If a person says: “I have abdominal pain,” then it is important to understand: behind abdominal pain there may be problems with any organs of the abdominal cavity, retroperitoneal space, or small pelvis.
If a person says: “I have abdominal pain,” then it is important to understand: behind abdominal pain there may be problems with any organs of the abdominal cavity, retroperitoneal space, or small pelvis. The intestines (ileum, jejunum, colon, sigmoid, colon, transverse colon), appendix, stomach, liver, duodenum, spleen, ureters, kidneys, mesenteric (mesenteric) vessels of the intestine can cause painful sensations in the abdomen. Therefore, pathologies can be gastroenterological, surgical, gynecological, or urological in nature.
Types of pain
Abdominal pain can be very different:
- Acute and chronic . Acute pain occurs suddenly, chronic pain develops gradually, its intensity increases step by step - sometimes over several weeks. In this case, a special type is formed by chronically recurrent abdominal pain. They can suddenly make themselves felt, and then also suddenly pass and resume after a certain period of time.
- Tonic and clonic . With tonic pain, the muscles are very tense, compacted areas appear on the abdomen, and uncontrolled muscle contraction is observed. Tonic pain is accompanied by fairly rhythmic spastic spasms.
- Burning (cutting) and aching – reminiscent of hunger.
The localization of pain can be the abdominal cavity, hypochondrium, areas above or below them.
Consequences of not following the diet
With spontaneous refusal of therapeutic nutrition, especially at the acute stage of the disease,
:
- pain symptoms, spasms;
- nausea, vomiting;
- diarrhea, to dehydration;
- bile flow disorders, hepatic colic;
- intoxication of the body due to intestinal infections, hepatitis C.
Errors in diet cause relapse of chronic gastrointestinal pathology.
Symptoms
A person who complains of abdominal pain may have different symptoms. Most often it manifests itself in the form of spasms and colic.
- Colic is an attack of primarily stabbing (hence the name) pain. In case of colitis, a person has colitis in both sides, in case of appendicitis or inflammation of the ovaries - in the lower abdomen, in case of poisoning, the localization of colic can be in different parts of the abdomen and most often an additional symptom appears (vomiting, diarrhea).
- Spasms are pain that is accompanied by involuntary muscle contraction. At the same time, the skin turns pale. The pain may cause the person to lose consciousness. If the spasms are due to inflammatory diseases of the intestines or stomach, they are accompanied by fever. Gynecological problems are indicated by spasms accompanied by bleeding.
- Anginal pain is an unpleasant sensation with a strong burning sensation.
- Sharp pain in the area above the navel is a common occurrence with appendicitis.
- A feeling of “fullness” in the lower back may indicate problems with the colon
- Cyclic pain (either intensifies or subsides) is a characteristic symptom of diseases of the bladder and intestines.
- Pain accompanied by severe gas formation indicates improper functioning of the colon.
- Painful sensations accompanied by itching of the anus are symptoms of damage to the rectum.
- Unpleasant sensations in the abdomen , intensifying at rest and disappearing with movement, are the result of problems with blood circulation.
Types of diets for various gastrointestinal diseases
Another interesting and working type of diet: the FODMAP diet, which is used for complaints of severe flatulence, abdominal pain, alternating diarrhea and loose stools - all manifestations of IBS (irritable bowel syndrome), as well as inflammatory bowel diseases.
The essence of the diet is to exclude carbohydrate groups that contain large amounts of fructose, lactose, fructans, galactans and sugar alcohol polyols. These carbohydrates are poorly absorbed in the intestines and promote the growth of bacterial and fungal flora, which leads to symptoms such as bloating, gas formation, pain and discomfort in the gastrointestinal tract.
We recommend
“Foods good for the kidneys: TOP-25 for good health” Read more
FODMAPs are found in a wide range of foods, and most people eat high FODMAP foods every day without problems. When FODMAPs are eaten, they move slowly through the small intestine, attracting water. When they reach the colon, gut bacteria use FODMAPs as a fuel source for survival. Bacteria quickly ferment FODMAPs, resulting in gas production.
Below are food groups that contain FODMAP substances. Oligosaccharides (fructans and galactooligosaccharides) are found in foods such as wheat, rye, onions, garlic and legumes. Disaccharides (lactose) - found in dairy products such as milk, soft cheeses, yoghurts. Monosaccharides (fructose) - found in honey, apples, corn syrups, etc. Polyols (sorbitol and mannitol) are found in some fruits and vegetables and are used as artificial sweeteners.
