Gastric resection is a partial removal of an organ, and the resected part can be very significant - up to 80% with a subtotal version of the operation, while 100% removal or total resection is a gastrectomy.
Surgery for any volume of removal is always a serious test for the patient, not so much with postoperative hunger, but with the daily consequences of reducing the volume of a hollow organ. A small stomach volume is positive only for patients at a bariatric clinic where they are fighting obesity.
- Why is gastrectomy necessary?
- Types of gastric resection
- Main stages of gastric resection
- Postoperative period
- Complications of resection
- Prognosis after gastrectomy
Why is gastrectomy necessary?
First of all, an operation to remove an unhealthy part of an organ is performed for cancer; in oncology, all main types of resections are used, and for early carcinoma in situ - stage 0, innovative endoscopic resection of the mucous membrane is practiced without dissecting the entire thickness of the gastric wall. Main indications for resection:
- Malignant organ damage and benign processes, including polyps of the mucous membrane;
- A long-term and non-healing callous ulcerative lesion of the gastric mucosa with life-threatening complications: bleeding, a hole penetrating through the entire thickness of the wall - perforation, including an omentum covered from the outside - penetration.
- Severe obesity, resistant to all other treatment methods.
The list of contraindications is long, but these are mainly diseases of a “general nature”: chronic diseases in the stage of decompensation, not excluding mental disorders, when it is problematic to undergo any surgical intervention.
Acute inflammatory processes and infections may delay surgery for a while.
Everything is determined by the need; of course, it is dangerous to perform a gastric resection, but there are clinical situations when it is dangerous not to perform the operation. It is important to be in good hands and in a clinic where they understand when and what the patient needs to do in order to preserve life and health, as the specialists of our clinic understand.
Types of gastric resection
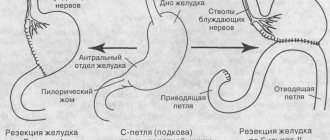
The intervention option is selected based on clinical need, and the name of the operation is based on the volume of the organ part removed or the gastric sections excised:
- The classic version of gastric resection according to Billroth is divided into type 1 and type 2, the difference lies in the connection of the remaining gastric part and the duodenum - end to end or side to side. In modern surgery, the classical technique in its pure form is almost never used, but modifications that improve the result are often used;
- Distal resection involves excision of the lower gastric sections;
- The proximal one, on the contrary, removes the upper part and several centimeters of the esophagus from the body;
- Sleeve, also known as bariatric or longitudinal resection, in the Russian-speaking segment of the Internet is often referred to as drain resection, from sleeve in English, the essence of the intervention is narrowing the cavity to the size of a wide tube;
- Subtotal resection is called according to the volume of removal, that is, almost complete, when less than a third remains, this is a typical operation for cancer, subtotal can be both proximal and distal;
- Reresection or re-resection is performed to prevent cancer recurrence if histological examination reveals cancer cells at the edges of the removed area.
Modern surgery and oncology gravitate toward endoscopic interventions to speed up the patient’s recovery. For cancer, laparoscopic resection is not inferior to open surgery in terms of long-term results.
Euroonco doctors have accumulated vast practical experience in endoscopic interventions, which guarantees our patients a low percentage of postoperative complications with high quality treatment. Vast experience - hundreds of interventions per year for several years.
Dietary recommendations
After surgery, the amount of food you can eat at one time and the length of time food remains in your stomach may change. For this reason, you may need to change your eating habits.
You may also have trouble tolerating foods high in fat or sugar, or both.
Follow the guidelines below. You can also use the sample menus at the end of this resource to help you plan your meals.
Eat smaller meals, but eat them more often
After surgery, you may feel fuller more quickly when eating. This may prevent you from getting enough nutrients. In this case, or if nausea or indigestion occurs, try eating slowly and in smaller portions, but eat more often. For example, try eating half a serving 6 times a day rather than one serving 3 times a day. This will allow you to eat the same amount of food overall, but in smaller portions that are easier to digest.
Eating half servings may also be helpful if you have nausea (the feeling of vomiting) or indigestion.
You may be able to increase your portions over time.
Chew your food thoroughly
Chew your food thoroughly so your body can digest it faster and easier.
Drink enough fluids
Aim to drink about 8 to 10 8-ounce (240 ml) glasses of fluid per day. This will help you prevent dehydration. If you drink more than 4 ounces (115 mg) of liquid at a meal, feeling full may prevent you from finishing your meal.
