Published: 09/24/2021 12:05:00 Updated: 09/24/2021
Peritonitis is an inflammatory lesion of the peritoneum, the serous membrane covering most of the internal organs and lining the walls of the abdominal cavity from the inside. In most cases, it occurs as a complication of infectious and inflammatory diseases or injuries in the chest and abdomen. The patient's condition is often severe, with intense abdominal pain, vomiting, fever and other symptoms. Treatment is aimed at combating the infectious pathogen, most often of bacterial origin, and always includes abdominal surgery.
The peritoneum performs several important functions:
- regulates the volume and composition of fluid filling the abdominal cavity;
- provides mechanical and immune protection of internal organs;
- limits the source of infection due to the formation of adhesions, preventing the spread of the pathogen throughout the body.
Its inflammation leads to disruption of vital organs and the development of adverse pathophysiological reactions that are dangerous to humans.
Causes
Typically, inflammation of the peritoneum is caused by a bacterial infection.
Often these are representatives of the normal microflora of the digestive system - enterobacteria, E. coli, Proteus, cocci, clostridia and other microorganisms. Less commonly, pathogens include gonorrhea, tuberculosis, hemolytic streptococcus or pneumococcus. Depending on the route of penetration of the pathogen into the abdominal cavity, three types of pathology are distinguished. Primary peritonitis develops when the pathogen migrates from other foci of inflammation along the bloodstream, fallopian tubes in women, or with the lymph flow. This is possible with diseases of the pelvic organs, including gynecological diseases, inflammation in the gastrointestinal tract, and infectious kidney lesions.
Secondary peritonitis is not an independent disease, but a complication of destructive and inflammatory lesions of the abdominal organs. Peritonitis can also be caused by penetrating injury to the abdominal wall or blunt trauma to the abdomen with rupture of internal organs, postoperative complications and errors during surgical interventions. Separately, it is worth noting inflammatory lesions of the peritoneum due to malignant tumors, helminthic infestation, granulomatous and rheumatoid processes in the body.
Tertiary peritonitis occurs two days after removal of the focus of secondary peritonitis. The reason for its appearance is that the patient’s body was unable to form an adequate response to the infectious process.
Prognosis and prevention
If left untreated, an appendicular abscess can spontaneously rupture into the intestinal lumen, abdominal cavity or retroperitoneal space, sometimes into the bladder or vagina, and very rarely through the abdominal wall to the outside. The prognosis is serious, the outcome of the disease is determined by the timeliness and adequacy of surgical intervention. Prevention of appendiceal abscess consists of early recognition of acute appendicitis and performing an appendectomy in the first 2 days.
You can share your medical history of what helped you in the treatment of appendiceal abscess.
Classification
Peritonitis is of the following types:
- bacterial – caused by microbial flora;
- abacterial - with aseptic or toxic-chemical inflammation of the peritoneum due to its irritation by aggressive non-infected fluids (blood, digestive enzymes and secretions of internal organs, urine);
- special forms - parasitic, rheumatoid, carcinomatous and granulomatous.
According to the course of the disease, peritonitis is divided into acute and chronic.
According to the area of the affected peritoneum, inflammation can be limited, local (with damage to 1-2 anatomical areas), diffuse (covering three or more areas) and general (with total inflammation).
In its development, the disease goes through an early phase (less than twelve hours), late (less than five days) and final (from one to three weeks from the onset of inflammation).
Anatomy of the rectum and perianal region, functions of the obturator apparatus
The rectum and anal canal are the final sections of the digestive tract. The immediate tasks of the rectum are the accumulation, formation and excretion of intestinal contents and gases. The functions of the anal canal are unique: a system of nervous reflexes and a complex muscle complex provide one of the most important functions of the body - control of bowel movements, as well as differentiation of the composition of intestinal contents without the need for conscious assessment and subsequent “smart” control of evacuation. In other words, a healthy person most of the time does not think about what kind of contents are in the rectum, whether it is necessary and whether it is possible to retain it in a given situation. All this is controlled unconsciously, thanks to multi-level neuromuscular self-regulation of the holding process.
The approximate boundary between the rectum and the anal canal on the side of the mucous membrane (lumen) of the intestine is formed by the so-called dentate line. There are vertical folds on it, alternating with depressions - crypts. The ducts of the anal glands open into the crypts. The mucus produced by these glands facilitates the sliding of intestinal contents as they pass through the anal canal. Circumstances such as trauma, swelling of the mucous membrane due to defecation disorders, chronic intestinal diseases can lead to inflammatory changes in the crypts and anal glands.