The FODMAP diet allows
:
- Reduce pain and discomfort.
- Reduce bloating and distension.
- Improve bowel function (reduce diarrhea or constipation).
- Improve quality of life.
The diet shows its effectiveness in eliminating the symptoms of diarrhea, bloating, and abdominal pain. Of course, strict adherence to all restrictions is required, but if they are followed correctly, many people feel improvement within the first week of the diet.
Study
: A diet low in FODMAPs reduces symptoms of irritable bowel syndrome
In addition to diet, it is also important to reduce the overall level of stress, increase the digestive capabilities of the gastrointestinal tract, and use nutritional supplements and medications if necessary.
Study
FODMAPs and Irritable Bowel Syndrome
List of permitted/prohibited products
| Allowed | Prohibited | |
| Fruits | Berries except blackberries and currants. Maximum 1 fruit (serving) per day: banana (mini or unripe), melon, clementine, grapes, ripe guava, kiwi (golden, green), lemon, lime, orange, passion fruit, pineapple, raspberry, rhubarb. | Apples, mangoes, dates, figs, pears, dried fruits, guava, papaya, watermelons, cherries, ripe bananas, persimmons, plums, prunes, peaches, nectarines, lychees, blackberries, currants, avocados (2-3 slices per day are allowed). |
| Vegetables | Arugula, bok choy, bean sprouts, cross salad, pickled or pickled beets, bell peppers, celery, cucumbers, eggplant, green beans, ginger root, cabbage (no more than half a cup per day), Chinese cabbage, lettuce, parsnips, spinach , chard, zucchini, seaweed, tomatoes, zucchini, turnips, radishes, olives, oyster mushrooms, dill, parsley. Limited starchy vegetables (no more than half a serving, for example, half a small potato per day): potatoes, pumpkin, squash, carrots. | Beets, broccoli, fennel, garlic, onions, shallots, Jerusalem artichokes, asparagus, artichoke, sweet green peas, sun-dried tomatoes, cauliflower, cabbage, mushrooms, corn. |
| Animal proteins | Organic (bio) meat chicken, turkey, lamb, duck, beef, pork. | Meat from farmed animals, sausages, sausages, canned meat. |
| Fish | Wild salmon, cod, trout, anchovies, herring, sardines, mackerel, low mercury wild fish. | Factory fish, fish with high mercury content, including tuna, shark, swordfish. |
| Cereals | Gluten-free grains including quinoa, rice, buckwheat, millet, amaranth, brown rice pasta, buckwheat noodles, and gluten-free oats. | Gluten-containing grains including wheat, barley, rye, spelled, bran, flour, couscous, oats not labeled as gluten-free. |
| Beans and legumes | All legumes (peas, beans, lentils, chickpeas). | |
| Nuts and seeds | All nuts and seeds except those prohibited. | Peanuts (classified as legumes), pistachios, cashews. |
| Dairy | Hemp, almond, rice or coconut milk. Cheeses with low lactose content: brie, camembert, cheddar, mozzarella, parmesan, pecorino, Swiss (hard cheeses). Butter. Lactose-free dairy products. | Cow, goat, sheep, soy milk, soft cheeses (ricotta, cream, Adyghe, etc.), cream, cottage cheese, yogurt, fermented baked milk, yogurt, powdered milk. |
| Sweeteners | Small amounts of stevia, 100% maple syrup, 100% date sugar, molasses (blackstrap molasses), sugar (refined sugar, brown sugar, cane sugar), vanilla extract. | Sweeteners (sorbitol, mannitol, isomaltose, maltitop, xylitol), concentrated fruit juices, high fructose corn syrup. |
| Beverages | Green and herbal teas, mineral water, filtered water, limited coffee. | Commercial fruit juices, energy drinks, alcohol, sodas. Chicory and dandelion tea. |
| Oils | Unrefined cold-pressed oils: olive, coconut, flaxseed. Butter, ghee. | Refined oils, margarine, salad dressings. |
The transition to a low FODMAP diet usually occurs in several stages
.
Stage 1
. Exclusion of prohibited products. The exclusion period for prohibited foods is usually 3-6 weeks.
Stage 2
. Elimination. The duration of the low FODMAP diet is usually 2 to 6 weeks or until symptoms improve. If you have SIBO (bacterial overgrowth syndrome), diet alone is not enough to reduce pathogenic or opportunistic flora.