Avoid eating foods that cause gas.
If you experience bloating or a feeling of fullness, limiting or avoiding foods and drinks that may cause gas may help. Examples of such products:
- Broccoli
- White cabbage
- Brussels sprouts
- Cauliflower
- Beans and legumes (lentils, peas, peanuts)
- Unripe fruit
- Carbonated drinks such as soft drinks or mineral water
Try to avoid these foods and drinks for the first month after surgery. If your symptoms go away after this, you can try adding them to your diet one at a time to see if you can tolerate them.
Include protein in your diet
After surgery, your body will need more protein to recover. Good sources of protein include:
- lean beef: roast from the inside of the rump (eye round);
- roast from the top part of the rump (top round);
- bottom round roast;
- steaks;
- top sirloin steak;
Start with low-fat products
Immediately after surgery, eat low-fat foods. To eat less fat, follow the recommendations below.
- trim all visible fat from meat;
- bake or grill food instead of frying it in oil;
- Spread a thin layer of butter or margarine on the bread.
- Use butter or vegetable oils only as a dressing for vegetables or salad.
- do not eat fatty gravies and creamy sauces;
- Limit your consumption of chips, croissants, donuts and high-calorie desserts such as sponge cakes and cream pies.
- Avoid meat products such as hot dogs, sausages, bacon and cooked sausage.
You can gradually increase the amount of fat in your diet to a level you can tolerate. For more information, see the “Watch for Bowel Changes” section below.
to come back to the beginning
Main stages of gastric resection
For any removal option, the intervention goes through three standard stages:
- Mobilization involves cutting the ligaments that secure the organ inside the abdominal cavity and ligating the vessels before cutting them to prepare the gastric section for removal;
- Cutting off the part of the organ planned for removal from the remaining intact area of the gastrointestinal tract;
- Connection of the remaining “healthy” sections with the intestines.
The intervention takes more than one hour, especially with carcinoma, when the greater and lesser omental bursa, tissue and lymph nodes must be removed.
Laparoscopic surgery is longer than in the open abdominal cavity, and technically much more complicated; in fact, this operation is the pinnacle of the professional art of an abdominal oncologist surgeon.
Postoperative period
In the postoperative period, the patient begins to understand how difficult it is to live after gastric resection. The wound on the abdominal wall is a burden, but every day it becomes less and more worrying because of the drainage left in the wound and the intestinal tube installed through the patient’s nose.
Drainage in the wound is required to control the condition of the abdominal cavity, where fluid can accumulate and blood will appear if bleeding occurs. Through drainage, the consistency of the gastrointestinal connection - anastomosis - is determined. The drainage is removed when the damaged tissue inside the abdominal cavity has healed safely.
With a significant decrease in the contractile activity of the intestine, intubation helps to free the intestinal tube from gases and, if necessary, from the resulting liquid; the probe is removed by the end of the week, when the function of the gastrointestinal anastomosis is improved and intestinal motility is restored.
Symptoms of operated stomach syndrome
Depending on the severity of the disease, dumping syndrome can be mild, moderate or severe.
Mild severity:
- Attacks occur 1-2 times a month due to errors in diet. They last for 15-30 minutes and go away on their own after giving up foods rich in carbohydrates and milk. Diarrhea is sometimes noted.
Moderate severity:
- Attacks 4-5 times a week lasting from 1 to 2 hours are accompanied by rapid heartbeat, increased blood pressure, diarrhea, decreased performance, and a decrease in body weight up to 10 kg.
Severe severity:
- Attacks lasting 3-4 hours after any meal, possibly with loss of consciousness, cachexia.
Complications of resection
Complications are not necessary, but are possible, especially in cancer patients weakened by the cancer process. Based on the time of development, all postoperative complications are divided into early and late.
Early complications arise shortly after surgery:
- According to the literature, failure of the gastrointestinal anastomosis occurs in 5% of operated patients; in cancer, it is caused by impaired hemostasis - all biochemical intracellular processes and decreased immunity due to malnutrition due to the disease; gastroscopy helps to identify this dangerous complication in a timely manner.
- Bleeding is very rare - less than 2%; early diagnosis is helped by installing drainage in the wound.
