- home
- Treatment of cancer (oncology)
- Gastrointestinal tumors
- Operations for esophageal cancer
—
—
—
In case of esophageal cancer, the malignant tumor first affects the inner layer, the mucous membrane, and then the outer layer - the submucosal and muscular layers.
There are 2 types of this pathology:
- Squamous cell carcinoma. Develops in the cells of the esophageal mucosa. Occurs in the neck and chest area.
- Glandular cancer (adenocarcinoma). Develops in the lower part of the esophagus.
The main method of treating a malignant tumor in the esophagus is surgery. Surgery is recommended in the following cases:
- For complete resection of the pathological focus.
- To remove as much of the tumor as possible.
- To restore the gastrointestinal tract after removal of the esophagus.
- To relieve symptoms in the late stages in the presence of metastases.
To understand what kind of operation a patient needs, the doctor looks at the volume, degree and location of the pathological focus, the presence or absence of previous operations, the age and physical condition of the patient.
Minimally invasive surgeries
- Remote consultation
- We will select the best treatment for you
Call me back!
Reconstructive surgery for esophageal cancer
This operation helps to restore the functioning of the digestive tract after removal of a malignant tumor. Usually performed immediately after excision of the pathological focus.
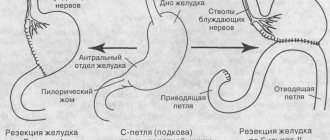
Plastic surgery using the stomach
When resection of part or the entire esophagus, the most optimal solution is to pull the stomach up, form a tube from the organ and connect it to the remaining segment of the esophagus. This procedure is called esophagogastric anastomosis.
Reconstruction using the large or small intestine
There are cases when the stomach cannot be used in reconstructive surgery. Then the doctor uses part of the intestine. This is usually a segment of the large or small intestine.
Advantages of this technique:
- safety: controlled depth of exposure (reduces the risk of developing cicatricial changes in the esophagus);
- efficiency: eradication (eradication) after the first procedure ≥ 90%;
- reducing the risk of “buried” Barrett through controlled application of energy and uniform removal of epithelium;
- easy to use, does not require much time: energy transfer
- rapid restoration of normal mucosa;
- Possibility of use for large lesions;
- is a minimal intervention and does not require a long hospital stay.
The European Society of Gastrointestinal Endoscopy recommends RFA as the most effective and safe method for treating Barrett's esophagus.
Approaches to surgery for esophageal cancer
Cavity (open) approach
During the operation, long incisions are made in the abdomen, chest or neck. Next, a feeding tube is placed in the stomach or mid-small intestine. This helps the patient recover and get the nutrition he needs.
Transhiatal approach
The doctor cuts into the abdominal cavity, frees the internal organs from tissue and removes the tumor, part of the stomach and some lymph nodes.
An option is possible in which the left side of the neck is cut, some parts of the esophagus are freed from tissue and an anastomosis is performed.
Transthoracic approach (Ivor-Lewis approach)
The abdominal cavity is cut, the stomach is freed from tissue, and the chest is cut on the right side. Then the esophagus or some part of it is removed. Next, a tube is made from the stomach and connected to the remaining segment of the esophagus.
Thoracoabdominal approach
Recommended when cancer has spread to the lower esophagus or upper stomach. The patient's abdomen is cut from the middle upward, towards the left side of the chest. The pathological focus is removed, and then a tube is formed in the same way as in the previous approach.
Radical esophagectomy
This procedure is performed when stage 1-3 cancer has spread to the lower part of the esophagus and there is a risk of it spreading to other organs. During the operation, the esophagus, abdominal tissue, lymph nodes, spleen, and part of the stomach are removed. Sometimes other nearby organs can be resected. Next, the stomach or part of the intestine is connected to the remaining esophagus.
Laparoscopic esophagectomy
Used in the early stages of cancer. 4-6 small incisions are made on the person’s body and the tumor is removed using a laparoscope. After this procedure, the patient recovers faster, and the risks of complications are reduced.