Stage 3
. Diet expansion. In order to establish a response to a specific FODMAP carbohydrate, it is advisable to first expand the diet to foods containing only one of the listed carbohydrates. For example, start with dairy products to eliminate lactose intolerance. Then - with honey (a source of fructose). Mannitol is found in mushrooms, and sorbitol is found in fresh avocado and peach. Fructans, other than some fruits (melon, etc.), are the only FODMAP carbohydrate in fresh onions, red onions and garlic. Galactans are present in significant quantities in almonds. It takes 3 days to introduce one product.
We recommend
“Proper diet: menu planning and ready-made recipes” Read more
On the first day, a small portion of the product is consumed. It is usually recommended to start with half a serving (for example, 100 ml of yogurt). If symptoms appear after consuming even a small amount of this product, this may indicate lactose intolerance. You should try another product with the same carbohydrate after 3 days. If there are no symptoms when consuming a small portion, you should continue to assess the tolerability of a regular portion of the product on the 2nd day.
The next day you can use a standard portion of the product. If unpleasant symptoms and sensations appear, the test is not carried out on the third day, but a break is taken for another three days. If all is well, on the third day you can consume a larger portion of the product. The presence of symptoms will indicate that such large quantities should not be consumed. If there are no symptoms after three days, the tolerability of other products from the same group should be assessed. Each new product is evaluated according to the above scheme (day 1-2-3). There should be 3 days between tests with two different products in order to completely eliminate the influence of the previous test on the subsequent one.
After analyzing the tolerance of various products within one group (for example, the group of milk and fermented milk products), you can move on to assessing other carbohydrates. Try a fructose tolerance test with honey and mango. The next food group to evaluate is, for example, lentils, hazelnuts and almonds (containing only galactans). Pomegranate, grapefruit, melon and some other fruits, garlic and onions will help assess your fructan tolerance. Sorbitol is found in peach, apricot, avocado, and blackberry. Mannitol is found in large quantities in mushrooms (champignons, porcini mushrooms), as well as in cauliflower.
Causes
What are the causes of abdominal pain, dysfunction of the abdominal organs and retroperitoneal space?
The cause of colic can be appendicitis, inflammation of the ovaries (in these cases, colic in the lower abdomen), poisoning, or colitis. With colitis, a person has colitis in both sides. If the colic is cramping and is localized both in the abdomen and in the lower back, the pain is more intense, the cause is most often urolithiasis, kidney injuries or pyelonephritis. Colic in the navel area may be a response to irritants of the sensitive mesenteric plexus of the intestine.
Among the common causes of paroxysmal spasms are intestinal obstruction and gastroduodenitis. And uterine endometriosis is most often behind spasms during urination in women.
If abdominal pain is accompanied by increased gas formation and a frequent urge to defecate, then the cause will most often be associated with diseases of the colon.
If you have abdominal pain - anginal, and the patient is bothered by an expressive burning sensation - the cause is most often gastritis (inflammation of the stomach lining) or pancreatitis (inflammation of the pancreas). If pain and burning are accompanied by severe tension in the muscles of the abdominal wall, and a person complains of pressure in the chest, the cause may be associated with heart pathologies: in particular, such pain is typical for 60% of patients with myocardial infarction.
The cause of abdominal pain accompanied by low-grade fever (the temperature remains at 37.1–37.5 °C for a long time) is most often inflammatory bowel disease.
Objectives and principles of nutrition for a sick intestine
Diseases of the gastrointestinal tract occur due to poor nutrition.
Scientists have found that the occurrence of most diseases of the gastrointestinal tract is associated with regular violations of the diet.
Therefore, it is important to adhere to certain norms and rules of nutrition that will help restore the intestines to their previous functions.
Diseases
Most often, abdominal pain is caused by diseases of the intestines, stomach, pancreas, problems with the gallbladder, as well as hernias.
Intestinal diseases
- Ulcerative colitis is a diffuse inflammation. The rectal mucosa is affected. In the initial forms of ulcerative colitis, inflammation affects only the proximal part (the entrance to the intestine); in advanced forms, the problems affect the entire colon. As the disease progresses and worsens, the patient feels a sharp deterioration in health, the body begins to become intoxicated, the pulse quickens, and in most cases blood appears in the stool. If the disease is not treated, the body can poison itself, and peritonitis can develop - damage to the abdominal cavity that poses a threat to life.