Another group of complications arises after some time and remains with the patient for a long period of varying intensity, complicating life after gastrectomy:
- Dumping syndrome is associated with a significant decrease in the volume of the gastric cavity, causing food to pass to the jejunum without delay, which causes an autonomic reaction with weakness up to loss of consciousness and vomiting due to the rapid distension of the intestine.
- Anastomositis is inflammation of the mucous membrane of the anastomosis, usually accompanied by pain and changes in appetite, but can occur without any symptoms, often detected during control gastroscopy, and can worsen in the fall or spring.
- Mucosal ulcers are more typical for chronic ulcers.
- Anemia develops due to impaired absorption of B vitamins.
UDC 616.33/.34-089:616-089.166-06-84
The work outlines modern principles of surgical treatment of patients and victims with suture failure in diseases and injuries of the gastrointestinal tract. Methods of surgical treatment of incompetent sutures of the gastrointestinal tract in complicated peptic ulcer disease, damage to the duodenum and small intestine, developed in the clinic, can improve the immediate and long-term results of surgical interventions and reduce postoperative mortality.
Surgical treatment of patients and affected with unsoundness suture at the diseases and injuries of the gastrointestinal tract
The paper presents the modern principles of surgical treatment of patients and affected with suture failure in diseases and injuries of the gastrointestinal tract. Developed at the clinic methods of surgical treatment of insolvency joints of the gastrointestinal tract in complicated peptic ulcer, duodenal lesions and small intestine can improve the immediate and long-term results of surgical interventions, to reduce postoperative mortality.
Suture failure in patients and victims with diseases and injuries of the gastrointestinal tract (GIT) is one of the most severe and dangerous complications in abdominal surgery [1-4]. Mortality in this pathology reaches 50-80% and is associated not only with biotic changes in tissues, but also with the traumatic nature of repeated operations, the number of which sometimes reaches more than 5 [5-7]. The sad statistics are also due to the fact that the issues of choosing the optimal options for operations that help prevent early postoperative complications have not been fully resolved [8-10]. In our opinion, such a high mortality rate is due to the mistakes surgeons make when choosing the method and volume of operations, which ultimately leads to the development of early postoperative complications, their late diagnosis and ineffective treatment [11].
Research objective:
improving the results of surgical treatment of patients and victims with diseases and injuries of the gastrointestinal tract by improving existing and developing new methods for the prevention and treatment of patients with suture failure.
Materials and methods:
for the period 1992-2011. In the surgical department of the Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, 208 patients and victims with suture failure due to diseases and injuries of the gastrointestinal tract were treated (Table 1).
Table 1.
Patients with leaky gastrointestinal sutures of the main group and comparison group
| Insolvency of gastrointestinal sutures | Main group | Comparison group |
| Failure of sutures after suturing the perforated hole of a gastric ulcer, 12 p.c. | 25 | 7 |
| Failure of enterojejunostomy sutures | 20 | 38 |
| Failure of stump sutures 12 p.c. | 17 | 16 |
| Failure of enterocoloanastomosis sutures | 8 | 14 |
| Failure of gastroduodenoanastomosis sutures | 7 | 14 |
| Failure of sutures after suturing acute ulcers of the small intestine | 5 | 17 |
| Failure of sutures after suturing injury 12 p.c. | 4 | 9 |
| Failure of gastrojejunostomy sutures | 4 | 3 |
| Total | 90 | 118 |
The main group consisted of 90 patients and victims with incompetent gastrointestinal sutures, operated on in the clinic from 2002 to 2011. In the main group, in addition to traditional methods of surgical treatment, 35 patients (38.9%) underwent surgical procedures using methods developed at the clinic. Of these, 12 patients (13.3%) underwent surgical interventions for complicated peptic ulcer disease and 23 patients (25.6%) for incompetent sutures of the intestinal anastomosis. There were 62 (68.9) men, 28 (31.1) women, the age of the patients ranged from 18 to 80 years. In 88 patients (97.7%), relaparotomy was performed for emergency reasons.
The comparison group included 118 patients and victims who were operated on in the clinic with similar complications during the period from 1992 to 2001. In 116 patients (98.3), repeated surgical interventions were performed for emergency indications. There were 77 (65.3) men, 41 (31.1) women, the age of the patients ranged from 16 to 86 years.
Diseases and injuries in which leakage of gastrointestinal sutures was observed in the main group and comparison group are presented in Tables 2, 3.