Our expert in this field:
Rudakova Maria Nikolaevna
Deputy Chief Physician, Oncologist-Surgeon, Doctor of Medical Sciences
Doctor of Medical Sciences
Experience: More than 30 years
Call the doctor
Call the doctor
Send documents by email The possibility of treatment will be reviewed by the chief physician of the clinic.
Surgery
SIGN UP FOR A CONSULTATION +7 (812) 951-7-951
Surgical treatment of esophageal cancer is one of the most difficult areas in surgery and oncology. When choosing the scope of surgical intervention, a comprehensive examination of the patient is performed. The complex, along with clinical studies (thorough history taking, examination, palpation, percussion, auscultation, examination of blood and urine parameters, external respiratory function, ECG, height and weight ratio), includes a polypositional x-ray examination of the esophagus, x-ray examination of the lungs and stomach , endoscopic examination (esophagoscopy, tracheobronchoscopy), ultrasound examination of the abdominal organs (liver, pancreas, kidneys, retroperitoneal tissue in the area of the fork of the celiac trunk, para-aortic zone) and mediastinum, as well as computed tomography (X-ray or NMR). In addition, an examination is carried out for the presence of concomitant diseases. When concomitant diseases of the cardiovascular system are identified, patients without clinical signs of decompensation or unstable circulatory compensation, unstable angina, or uncorrectable arterial hypertension are considered functionally operable. The presence of signs of ischemia, cicatricial changes in the myocardium, blockades, and cardiac arrhythmias are regarded as relative contraindications to surgery, which require an in-depth study of the cardiovascular system, coronary circulation, and exercise tolerance. Patients with satisfactory tolerance to physical activity and the absence of negative dynamics on the ECG are considered functionally operable. Absolute contraindications to surgery are grade IY pulmonary ventilation insufficiency and acute myocardial infarction within 6 months. The risk of surgery is increased in patients with excess weight of more than 20% and significant weight deficiency. With concomitant diseases of the kidneys and liver, patients who do not have severe exacerbations of intercurrent diseases and clinical and laboratory signs of hepatic-renal failure are considered functionally operable. The final stage of diagnosis is revision laparotomy (abdominal stage) in order to finally resolve the issue of metastatic spread of the tumor process below the diaphragm. Depending on the treatment plan developed, the abdominal stage can be completed in different ways. In cases of extensive metastasis to the lymph nodes below the diaphragm, especially to the para-aortic and retroperitoneal (excluding the lymph nodes along the left gastric artery and along the upper edge of the pancreas in the tail and body), the abdominal stage ends with gastrostomy. The simplest and most reliable option for this operation is the formation of a stalk-type gastrostomy from the anterior wall of the stomach closer to the lesser curvature. The choice of indications for surgery is also determined by the level of damage to the esophagus. So, the higher the esophageal tumor is localized, the less likely it is to perform one-stage resection and plasty of the esophagus. This is due to the need to supplement surgical treatment with radiation therapy or chemo-radiation treatment, and the artificial esophagus formed during plastic surgery would inevitably fall into the irradiation zone, which is undesirable. In other words, indications for surgery of a particular volume depending on the location of the tumor process in the esophagus should be considered separately. Differences in indications for surgical intervention of a particular volume, in addition to the localization of the process, also depend on the characteristics of metastasis of esophageal cancer and the need to cover different zones of regional metastasis with therapeutic effects, as well as on the degree of risk of surgical intervention due to differences in surgical trauma. In case of cancer of the cervical and upper thoracic esophagus, when planning the scope of the operation, preference should be given to extirpation of the esophagus using the