- Enteritis . The small intestine becomes inflamed. At first, the disease is “masked” as a disease, and often accompanies this problem. If the disease is not treated in a timely manner, the functions of the small intestine are disrupted. Food begins to be poorly absorbed by the intestinal walls. Digestion processes are disrupted.
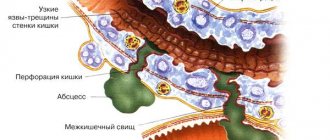
- Crohn's disease . One or several areas of the intestine can become inflamed. But almost always the inflammation affects the junction of the large and small intestines. One of the most unpleasant aspects is that the inflammation affects the entire thickness of the wall, and a complication of the disease is intestinal obstruction syndrome, the treatment of which requires the adoption of a set of measures related to the simulation of motility and restoration of intestinal function.
- Dysbacteriosis is a disorder of the intestinal microflora. The number of beneficial bacteria in the intestines is reduced, and pathogenic microflora develops. As a result, gas formation occurs, a person cannot digest food, and bowel movements are disrupted. Very often, the development of dysbiosis is a consequence of incorrect antibiotic therapy or a reaction to stress.
Pancreatic diseases
- Pancreatitis . The most common disease affecting the pancreas is pancreatitis. When the pancreas is inflamed, a person feels severe discomfort in the upper abdomen, and it becomes difficult for the body to digest proteins and fats. Often in everyday life they say in this case: “There are not enough enzymes.” And this really reflects the real picture. In the affected pancreas, the production of lipase, chymotrypsin, and trypsin is significantly reduced.
- Cystic fibrosis is a disease that disrupts the functioning of the pancreas and respiratory system. It is a non-inflammatory pathology. The reason is hereditary factors. A complication of the disease may be the formation of a duodenal ulcer.
Stomach diseases
Some of the most common diseases that affect people of all ages are accompanied by abdominal pain - these are pathologies of the stomach, especially its mucous membrane. The leaders are gastritis, ulcers, gastroesophageal reflux disease.
- Gastritis . It is an inflammation of the gastric mucosa. The entire stomach or certain parts of it can become inflamed. With gastritis, pain with burning and spasms predominate. The patient is concerned about discomfort after eating, a feeling of a full stomach or, on the contrary, “sucking” and a constant feeling of hunger. Accompanying the disease in the acute stage are vomiting and nausea.
- Stomach ulcer . Pain occurs against the background of characteristic ulcerative damage to the gastric mucosa. Dyspeptic symptoms are pronounced: heaviness in the stomach, a feeling of oversaturation of the stomach, pain in the epigastric region.
- Gastroesophageal reflux disease (popularly known as “reflux”). The disease is associated with a weakening of the valve between the stomach and esophagus. The result of this weakening is pain, accompanied by heartburn. Very often, gastroesophageal reflux disease appears in patients who have already experienced gastritis or a stomach ulcer.
Bibliography:
- Alexander KC Acute Abdominal Pain in Children – 2003.
- Fitzgerald M., Mcntosh N., Pain and analgesia in the newborn. — Arch.Dis.Child.,1989
- Drossman DA The functional gastrointestinal disoders and the Rome III process – 2006.
- Novikova V.P. Functional diseases of the gastrointestinal tract in young children - 2016.
- Pediatric gastroenterology and nutritionology. - 2005. - T. 13. - No. 18.
- Abdominal pain syndrome in children. Ivanovo - 2009.
- Ashcraft K.W., Holder T.M. Pediatric surgery. Practical guide in 3 volumes. 1996-1997.
- Pediatric surgery. National leadership - 2009.
- Filimonov R.M. Adolescent gastroenterology - 2008.
- Keshishyan E.S. Intestinal colic and correction of microbial colonization in children in the first months of life // information for doctors. – 2006.
- Sologub E.A., Karaseva O.V., Timofeeva A.G. Nonspecific mesadenitis in children (literature review). Pediatric pharmacology. 2013.
- Chadwick V.S., Phillips S.F. Gastroenterology 2. Small intestine - 1985.
- Petrenko V.M. Lymphatic system: anatomy and development. Basic research. 2010.