Table 2.
Failure of gastrointestinal sutures in patients and victims in the main group
| Diseases and injuries of the gastrointestinal tract | Suture failure Gastrointestinal tract |
| Complicated gastric ulcer and 12 p.c. | 53 (58,9%) |
| Acute intestinal obstruction with necrosis of the small intestine | 9 (10,0%) |
| Injuries of the 12th p.k., small and large intestine | 7 (7,8%) |
| Thrombosis of mesenteric vessels with necrosis of the small intestine | 5 (5,5%) |
| Strangulated hernia of the anterior abdominal wall with necrosis of the small intestine | 4 (4,5%) |
| Perforation of acute ulcers of the small intestine | 4 (4,5%) |
| Abdominal abscess with small bowel necrosis | 3 (3,3%) |
| Colon tumors | 2 (2,2%) |
| Ileostomy | 1 (1,1%) |
| Failure of sutures after suturing perforations of acute ulcers of the small intestine | 1 (1,1%) |
| Failure of sutures after suturing perforations of acute colon ulcers | 1 (1,1%) |
Table 3.
Failure of gastrointestinal sutures in patients and victims in the comparison group
| Diseases and injuries of the gastrointestinal tract | Insolvency of gastrointestinal sutures |
| Complicated gastric ulcer and 12 p.c. | 40 (33,9%) |
| Acute intestinal obstruction with necrosis of the small intestine | 19 (16,1%) |
| Strangulated hernia of the anterior abdominal wall with necrosis of the small intestine | 17 (14,4%) |
| Perforation of acute ulcers of the small intestine | 15 (12,7%) |
| Thrombosis of mesenteric vessels with necrosis of the small intestine | 13 (11,0%) |
| Injuries of the 12th p.k., small and large intestine | 10 (8,5%) |
| Abdominal abscess with small bowel necrosis | 4 (3,4%) |
The vast majority of patients with incompetent gastrointestinal sutures in the main group were patients with complicated peptic ulcer of the stomach and duodenum (12 p.c.) - 53 (58.9%). In patients with failure of the sutures of the sutured perforation, the main reason for the development of complications in 21 (84.0%) cases was errors made when choosing the method of primary surgery. Thus, in 14 patients, relaparotomy revealed the presence of pyloroduodenal stenosis, in 7 patients there was perforation of callous and penetrating ulcers, which initially suggested gastric resection. In addition, 7 patients did not receive adequate preoperative preparation, even if they had hypoproteinemia, fluid and electrolyte disturbances, and concomitant diseases.
When the sutures of the sutured perforated hole failed in large callous, stenotic and penetrating ulcers, gastric resection was performed in 16 patients. Repeated suturing of the perforated hole in combination with bilateral subphrenic truncal vagotomy and gastroenterostomy in patients with callous and penetrating ulcers was performed in 5 cases, due to the presence of widespread peritonitis and a high risk of radical surgery. Suturing of the perforated hole during relaparotomy without excision of the ulcer and drainage operations was performed in 4 patients.
Thus, with perforation of stenotic, penetrating, bleeding gastric ulcers, 12 p.c. The method of choice is primary gastrectomy or suturing of the perforation with bilateral subdiaphragmatic truncal vagotomy, gastroenterostomy. Suturing the perforated hole, excision of the perforated ulcer followed by pyloroplasty and vagotomy are indicated for perforation of simple gastric ulcers and 12 p.c.
If the sutures of the stump fail, 12 p.c. treatment tactics were determined by its form. In patients with an infiltrative form of failure of the stump sutures, 12 p.c. conservative therapy was carried out, consisting of decompression of the stump 12 p.c. through a probe installed during endoscopy, antibacterial therapy, correction of water and electrolyte balance, administration of protein drugs, protease inhibitors. In the case of the primary fistula form of incompetence of the duodenal stump, enteral nutrition was provided, the skin in the area of the fistula was protected by multi-layer application of medical glue, zinc ointment or paste, and irradiation with infrared laser radiation. Duodenal contents coming from the abdominal drains, after filtering, were returned through a nasointestinal tube.
Peritoneal form of failure of stump sutures 12 p.c. is an absolute indication for emergency surgery. The purpose of the operation is to eliminate the entry of duodenal contents, decompress 12 p.k., sanitation and drainage of the abdominal cavity, delineate the free abdominal cavity from possible intestinal contents.
