15. Schmulson MW, Chang L. Diagnostic approach to the patient with irritable bowel syndrome. Am J Med 1999 Nov 8;107(5A):20S–26S
16. Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller–Lissner SA. Functional bowel disorders and functional abdominal pain. Gut 1999 Sep;45 Suppl 2:II43–7.
Diagnostics
In most cases, an experienced doctor will be able to make a diagnosis during the initial examination. However, there are additional research methods that can assess the severity of the disease and help in the correct choice of a particular treatment method.
Studies that may be required to determine the severity of rectal prolapse:
- Anal electromyography. This test determines whether nerve damage is causing the anal sphincters to not work properly. It also covers coordination of the rectum and anal muscles.
- Anal manometry. This test examines the strength of the anal sphincter muscles. The study allows you to evaluate the holding function.
- Transrectal ultrasound examination. This test helps evaluate the shape and structure of the anal sphincter muscles and surrounding tissues.
- Proctography (defecography). This test evaluates how well the rectum holds stool and how well the rectum empties.
- Colonoscopy. Allows you to visually examine the entire colon and helps identify certain problems.
Our Clinic has all the necessary diagnostic services. We also work closely with urologists and gynecologists from other departments of Sechenov University, which allows us to approach the issue of treating rectal prolapse multidisciplinary, that is, jointly.
Treatment of rectal prolapse
Our Clinic provides the full range of treatment for rectal prolapse. Based on the stage of the disease and its manifestations, our specialists select the most optimal treatment method. It is important to understand that rectal prolapse is a complex disease that cannot be treated without surgery. To treat rectal prolapse, our Clinic uses the following surgical techniques:
Abdominal surgeries (surgeries through the abdominal cavity)
1. Operation rectosacropexy - it uses a mesh allograft (alloprosthesis), which holds the intestine in a given position. During the operation, the rectum is mobilized to the level of the levator ani muscles, then the rectum is pulled up and fixed to the presacral fascia, located between the sacrum and the rectum, using a mesh allograft.
2. Kümmel’s operation is the fixation of the previously mobilized rectum to the promontory of the sacrum with interrupted sutures.
These operations can be performed either openly through incisions (laparotomy) or laparoscopically through small punctures.
Transanal operations (operations through the anal canal)
1. Delorme's operation is the removal (resection) of the mucous membrane of a prolapsed section of the intestine with the formation of a muscular cuff that holds the intestine, protecting it from prolapse.
2. Altmeer's operation - resection of the rectum or its prolapsed section with the formation of a coloanal anastomosis - joining the colon to the anal canal.
Surgical treatment in most cases allows patients to completely get rid of the symptoms of rectal prolapse. The success of treatment depends on the type of prolapse - internal or external, on the general condition of the patient and on the degree of neglect of the disease. Patients may need some time to regain gastrointestinal function. After surgery, it is important to control bowel movements, avoid constipation and severe straining.
What should parents do if they have prolapse?
When identifying a prolapsed section of intestine, parents should not panic. This will quickly affect the baby, cause crying and worsen the situation. To regular care, you should add mandatory washing with chamomile decoction. Then calmly try to straighten the intestine.
To do this you need to follow the rules:
- wipe the baby's perineum with blotting movements;
- lay the baby on his back;
- lifting the pelvis, spread the legs outward;
- lubricate the fallen knot with Vaseline;
- lightly press the formation with your thumb until it enters the lumen of the anus;
- turn the baby onto his stomach;
- squeeze the buttocks with your hand or a diaper for half an hour;
- maintain bed rest.
If the procedure had to be performed for the first time, for an infant you need to call a doctor home; older children must be shown to a specialist in the near future.