Published on the portal baby.ru
Hernias
Often abdominal pain is caused by peritoneal hernias. They can be umbilical, inguinal, diaphragmatic. Umbilical hernias are more often formed during pregnancy or in the postpartum period, inguinal hernias - with excessive stress, diaphragmatic hernias - defects of the abdominal wall that form as a reaction to improper bowel function, an incorrectly selected corset, or heavy lifting. The insidiousness of diaphragmatic hernias is that at the initial stage of the disease, a person believes that he has typical gastritis - with heartburn and belching, but traditional therapy does not provide treatment, and ultrasound shows that the cause is not inflammation of the stomach, but precisely the presence of a hernia. In toga, to combat pathology, it is not necessary to relieve inflammation or eliminate spasms, but to undergo surgical treatment, which is aimed at strengthening the abdominal wall.
Diseases of the gallbladder and bile ducts
A special group consists of diseases associated with the gallbladder and bile duct.
- Cholangitis . Inflammation of the bile ducts. The pain is unbearable. Mainly on the right side. It is complicated by the fact that it requires not only quick relief from the attack of pain itself, but also normalization of blood pressure.
- Cholecystitis . Acute pain due to eating fatty foods. Often the pain itself is followed by vomiting mixed with bile. Flatulence (gas formation) and vomiting may occur.
- Gallstone disease is the formation of hard structures – stones – in the bile. Pain in the disease is paroxysmal. Especially if the stones move through the gallbladder and ducts.
How can you help?
If there is no stool during the day or insufficient emptying, it is necessary to force a bowel movement in the child.
It is possible to use a microenema or a glycerin suppository. Self-administering a water enema to a child is not recommended due to complications that can arise from a number of surgical diseases. If you refuse to eat, and especially if you are vomiting, do not try to force-feed your child. It is enough to provide him with a drinking regime to normalize the water balance. Self-prescription of pro- and prebiotics, antibacterial and painkillers is unacceptable. The latter can “blur” the picture and make it difficult to diagnose surgical pathology when visiting a doctor.
The use of enterosorbents is permissible; drugs based on simethicone, eliminating gas formation and bloating; drugs that relax the intestinal muscles - antispasmodics. Medicines must be used in accordance with the official instructions.
It should be noted that in children, abdominal pain syndrome in acute surgical pathology may not be as pronounced as in adults. And besides, it does not always have a clear localization even in acute appendicitis, and develops gradually. Therefore, if there is no positive dynamics from your actions within 2 hours, consult a doctor immediately.
Contraindications
An incorrect diagnosis can lead to the fact that treatment will not only be useless, but will provoke serious complications. After all, many medications and physiotherapeutic techniques that are effective for some diseases accompanied by abdominal pain are strict contraindications for other diseases with similar symptoms.
For example, if a number of medications prescribed for pancreatitis are given to patients with hepatic colic, the reaction may be unpredictable. And treating a number of stomach diseases with antibiotics can cause serious dysbiosis.
And absolute contraindications for pain in the abdomen or stomach are self-medication - especially independent decision-making to take a painkiller or antispasmodic. If, for example, such drugs are used by a person whose appendix is inflamed, relief will follow for a while. But this will not be help, but false help to yourself. There are often cases when patients who did not get to the surgeon in a timely manner to remove appendicitis began to experience necrosis of the tissues of neighboring organs.
Under no circumstances should you resort to even seemingly “harmless” means to combat high acidity without making a diagnosis. What seems to be simply a release of excess hydrochloric acid and inflammation of the stomach may turn out to be a symptom of a completely different disease, such as a heart attack.
Also, for abdominal pain with an unclear diagnosis, you should not apply a heating pad with hot water. In a number of pathologies, heat only accelerates the inflammatory process and activates bleeding.
Surveys
An effective examination of a patient who is bothered by abdominal pain consists of an interview, palpation of the abdomen, and laboratory and functional diagnostics.
For a doctor to make a diagnosis, the smallest details are important. For example, even a basic assessment of stool can clarify a lot in the case of abdominal pain.
- Hard lumps (“sheep” feces) are a frequent companion to colitis, elongation of the sigmoid colon, and gastric ulcers.
- Watery stools often accompany poisoning and infectious diseases.
- With a parasitic disease (presence of worms in the intestines), dysbacteriosis, stool particles are usually very loose.
Also, to select a tool and diagnostic technology, an oral interview with the patient is important. The doctor asks the patient how long the pain lasts, whether there are attacks, what exactly causes the pain - physical movements, going to the toilet, eating, taking a certain position.