An important point when suturing a stump defect 12 p.c. was an additional mobilization of the intestine with the intersection of the Clermont ligament, fixing the lower horizontal part of the 12 p.c., which made it possible to eliminate tension along the line of the stitched tissues, while maintaining adequate blood supply. It is mandatory to insert a nasointestinal tube into the outlet loop for the purpose of nutritional support. In cases of large defects in the stump, 12 p.c. and the impossibility of covering its lumen, in 5 patients a duodenojejunostomy was performed on a long loop with an interintestinal anastomosis (patent No. 2184493, 2002).
In case of peritoneal form of failure of the sutures of the gastrointestinal anastomosis, it is possible to suture the defect with strengthening the suture line with a strand of omentum, as well as using the TachoComb wound covering. In 2 patients with a peritoneal form of gastroduodenoanastomosis failure, with a significant size of the defect and the inability to ensure its tightness, B-I was transferred to Roux, while forming, after gastroenterostomy, an end-to-side duodenojejunostomy according to the method developed in our clinic (patent No. 2325853 , 2008). It is mandatory to insert a nasointestinal tube into the outlet loop during the operation for the purpose of enteral nutrition.
In the program for the prevention of insolvency of gastrointestinal sutures in patients and victims with diseases and injuries, 12 p.c. and small intestine, the choice of the optimal option for primary surgical intervention and timely diagnosis of complications are crucial. In case of injury to the 12th p.c., in order to prevent suture failure, it is necessary to mobilize the 12th p.c. during surgery. according to Kocher-Clermont, suturing wounds in the transverse direction with atraumatic suture material. If more than 1/3 of the intestinal circumference is damaged, it is necessary to apply duodenojejunostomy with Brown's anastomosis or turn off 12 p.c. from the passage.
Issues of preventing the failure of gastrointestinal sutures in acute intestinal obstruction, acute ulcers of the small intestine complicated by perforation, thrombosis of mesenteric vessels, hernia repair for strangulated hernias of the abdominal wall are complex and come down mainly to drainage of the abdominal cavity and closed intubation of the intestine, after suturing its defect or resection of the affected part organ. In acute adhesive intestinal obstruction, hernia repair for strangulated postoperative ventral hernias, an important point in the operation is the stage of entry into the abdominal cavity, during which damage to the intestine is possible, followed by the probable development of suture failure. To avoid damage to the intestine, it is necessary to perform laparotomy extremely carefully, enter the abdominal cavity in the part where there are no adhesions, and use the technique of tissue differentiation by infiltrating them with saline solution or novocaine, thus performing hydraulic preparation. Dissection of adhesions should be carried out carefully, sequentially, and all deserated areas should be sutured using atraumatic suture material.
Perforations or damage to the small intestine must be sutured with a double-row suture with atraumatic suture material, after first excising the crushed edges of the wounds. In case of closely spaced perforations, ruptures of the intestine, damage to more than 2/3 of its circumference, complete transverse rupture and separation of the intestine from the mesentery of more than 5 cm, resection of the small intestine with a side-to-side anastomosis and nasointestinal intubation with a double-lumen probe are indicated. If there is a “problematic” blood supply to the intestine, an important point in preventing the failure of the sutures of the intestinal anastomosis is to establish the boundaries of its viability and determine the required volume of intestinal resection.
In order to prevent suture failure in diseases of the abdominal organs, widespread peritonitis, severe condition of patients, water and electrolyte disturbances, intestinal resection must be completed by removing the stoma, except in situations where large losses of intestinal contents along the stoma are possible in the postoperative period with extensive resections. If there is uncertainty about the reliability of the interintestinal anastomosis, it is possible to perform a Meidl jejunostomy. The advantages of Meidl jejunostomy include early enteral nutrition and the return of intestinal contents through the stoma.
Surgical interventions for acute intestinal obstruction must be completed with nasointestinal intubation with a double-lumen probe, followed by multiple enterosorption in the early postoperative period. In case of early postoperative adhesive intestinal obstruction, passing a probe through a gastrostomy tube has advantages, when, unlike nasointestinal intubation, the probe can remain in the gastrointestinal tract for up to two weeks or more.