Outside the mucous membrane there is a complex of muscles - these are the sphincter muscles mentioned above, which provide the function of retention and excretion. There are internal and external sphincters. The internal sphincter forms the so-called resting tone, uninterruptedly ensuring the tightness of the anal canal. Its regulation and reduction occur unconsciously, that is, without our will. The external sphincter surrounds the internal one and consists of several layers (portions). Its reduction occurs due to our volitional effort (Fig. 1).
Figure 1. Schematic representation of the rectal sphincters
Symptoms
Acute peritonitis occurs in three stages, each of which has its own manifestations.
On the first day from the onset of peritonitis, in the reactive stage, a local reaction to irritation of the peritoneum is noted. Initially, pain is localized where the source of inflammation is located, and can radiate to the shoulder, under the collarbone. Subsequently, the pain spreads throughout the abdomen. To alleviate the condition, a person assumes the “embryo” position, lying with his legs pressed to his stomach. The patient is concerned about dry mouth, nausea and vomiting, and loss of appetite. The toxic stage develops between four and seventy-eight hours. Characterized by increasing intoxication up to endotoxic shock, increased general manifestations - blood pressure decreases, heart rate increases, body temperature rises and breathing problems appear. The pain is diffuse in nature, its intensity decreases, as paralysis of the nerve endings of the peritoneum begins, bloating and constipation are noted.
In the terminal stage, after seventy-two hours from the onset of inflammation of the peritoneum, a gross disruption of vital processes inside the body occurs. The symptoms of peritonitis are dominated by manifestations of paralytic intestinal obstruction - intense abdominal pain, severe vomiting that does not bring relief, and severe bloating. The patient's condition is extremely serious, facial features are sharpened, blood pressure is sharply reduced, urine does not pass, consciousness is confused, limbs acquire a bluish or yellow tint, increased sweating and other signs of multiple organ failure are characteristic.
Chronic peritonitis is characterized by “blurred” symptoms that arise as a result of prolonged intoxication and the formation of adhesions in the abdominal cavity, disrupting the functioning of internal organs.
Pathology manifests itself:
- lack of appetite and weight loss;
- increased sweating;
- persistent low-grade fever up to 37.5 °C;
- bowel dysfunction;
- periodic abdominal pain and bloating.
Adhesions and dense scar cords make it difficult to empty the hollow organs, which is accompanied by dyspeptic symptoms - nausea, vomiting, flatulence, urination and menstrual disorders.
Prognosis for recovery
The mortality rate for septicemia ranges from 10 to 40%. It is higher among patients who develop septic shock. The prognosis mainly depends on three factors: [2]
- Types and characteristics of the infectious agent.
- Features, physiology of the patient’s body.
- Depending on how correct and timely the diagnosis was made, treatment began.
Euroonco clinics in Moscow and St. Petersburg have intensive care units equipped with all the necessary equipment. We have every opportunity to quickly and fully provide assistance to a patient in a condition of any severity.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Sepsis: classification, clinical diagnostic concept and treatment: a practical guide / ed. V.S. Savelyeva, B.R. Gelfand. - Moscow, 2010. - 352 p.
- V.A. Rudnov, V.V. Kulabukhov. Sepsis 3: updated key points, potential challenges and next practical steps. Messenger of Anesthesiology and Resuscitation, Vol. 13, No. 4, 2016. DOI 10.21292/2078-5658-2016-13-4-4-11
- Intensive care of sepsis: textbook / D.V. Martynov, V.M. Zhenilo, A.A. Bychkov, V.N. Malygin; Federal State Budgetary Educational Institution of Higher Education Rost State Medical University of the Ministry of Health of Russia, department. anesthesiology and resuscitation - Rostov n/a; Publishing house RostGMU, 2016. – 64 p.
- Kurmukov I.A., Kashiya Sh.R., Obukhova O.A., Pronina A.M., Yunaev G.S. Primary diagnosis of sepsis in patients receiving drug treatment for cancer: comparison of SIRS and SOFA criteria. Translational medicine. 2017;4(2):46-51. https://doi.org/10.18705/2311-4495-2017-4-2-46-51
- The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)/ M. Singer, CS Deutschman [et al.]// JAMA.- 2016.- Vol. 315(8).-P. 801-810
- Angus DC, van der Poll T. Severe sepsis and septic shock // N. Engl. J. Med. 2013. Vol. 369. P. 840-851. Hemodynamic support for septic shock / V.A. Rudnov, F.N. Brezgin: methodological manual. - Ekaterinburg, 2012. - 24 p.