Dobromyslov-Torek method. One-stage esophageal plasty should be avoided due to the need for postoperative radiation therapy to areas of regional metastasis and the bed of the removed esophagus. Subtotal resection of the esophagus according to Dobromyslov-Torek, refusing simultaneous resection and plasty of the esophagus, should be resorted to in cases of palliative resection of the esophagus, i.e. when the surgeon was unable to completely remove the tumor tissue due to direct tumor growth into adjacent anatomical structures (aorta, main bronchi, trachea, spine, pericardium), or intimate adhesion to these organs, as well as extensive metastasis to regional lymph nodes that can be removed, including cases with metastases on both sides of the diaphragm. This operation should also be performed in patients with low functional indicators, which limit the ability to perform traumatic, time-consuming interventions. Esophagoplasty should be performed in these cases after 4-6 months if there are no signs of disease progression according to an in-depth examination. In other cases, if the process is resectable, one-stage resection and plasty of the esophagus should be considered the operation of choice. In case of cancer of the lower thoracic esophagus, as well as in cases of damage to the abdominal segment of the esophagus and transition to the stomach, simultaneous resection and plastic surgery of the esophagus with an isoperistaltic stem from the greater curvature of the stomach with extracavitary cervical anastomosis is indicated. In some cases, with a slight extent of the process (within stages I-II) with such a localization of the tumor lesion, resection of the lower thoracic esophagus and proximal stomach can be performed with the imposition of an esophageal-gastric anastomosis under the arch or at the level of the aortic arch, or a Lewis or Garlock operation. The optimal completion of a one-stage resection and plasty of the esophagus can be considered the formation of a cervical extracavitary esophageal-gastric anastomosis. The extracavitary location of the anastomosis also has the advantage that if the anastomosis sutures fail, there are no fatal consequences for the patient. In some cases, due to surgical trauma to the remaining part of the esophagus and its displacement from the posterior mediastinum to the neck, its nutrition is disrupted. In this case, the honey of choice is delayed formation of the cervical esophagogastric anastomosis. Delayed esophageal plasty is performed, as mentioned above, 4-6 months after resection of the esophagus, if there are no signs of progression of the process. We are fundamental supporters of tubular esophagoplasty of the greater curvature of the stomach, but do not reject the possibility of using other segments of the gastrointestinal tract for esophagoplasty. The latter is important in cases where surgery on the esophagus was preceded by surgery on the stomach (resection of a certain volume or gastrectomy). In cases where it is impossible to use the stomach as a material for plastic surgery of the esophagus, options for intestinal esophagoplasty are used, including free transplantation of a segment of the small intestine with microsurgical intervascular anastomoses. The use of microsurgical techniques is also used when it is necessary to revascularize the gastric tube in cases of damage to the right gastric artery and the veins accompanying it, as well as in cases of insufficiency of venous outflow and the development of venous stagnation in the veins of the gastric tube. Operations Abdominal stage. The task of the abdominal stage is, first of all, to revise areas of regional metastasis below the diaphragm. The patient's position is on the back with a bolster at the level of the xiphoid process of the sternum. Access: upper-median laparotomy. Audit and mobilization for audit. With the right hand, the condition of the paracardial right and left lymph nodes, nodes of the lesser omentum and along the course of the left gastric artery is palpated. For better orientation and assessment of the condition of the lymph nodes in the area of the fork of the celiac trunk, the omental bursa is opened in the avascular area closer to the liver. Lymph nodes suspicious for metastasis are verified using a puncture biopsy; in some cases they are