Symptomatic manifestations of the disease
Symptoms of colic in the intestines depend on the primary disease: pain can be localized in certain areas of the body or spread over the entire surface of the abdominal wall.
The condition lasts up to 3 days and is fraught with the gradual development of narrowing of the intestinal lumen (due to accumulated feces), which leads to primary spasms. Symptomatically, intestinal colic manifests itself:
- attacks of acute pain combined with spasms - manifestations increase and last from several hours to a couple of days;
- dyspeptic symptoms - belching, nausea, vomiting, bloating;
- diarrhea with mucus;
- weakness, deterioration of general condition;
- aversion to food;
- intestinal obstruction - excruciating pain, decreased blood pressure, cold sweat, pallor.
At the first signs of intestinal obstruction, you must call an ambulance.
Abdominal colic in adults, caused by intestinal obstruction, is life-threatening for the patient. If the disease is advanced, surgical intervention will be required.
[media=
https://youtu.be/ZmD3rM-4PQk
]
Diagnostics
The following types of research are especially valuable for identifying the cause of the disease and finding treatment methods for pathologies of the abdominal cavity:
- Ultrasound of the abdominal cavity. One of the most prompt measures in diagnosing diseases of the abdominal and pelvic organs and identifying the cause of abdominal pain is ultrasound diagnostics. Using ultrasound, you can identify pathologies of the liver, gall bladder, spleen, kidneys, uterus, and ovaries. Many people wonder whether the stomach and intestines are visible on an ultrasound. The stomach cannot be examined using ultrasound; the intestines cannot be examined partially. If the equipment has good resolution, for example, volumetric formations in this area are visible.
- FGDS (gastroscopy, probing, intestinal swallowing) is a diagnostic method that can be used to obtain an objective picture of the condition of the stomach, duodenum, and esophagus. If necessary, you can immediately conduct a rapid test for Helicobacter pylori (the cause of the development of ulcers), do cytology and biopsy to exclude the oncological nature of the disease, and determine “acidity”.
- X-ray. An old, but still practiced method of diagnosis. It can be used as an emergency measure to examine the stomach if for some reason an FGDS cannot be done. In addition, x-rays are informative in identifying diseases accompanied by symptoms of intestinal obstruction. Depending on the nature of the patient’s pain and complaints, traditional X-rays or contrast-enhanced X-rays (irrigoscopy) may be used.
- MRI is a progressive diagnostic method for abdominal injuries, liver enlargement, and an uninformative picture of the abdominal cavity on ultrasound (for example, due to severe flatulence).
- Colonoscopy. One of the most accurate methods for examining the intestines. This is done using a fiber colonoscope. Using the device, you can examine everything - even the most complex areas, including the inner surface of the colon.
- Cholescintigraphy . Isotopic study. It is carried out using a radiopharmacological drug. Informative for problems with the gallbladder and bile ducts.
- Blood, urine and canal analysis . In the blood test, special emphasis is placed on ESR (inflammation can be determined by the erythrocyte sedimentation rate), biochemical indicators, and in many types of examinations for abdominal pain, stool is examined for occult blood.
What to do?
So, the main thing for abdominal pain is not to self-medicate, and not to delay visiting a doctor and getting a diagnosis.
At the same time, in some cases, it is important not just to make an appointment at the clinic, but to immediately call an ambulance. In what cases is an ambulance required?
- Abdominal pain is very intense.
- Cold sweat appears.
- Severe vomiting of blood begins.
If the pain is not acute, there is no blood in the vomit, the temperature differs from that of a healthy person, but there is no fever, consultation with a therapist, gastroenterologist and diagnosis are recommended.
Timely diagnosis is a guarantee that the most gentle methods will be used to combat the disease. Even if we are talking about surgery.
- Laparoscopy is used to remove gallstones and appendicitis (if the situation is not advanced).
- Laparoscopic funduplication is used to treat gastroesophageal reflux disease.
- To effectively solve problems with hernias and strengthen the abdominal wall, surgical hernioplasty is used.
If there are no indications for surgical treatment, the therapeutic effect for many diseases of the intestines and stomach is provided by an integrated approach, which is based on diet therapy, physiotherapy and drug therapy - antibiotics, antiparasitic drugs, corticosteroids, prokinetics to improve intestinal motility.
How can a parent help?
If the child has not passed gas or stool for a long time, and his stomach is tense, give him a gas tube.