- Sepsis: current dogma and new perspectives/ CS Deutschman, KJ Tracey// Immunity.- 2014.- Vol.40 (4).- P. 463-475
- Sepsis definitions: time for change/ JL Vincent, SM Opal, JC Marshall, KJ Tracey// Lancet.- 2013.-Vol. 381(9868).- P.774-775
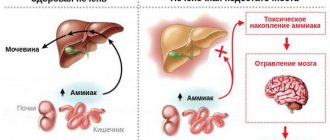
Complications
Peritonitis in children and adults is dangerous due to the development of multiple organ failure and intoxication of the body. Among the complications of the acute process:
- dehydration;
- renal failure;
- toxic shock;
- pulmonary pathologies;
- liver failure;
- secondary inflammatory processes.
Peritonitis after surgery may be accompanied by the formation of fistulas and abscesses of internal organs, and suppuration of postoperative sutures. The appearance of a number of complications is possible far beyond the abdominal cavity - occlusion of deep veins, inflammation of the lungs and pleura, mediastinitis.
1.General information
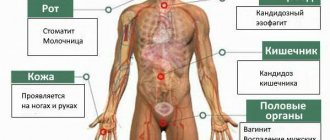
An abscess is a suppurating closed cavity in a tissue or organ, sealed by a granulation membrane, usually painful and disrupting the functioning of the affected structure; The general condition often worsens, significantly, and in some cases the situation becomes life-threatening. In general, everything depends on the location, size and dynamics of abscess formation.
Abscesses are very diverse, given the complexity of the human body, but their common specific feature is that such infiltration always develops as a natural consequence of an infectious-inflammatory process and is always caused by purulent fusion of tissues, i.e. mass death and destruction of cells due to the activity of a pathogenic microorganism. It is these “remains”, together with the waste products of the infectious pathogen, that form a purulent mass, which, accumulating in a closed volume, can exert significant and painful pressure on the surrounding tissues. Not only “traditional” pyogenic streptococci and staphylococci, but also many other bacterial, protozoal, and fungal cultures can act as a pathogen.
An abscess is always, at a minimum, unpleasant, even if it is “just an abscess” on some relatively safe area of skin (according to a well-known saying, abscesses are easily tolerated except on someone else’s back). But if the purulent infiltration is multiple, develops rapidly and/or affects vital organs, it can be very dangerous: a breakthrough of the hermetic membrane and the outpouring of purulent contents into the surrounding space is fraught with fatal intoxication and sepsis. Therefore, a diagnosis such as an abdominal abscess requires the most serious response measures.
A must read! Help with treatment and hospitalization!
Diagnostics
If, during a conversation with the patient and examination, the doctor suspects peritonitis in an adult or child, the patient is urgently hospitalized in a hospital inpatient unit, where further laboratory and instrumental studies are carried out to clarify the diagnosis.
The list of tests for peritonitis includes:
- Clinical blood test. During the purulent process, an increase in the number of leukocytes is determined, accelerated ESR, and the hematocrit changes.
- Biochemical blood test to determine indicators such as C-reactive protein, aspartate aminotransferase, alanine aminotransferase, total bilirubin, blood sugar, creatinine, lactate dehydrogenase, amylase, lipase, procalcitonin, interleukins 1, 6, 8, 10, tumor necrosis factor, urea, total protein and albumin.
- Hemostasis indicators, fibrinogen concentration, prothrombin time, INR, APTT.
- Content of electrolytes in the blood.
- General urine analysis.
Instrumental diagnosis of peritonitis consists of ultrasound and survey R-graphy of the abdominal organs, electrocardiography, magnetic resonance and computed tomography. In complex clinical cases, to clarify the nature of the causative agent of the disease and confirm peritonitis, abdominal puncture, bacteriological examination of peritoneal exudate and laparoscopy are performed.
Treatment
Treatment of peritonitis is always surgical, with mandatory preoperative drug preparation.
The latter is aimed at replenishing the balance of fluids, salts and normalizing the patient’s condition, as well as adequate pain relief and normalizing blood pressure. During surgery for peritonitis, the source of infection is eliminated, pus and peritoneal effusion are removed, the abdominal cavity is washed with antiseptic solutions and drained. Postoperative management of the patient includes a course of powerful antibiotic therapy, drips with detoxification solutions, medications to support the functioning of the cardiovascular system, respiratory system and nervous system.
Author:
Pugonina Tatyana Alekseevna, Therapist