removed for morphological examination, as well as to study the sensitivity of the tumor to chemotherapy. Palpation and visual assessment of the condition of the liver surface. Suspicious areas are punctured. In the absence of irremovable metastases to organs and regional lymph nodes below the diaphragm and the tumor is localized in the mid-thoracic esophagus or in its lower third with transfer to the stomach with a resectable process, it is possible to perform a simultaneous resection and plasty of the esophagus in an independent surgical plan, or, preferably, in combination with postoperative radiation therapy. The latter option is currently the dominant one. When the lesion is localized in the upper thoracic and cervical esophagus, the abdominal stage ends with gastrostomy from the anterior wall of the stomach. Then extirpation of the esophagus is performed with the formation of a pharyngostomy or subtotal resection of the esophagus with the formation of a high esophagostomy in the neck. The technique of gastrostomy from the anterior wall of the stomach is quite simple: a ligature holder is placed on the anterior wall of the stomach at the lesser curvature, 8-10 cm away from the pylorus. The second holder is applied 6 cm in the distal direction. Using handles, lifting the anterior wall of the stomach, a fold is formed and the jaws of the NZhKA-60 apparatus are placed on it in the antiperistaltic direction so that a conical tube is formed with the base towards the stomach. The mechanical suture line is peritonized with separate interrupted seromuscular sutures. The top of the formed tube is brought out through an additional incision in the left hypochondrium and fixed with two sutures to the aponeurosis. When forming an additional incision, it is better to cut the skin in a horizontal direction, and the aponeurosis in a vertical direction, preserving the fibers of the rectus abdominis muscle, which are pulled apart with Farabeuf hooks. The abdominal cavity is checked for the absence of bleeding and after this the laparotomy wound is sutured tightly. Then, by cutting off the top of the stem, its lumen is opened and the external opening of the gastrostomy is formed by suturing the mucous membrane to the skin with separate interrupted sutures. A thin rubber tube is inserted into the stomach through the opening of the gastrostomy tube for feeding and decompression. Subsequently, by introducing gastric tubes with a gradually increasing diameter, the width of the gastrostomy opening is brought to the optimal value. Subtotal resection of the esophagus. The purpose of this operation is to remove en bloc the thoracic esophagus with the tumor, surrounding tissue, paratracheal, upper and lower tracheobronchial (bifurcation), posterior mediastinal (paraesophageal) lymph nodes. Position the patient on the left side with a bolster at the level of the angle of the shoulder blades. Access: right anterolateral thoracotomy along the fifth intercostal space if the upper and middle third of the esophagus is affected and along the sixth intercostal space if its lower third is affected. Palpation and visual assessment of the condition of the parietal, visceral pleura and lung tissue in order to detect possible metastases. In the absence of signs of tumor dissemination in the pleura, the lung is retracted anteriorly. The condition of the mediastinal lymph nodes is assessed by palpation and the location, level and extent of damage to the esophagus is assessed. Next, mobilization of the esophagus and revision of the mediastinum begin. Mobilization for audit and audit. The inferior pulmonary ligament is divided and the lung is bluntly mobilized to the inferior pulmonary vein, displacing the lymph nodes to the esophagus. The mediastinal pleura is dissected above the esophagus in front of it and behind it all the way from the diaphragm to the dome of the pleura, leaving a strip about 3 cm wide on the esophagus. Next, the upper and lower edges of the tumor are determined by palpation, its connection with the spine, aorta, trachea, and main bronchi is assessed. Above and below the tumor at a distance of 3-4 cm, a finger is walked around the esophagus, and rubber holders are passed through the formed channels. When pulling on them, the possibility of removing the esophagus is assessed again.