Based on the results of our experimental studies, a new method for preventing enteroenteroanastomosis suture failure has been developed and introduced into clinical practice (patent No. 2445022, 2012, “Method for preventing enteroenteroanastomosis suture failure”). The essence of the method is extraperitonealization of the interintestinal anastomosis. After re- or laparotomy, revision and sanitation of the abdominal cavity, resection of the necrotic part of the intestine, a side-to-side interintestinal anastomosis is formed or the defect in the previously formed interintestinal anastomosis is sutured. Subsequently, all layers of the abdominal wall are dissected in the place where the interintestinal anastomosis can most freely be brought and placed. A cavity is formed in the abdominal wall, the walls of which are the parietal peritoneum, muscles, and subcutaneous fatty tissue. An interintestinal anastomosis is placed into the cavity thus formed, sealing and fixing it to the parietal peritoneum and forming “spurs” of the afferent and efferent loops of the intestine. The skin wound is sutured with rare sutures with mandatory drainage of the subcutaneous tissue. In the event of failure of the sutures of the interintestinal anastomosis, an external intestinal fistula is formed, which subsequently often closes on its own. This technique achieves the main goal of preventing the development of widespread peritonitis and the need for repeated surgery. All this ultimately leads to improved immediate and long-term results of surgical interventions for diseases and injuries of the small intestine.
An important point in the prevention and treatment of suture failure in small intestinal injuries is drainage of the lateral sections of the abdominal cavity and small pelvis. In addition, in case of damage to 12 p.c. We widely drain the retroperitoneal space with tubes and glove drains through a lumbotomy approach.
In case of trauma to the colon, it should be resected with removal of the adductor colon in the form of a single-barrel colostomy. In case of small wounds of the intestine, the serious condition of the victim, widespread peritonitis, the damaged area of the colon can be removed in the form of a double-barreled colostomy, and it can also be sutured with retrograde intubation of the colon.
results
In patients with failure of the sutures of the sutured perforated hole with a perforated ulcer, 12 p.c. In 13 cases, resection of 2/3 of the stomach was performed according to Brown. In 3 patients, due to the presence of a large callous ulcer of the subbulb section 12 p.k., the impossibility of forming a direct gastroduodenoanastomosis, suturing the stump 12 p.k. Gastric resection was performed using a technique we developed, the main difference of which is the application of duodenojejunostomy. In 5 cases, repeated suturing of the perforation was combined with bilateral subphrenic truncal vagotomy and Welfler-Brown gastroenterostomy. In 4 patients, the perforation was again sutured and covered with TachoComb wound dressing, prolonged gastric decompression and 12 p.c. In all patients, the operation included thorough sanitation and adequate drainage of the abdominal cavity. Early postoperative complications were observed in 5 patients. In 2 cases, intra-abdominal bleeding developed, and therefore the patients underwent relaparotomy. One patient developed gastric bleeding from acute gastric ulcers on the 3rd day after surgery. Endoscopic hemostasis and antiulcer therapy helped stop bleeding and heal ulcers. One patient developed early postoperative adhesive intestinal obstruction; relaparotomy and viscerolysis with nasointestinal intubation were performed. Subcutaneous eventeration occurred in 1 patient. Death occurred in 7 patients (28.0%).
In 2 patients with an infiltrative form of stump failure, 12 p.c. On days 7-9, an infiltrate formed in the right hypochondrium. Both patients were operated on on the 8th day due to the formation of a subhepatic abscess; one of them underwent drainage of the subhepatic abscess under ultrasound guidance. In 3 patients, a primary fistula form of incompetence of the stump 12 p.c. developed. The fistula formed on the 4th–5th day and was manifested by the leakage of duodenal contents through the drains. Given the absence of widespread peritonitis, all patients underwent conservative therapy. One patient was re-operated due to large drainage losses. 12 patients with peritoneal form of stump failure 12 p.c. relaparotomy was performed. In 5 patients with the peritoneal form of incompetence of the stump sutures, 12 p.c. During the operation, it was possible to isolate the stump of 12 p.c. from the infiltrate and suturing the stump defect and draining it with a transnasal probe. In 3 patients after gastric resection according to Brown, with a dense infiltrate in the subhepatic space, a small defect in the stump, with a small amount of duodenal discharge, we limited ourselves to draining the stump area with passive and active drains, and placing delimiting glove drains. In one patient with a primary fistula form of failure of the stump sutures 12 p.k., with more than 1.5 liters of drainage discharge and in 4 patients with a peritoneal form of failure, with a significant size of the defect and the inability to ensure tightness, a duodenojejunostomy was formed on a long loop with interintestinal anastomosis. Early postoperative complications were observed in 3 patients. In 2 patients, early acute adhesive intestinal obstruction developed; relaparotomy and viscerolysis were performed. In 1 patient, an abdominal infiltrate formed in the postoperative period; after complex conservative therapy, the infiltrate resolved. Death occurred in 3 patients (17.6%).