If the child's condition does not improve or there is no passing of gas or stool, consult a doctor. In case of prolonged attacks of colic, the child is restless outside of an attack and has poor sleep, it is necessary to exclude neurological disorders that can aggravate the course of physiological intestinal colic. Frequent and profuse regurgitation is also a reason to consult a specialist in order to exclude surgical and neurological pathologies. Fever accompanying the pain syndrome requires professional observation and differential diagnosis.
Where to go?
The doctors of the 5th Clinical Hospital have extensive experience in performing laparoscopic operations and hernioplasty in Minsk.
In addition to accepting patients who are citizens of Belarus, the 5th City Hospital of Minsk also accepts foreign citizens (on a paid basis). Each of them can undergo comprehensive diagnostics and treatment at the surgical and therapeutic departments.
The hospital has its own clinical diagnostic laboratory, X-ray department, X-ray CT and MRI rooms. The physiotherapy department has all the conditions for conducting rehabilitation programs.
Prevention
Doctors at the 5th Hospital will not only select the optimal diagnostic and treatment option for each patient, but will also advise on how to prevent relapses.
Diet occupies a special place among measures to prevent intestinal and stomach diseases. It is important to learn to maintain balance in nutrition. You should not overeat; you should chew food carefully and slowly. Water and willow tea https://teahelp.ru/tea/herbal-tea/ivan-chaj/ should be consumed in sufficient quantities; coffee is not recommended in this case. At the same time, when choosing a diet, experienced doctors take into account all factors:
- functional state of the intestines, liver, pancreas
- secretory function of the stomach,
- intestinal motility,
- the presence of other concomitant diseases.
In addition to your diet, it is important to reconsider how you store and process food. Do not leave food open in the sun. Avoid damp food storage areas. Otherwise, they may begin to mold and rot. Avoid contact between raw foods and cooked foods.
Exercise therapy is also of great importance in the complex of preventive measures. Instructors-methodologists select their own loads and exercises for each patient.
Lists of permitted and prohibited products
The diet helps reduce inflammation in the gastrointestinal tract, normalize bowel movements, whether diarrhea or constipation, by eliminating certain foods that cause excess bile and digestive enzymes. When compiling a treatment menu, it is recommended to exclude from the diet
:
- rich broths, first courses with pasta and whole grain cereals;
- flour products (only white bread crackers are allowed);
- fatty meat, fish;
- dairy products;
- all legumes;
- vegetables (can only be used for decoctions)
- fresh and dried berries and fruits;
- sparkling water, coffee, strong tea;
- sauces and spices, marinades and canned food, sausages.
Can be included in the menu
:
- soups from lean fish, meat and vegetables;
- wheat crackers (100-200 g per day);
- white meat turkey, rabbit, chicken, lean veal and beef;
- oatmeal, rice and buckwheat (we are talking about pureed cereals);
- cocoa without milk, herbal infusions;
- butter (5 g per meal);
- soups with a slimy consistency, cooked in low-fat meat, fish broth or vegetable broth, with well-cooked cereals, noodles or noodles, the addition of meatballs is allowed.
Breakfast options you can cook
:
- oatmeal (ground) in water with butter, soft-boiled egg;
- oatmeal and boiled chicken in the form of pate with a little butter;
- casserole of buckwheat and fresh (homemade) cottage cheese in breadcrumbs with egg;
- casserole (soufflé) of rice without milk with eggs and butter, crackers;
- steamed chicken cutlets with butter and egg, rice on water.
Lunches
:
- low-fat chicken broth with semolina, grated buckwheat in water, steamed chicken cutlets;
- soup with meatballs and rice, buckwheat with steamed cutlets;
- light broth with rice and chicken soufflé with eggs and butter in the oven, toasted bread;
- steamed fish cutlets, buckwheat porridge, light vegetable broth with semolina;
- steamed turkey cutlets, water rice, turkey fillet broth with breadcrumbs;
- light broth soup with pureed beef and buckwheat, rice with steamed cutlet.
Dinners
:
- steamed omelette;
- buckwheat casserole with egg;
- soufflé made from rice, eggs and chicken;
- baked fish fillet and rice porridge;
- steamed turkey (or fish) cutlets, buckwheat porridge;
- buckwheat porridge and two soft-boiled eggs.
Green tea, coffee, decoctions of rosehip, currant, quince and bird cherry diversify the drinking regime and the vitamin composition of the diet.