Mobilization for resection. By blunt and sharp means, with the help of clamps and ligation of vascular formations, the esophagus with the surrounding tissue, paraesophageal lymph nodes (from the diaphragm to the upper thoracic aperture), and a single block with the bifurcation lymph nodes are isolated. In this case, if possible, it is necessary to preserve the branches of the vagus nerves extending to the lungs. When mobilizing in the middle third of the esophagus, the esophageal arteries, usually originating from the anterior surface of the aorta, are crossed and ligated. Below the origin of the pulmonary branches, the vagus nerves are crossed. When a tumor grows into the azygos vein, it is isolated, sutured with a US device and additionally bandaged. If there is no germination, the azygos vein is preserved. After mobilizing the esophagus and peri-esophageal tissue along the entire length of the intrathoracic esophagus, the esophageal-diaphragmatic ligament is incised and the esophagus is mobilized in the area of the esophageal opening of the diaphragm. By pulling the esophagus into the pleural cavity, the cardiac part of the stomach is removed. At the level of the cardiac sphincter, the vagus nerves are crossed, the esophagus is sutured with two UO devices and crossed between mechanical sutures. The proximal end of the esophagus is placed in a rubber cap or covered with a napkin. The distal line of the mechanical suture is immersed with interrupted sutures, then the esophageal opening of the diaphragm is sutured. The proximal border of esophageal resection should be at least 5 cm from the upper edge of the tumor. At this level, the esophagus is sutured with a UO apparatus and a clamp is applied below. The esophagus is crossed between the apparatus and the clamp. The drug is removed. If the tumor is localized in the upper third of the esophagus, the esophagus is sutured with a UO apparatus and crossed under the dome of the pleura. An urgent morphological examination is carried out along the proximal and distal resection edges to exclude possible intersection of the esophagus along the tumor. The pleural cavity is washed with antiseptic solutions and, after checking for hemostasis and the tightness of the lung (if manipulations were performed on it), it is sutured tightly, leaving two pleural drains (the upper one at the level of the 2nd intercostal space and the lower one at the level of the 7th intercostal space). Cervical stage of the operation. With the patient in the supine position with a bolster at the level of the shoulder blades and a slight turn of the head to the right, the skin and soft tissue are dissected in layers along the medial edge of the left sternocleidomastoid muscle (sternocleidomastoid) to the pretracheal fascial plate, dissected longitudinally. The vascular bundle is shifted outward with a blunt hook. The remaining part of the cervical esophagus is brought into the wound and sutured deep into the wound to the surrounding muscles, sealing the mediastinum. The wound is sutured down to the esophagus. The muscular wall of the esophagus above the mechanical suture is dissected to the submucosal layer. Part of the esophagus with a mechanical suture is removed. The mucous membrane is sutured to the skin of the neck. Upon receipt of data from an urgent morphological study about the presence of tumor elements in the resection margin, an additional 1-2 cm of the esophagus is resected and only then an esophagostomy is formed. In cases where the tumor lesion is localized high up to the pharynx, the remaining part of the esophagus is extirpated. To do this, the incision is extended higher, the left lobe of the thyroid gland is widely exposed, the inferior thyroid artery is crossed with ligation, tracing the course and preserving the left recurrent nerve and parathyroid bodies. By pulling out the stump of the esophagus, they mobilize it to the laryngopharynx. The edge of the sternocleidomastoid muscle is sutured to the prevertebral fascia deep in the wound. This achieves sheltering of the vascular bundle and sealing of the upper mediastinum. The edges of the skin are separated to the sides. The laryngopharynx is opened, the edge of the skin is sutured along the edge of the remaining part of the laryngopharynx deep in the wound, forming a lateral pharyngostomy. Delayed esophagoplasty with an isoperistaltic stem from the greater curvature of the stomach. With the patient in the supine position. Access: upper-median laparotomy. The abdominal cavity is opened layer by layer with excision of the postoperative (after the abdominal stage) scar. The revision is carried out in the same way as when performing the abdominal stage. In the absence of tumor dissemination in the abdominal cavity and unremovable metastases in regional areas, mobilization of the stomach begins. The external opening of the gastrostomy tube is excised. Its hole is sutured, and the tube is moved into the abdominal cavity with the mouth of the gastrostomy tube pre-sutured. The stomach is mobilized along the greater curvature from the pylorus to the fundus by crossing and ligating the gastrocolic ligament, 5 cm away from the stomach wall in order to preserve the gastroepiploic vessels. Subsequently, these vessels will be the main blood circulation for the artificial esophagus. The short gastric vessels are ligated and divided directly at the hilum of the spleen. Then they begin to