If the sutures of the gastroduodenoanastomosis in the main group failed, the anastomosis was disconnected in patients, followed by its transfer to Roux, due to a large defect in the anastomosis. 4 patients underwent reconstructive surgery using a technique we developed, the essence of which is the formation of a gastroenteroanastomosis on a long Roux-en-Y loop with an end-to-side duodenojejunostomy. Death occurred in 3 patients (42.9%),
In 4 cases of gastroenteroanastomosis suture failure, the defect was sutured with strengthening of the suture line with a strand of omentum (2 patients), as well as using TachoComb wound dressing. 1 patient died, mortality rate - 25%.
In the main group, 23 patients underwent extraperitonealization of the interintestinal anastomosis; in 3 cases (13.0%), the anastomotic sutures failed with the formation of an intestinal fistula, which closed 3 weeks after conservative therapy. There were 2 deaths (8.6%), both patients died from progressive multiple organ failure and severe concomitant pathology.
Mortality in the main group was 27.8%, in the comparison group - 35.6%.
conclusions
1. The introduction of new methods of surgical treatment that we have developed for patients and victims with suture failure in complicated peptic ulcer disease, injuries of the 12 p.c., small intestine allowed us to improve the results of surgical interventions and reduce postoperative mortality by 7.8%.
2. If the sutures of the sutured perforation fail, gastrectomy is indicated in patients with large callous, stenotic and penetrating ulcers. If it is impossible to form a stump, 12 p.c. Gastric resection should be performed according to the methods we have developed.
3. If it is impossible to suturing the stump defect, 12 p.c. or gastroduodenoanastomosis in patients with the peritoneal form of suture failure, reconstructive operations with the formation of duodenojejunostomy according to the methods developed by us are indicated.
4. When extraperitonealization of enteroenteroanastomosis occurs, the likelihood of developing insolvency of the sutures of the interintestinal anastomosis is significantly reduced due to its reliable sealing in the abdominal wall. In the event of failure of the sutures of the interintestinal anastomosis, an intestinal fistula is formed, which subsequently often closes on its own. This method of operation helps prevent widespread peritonitis and the need for repeated intervention.
D.M. Krasilnikov, Ya.Yu. Nikolaev, M.M. Minnullin
Kazan State Medical University
Krasilnikov Dmitry Mikhailovich - Doctor of Medical Sciences, Professor, Head of the Department of Surgical Diseases No. 1
Literature:
1. Agaev E.K. Failure of sutures of intestinal anastomoses in patients after emergency and urgent resection of the intestine // Surgery. - 2012. - No. 1. - P. 34-37.
2. Gorsky V.A., Shurkalin B.K., Faller A.P. Problems of reliability of the intestinal suture in peritonitis and intestinal obstruction // Difficult patient. - 2005. - No. 4. - P. 23-27.
3. Hsu TC Inferior mesenteric artery stump pressure is an unreliable predictor of the outcome of colorectale anastomosis // Int. J. Colorect. Dis. - 2007. - Vol. 22, No. 12. - P. 1481-1482.
4. Lipska MA, Bissett JP, Parry BR et al. Anastomotic leakage after lover gastrointestinal anastomosis: men are ata higher risk // Aust. NZJ Surg. - 2006. - Vol. 76, No. 7. - P. 579-585.
5. Galimov O.V., Gilmanov A.Zh., Khanov O.V. and others. Prevention of anastomotic failure of hollow organs of the gastrointestinal tract // Surgery. - 2008. - No. 10. P. 27-29.
6. Gulov M.K. Prevention of failure of stump sutures 12 p.c. after gastrectomy // Experimental and clinical gastroenterology. - M.: Anacharsis, 2005. - No. 2. - P. 56-58.