mobilize the stomach along the lesser curvature. Closer to the liver, the lesser omentum is ligated and transected along its entire length. At a distance of approximately 4-5 cm, the right gastric artery is ligated and divided. The peritoneum above the gastro-pancreatic ligament is opened. Fiber with lymph nodes is shifted to the stomach, highlighting the left gastric artery and veins. The artery and vein are crossed and ligated with suturing at the origin. Departing from the pyloric sphincter by 4-5 cm along the lesser curvature, using UO-60 devices along the greater curvature, a gastric tube 3-4 cm wide is formed. To obtain a sufficient length of the gastric tube, the stomach is stretched along the greater curvature before applying the staplers. To seal the tube between individual fragments of the mechanical seam, the last bracket of the previous step is included at the beginning of the next one. The mechanical suture line is covered with interrupted seromuscular sutures. The formed gastric tube (about 38 cm) is passed into a preformed presternal canal with preliminary resection of the xiphoid process of the sternum and covering the resection site with the peritoneum. The canal is drained with two parastem rubber active drains. The gastric tube is fixed to the fascia at the beginning of the presternal canal. When placing an artificial esophagus, they try to ensure that the upper end of the tube extends beyond the lower end of the remaining part of the esophagus by 3-4 cm in order to create better conditions for the formation of a cervical esophageal-gastric anastomosis in the future. After checking for hemostasis, the laparotomy wound is sutured tightly. Formation of cervical esophageal-gastric anastomosis. The end of the own esophagus is mobilized with a bordering incision around the esophagostomy for about 3 cm. The muscular layer is cut circularly around the stoma, then the mucous membrane is cut off. The wall of the gastric tube is dissected along the posterior right wall at the level of the esophagostomy along the diameter of the esophagostomy to the submucosal layer. Then, with separate interrupted sutures, the muscular membranes of the stump of the esophagus and the gastric tube are sutured along the posterior lip of the anastomosis being formed. The lumen of the gastric tube is opened and the second row of anastomotic sutures is formed with intraluminal interrupted sutures along the anterior and posterior semicircles of the anastomosis. Then a second row of seromuscular sutures is formed on the anterior wall of the anastomosis. The formation of an anastomosis of the “end to side” type is optimal. The skin over the anastomosis is sutured to the mouth of the apex of the gastric tube, where the opening of the gastrostomy is formed by suturing the mucous membrane to the skin. A thin rubber tube is inserted into the gastrostomy opening for feeding and decompression. If there is no confidence in the quality of the blood supply to the artificial esophagus, the anastomosis is formed after 1-3 months. The technique for forming an anastomosis can vary depending on the surgeon’s inclination towards one or another technical option. Simultaneous resection and plasty of the esophagus. The purpose of the operation is to remove the esophagus with tissue, paratracheal, bifurcation, posteromediastinal, left and right paracardial lymph nodes; lesser omentum groups of lymph nodes, as well as lymph nodes along the left gastric artery and the lesser curvature of the stomach. Combined approach: upper-median laparotomy and anterolateral right thoracotomy. The operation begins with the patient in the supine position. The abdominal stage ends with revision. In the absence of signs of distant metastasis, provisional sutures are placed on the laparotomy wound. The patient is turned on his left side. Next, revision and mobilization of the esophagus is carried out as in the case of subtotal resection, with the difference that the esophagus is crossed only along the proximal border of the resection after its mobilization in the area of the esophageal opening of the diaphragm. The esophagus with the tumor, lymph nodes and fiber moves into the abdominal cavity. After checking for hemostasis and drainage using the method described above, the pleural cavity is sutured tightly. With the patient in the supine position, the cervical stage is performed with removal of the cervical segment of the esophagus into the wound. The provisional sutures are removed from the laparotomy wound. The xiphoid process of the sternum is resected, a subcutaneous canal is formed and plugged. Next, the stomach is mobilized as in delayed esophagoplasty and a gastric tube is formed. The preparation containing tissue from the mediastinum, lesser omentum, paracardial and tissue from the gastro-pancreatic ligament, together with the lymph nodes located in it, as well as the lesser curvature of the stomach, is removed. The gastric tube is placed in a pre-formed and drained canal and fixed to the fascia at the level of the xiphoid process. After checking for hemostasis, the laparotomy wound is sutured tightly. Next, a cervical esophagostomy and gastrostomy are formed. In the case of good blood supply to the artificial esophagus and the stump of one’s own, a cervical esophageal-gastric anastomosis is formed according to the method described above. Otherwise, a delayed cervical esophageal-gastric anastomosis is formed.
Share link:
Palliative surgery for esophageal cancer
Surgeries are also performed to stop the development of metastases. The main goal of such a surgical intervention is to alleviate the patient’s condition, relieve him of problems with swallowing, and improve his well-being and quality of life.
Bypass surgery
This procedure is performed if it is impossible to place a stent, and the direction of flow of food or liquid around the tumor needs to be changed. Then the stomach is attached to the upper part of the esophagus, bypassing the pathological focus.
Esophagectomy
This is done only if doctors have sufficient confidence that the patient will survive after this operation. Indeed, during surgery, almost the entire esophagus is cut out, and the remaining segment is connected to the stomach.
Feeding tube
Through it, the patient receives the right amount of nutrients so as not to lose body weight, and medications. If there are metastases and other methods to eliminate the blockage caused by the tumor do not help, then a probe is used. It is inserted into the stomach through the nose (nasogastric tube) or into the small intestine.
FAQ
Is special preparation needed for surgery for achalasia cardia?
Surgery is performed on an empty stomach, with the last meal taken at least 8 hours before the procedure. The patient must inform the doctor in advance about all medications taken; some of them may have to be temporarily excluded.
What types of surgery are there for achalasia cardia, besides esophagomyotomy?
The generally accepted technique is endoscopic bougienage of the esophagus, but the effect of the procedure is short-lived, and tissue rupture and scarring only worsen the situation. However, this method may be recommended for older patients with recurrent achalasia, who have had a history of surgery, and for those who are contraindicated for surgery. In addition, in the treatment of the disease, endoscopic intrasphincteric injection of botulinum toxin is used, recommended for patients who have contraindications to surgery. However, the effect of this technique lasts only 2-3 months.
What complications are possible during surgery for achalasia cardia?
Of course, theoretically, there is a possibility of developing intraoperative complications, such as esophageal perforation, bleeding, damage to the vagus nerves, wound infection, etc. To minimize the likelihood of their occurrence, treatment should be carried out in a specialized clinic equipped with modern equipment.
Features of rehabilitation after surgery for achalasia cardia?
Hospitalization usually lasts two days, already on the day of surgery the patient is allowed to drink, from the next day - liquid food, the diet expands gradually. Full recovery usually takes about 2 weeks. A follow-up examination is carried out 2-3 weeks after the operation; further endoscopic examination is recommended one year after the intervention in order to exclude dysplastic changes in the esophagus.
Refusal of surgery - what is the danger?
The course of the disease is slowly progressive; without surgery, achalasia cardia can lead to thinning of the walls of the esophagus, which can cause the development of various pathologies, including varicose veins of the esophagus, diverticula, peeling of the submucosal layer, etc. In addition, if left untreated, bleeding and perforation are possible walls of the esophagus, general exhaustion. The risk of developing a malignant tumor of the esophagus also increases.
Tags: General surgery Achalasia cardia Hernia Hernia
Reviews
16.11.2021
“I was amazed that the doctors are very attentive to patients, explaining everything down to the smallest detail”
In 2022, on August 16, my older sister flew to Lobnya to undergo examination and, if necessary, treatment at the NACFF oncology clinic.
She lives in the capital Kyrgyzstan...
Read full review
27.10.2021
At the clinic, like at home
30.09.2021
Feedback on the treatment of ovarian cancer at the NACFF clinic
07.09.2021
NACFF patient about treatment, quick examinations and attentive attitude
View all reviews
Hospital, hospitalization, emergency medical care - 24/7, 7 days a week
+7 (495) 259-44-44