7. Kim KW, Choi BI, Han JK Postoperative anatomical and pathological findings at Ct following gastrectomy // Radiographics. - 2002. - Vol. 22, No. 3. - P. 323-326.
8. Dibirov M.D., Briskin B.S., Rodionov I.E. and others. The use of surgical glue “Bioclay-Lab” for the prevention of anastomotic leakage on the organs of the gastrointestinal tract // Annals of Surgery. - 2008. - No. 2. - P. 31-34.
9. Krasilnikov D.M., Nikolaev Ya.Yu., Minnullin M.M. Prevention of failure of enteroenteroanastomosis sutures // Creative surgery and oncology. - 2012. - No. 1. - P. 38-39.
10. Krasilnikov D.M., Nikolaev Ya.Yu., Minnullin M.M. and others. Experimental analysis of the causes of failure of the sutures of the gastrointestinal tract in isolated damage to the small intestine and with concomitant acute pancreatitis // Electr. scientific-practical magazine "Creative Oncology and Surgery". - 2011. - No. 1.
11. Krasilnikov D.M., Minnullin M.M., Nikolaev Ya.Yu. Diagnosis and complex treatment of gastrointestinal tract suture failure in patients with gastric and duodenal ulcers // Creative surgery and oncology. - 2012. - No. 3. - P. 49-55.
Prognosis after gastrectomy
Medical statistics do not know how long people live after gastrectomy, because life expectancy depends on the disease that caused the operation.
With benign processes and peptic ulcer disease, the prognosis is quite favorable and, as a rule, does not affect life expectancy.
For cancer, the prognosis depends on the stage of spread of the malignant process at the time of its detection and the degree of aggressiveness of the tumor, so 80 out of a hundred people with stage 1 live 5 years after the intervention, 60 patients with stage 2 and no more than 35 patients admitted for treatment with stage 3 carcinoma .
A cancer patient arrives on the operating table in not the best condition, when there is no question of balance in the body: weakened by poor nutrition, not receiving a sufficient complex of necessary substances, immunity undermined by cancer, the nervous system torn by the unknown. Any operation, especially on the organs of the gastrointestinal tract, disturbs the balance in the body; the professionals at our clinic can quickly and effectively restore the balance.
| More information about the treatment of stomach cancer at Euroonco: | |
| Treatment of stomach cancer | |
| Oncologist-gastroenterologist | RUB 5,100 |
| Chemotherapy appointment | RUB 6,900 |
| Emergency oncology care | from 12,100 rub. |
| Radiologist consultation | RUB 11,500 |
Book a consultation 24 hours a day
+7+7+78
Bibliography
- Davydov M.I., Turkin I.N., Davydov M.M./Encyclopedia of surgery for gastric cancer/Moscow: EKSMO; 2011.
- Davydov M.I., Turkin I.N., Polotsky B.E./Modern surgery of gastric cancer: from D2 to D3//Proceedings of the IX Russian Oncological Congress; Moscow; 2005.
- Davydov M.I., Ter-Ovanesov M.D., Stilidi I.S./ Surgical treatment of cancer of the proximal stomach. Materials of the V Annual Russian Oncological Conference//Moscow: 2002.
- Chernousov A.F., Khorobrykh T.V., Vychuzhanin D.V./Results of surgical treatment of patients with cardioesophageal cancer // Sechenovsky Bulletin; 2011; No. 1
- Orsenigo E., Tomajer v. ,Palo SD et al. /Impact of age on postoperative outcomes in 1118 gastric cancer patients undergoing surgical treatment // Gastric Cancer; 2007; v. 10.-P.
- Karanicolas PJ, Elkin E.V., Lindsay MJ et al.//Staging Laparoscopy in the Management of Gastric Cancer: A Population-Based Analysis /J Am Coll Surg; 2011; v. 213.
Menu examples
The sample menus at the end of this material consist of 6 small meals, and you should drink 4 ounces (120 ml) of fluid with each meal and 8 ounces (240 ml) between meals. Soup is also considered a liquid.
It is often helpful to consume liquids separately from solid foods. Try to drink fluids between meals rather than during meals.
Many foods on this menu contain sugar. Use sugar-free or “light” yogurt instead of regular yogurt, limit your intake of fruit juices and dilute them with water if you have:
- do you have diabetes?
- high blood sugar;
- operated stomach syndrome.
Foods marked with an asterisk (*) contain lactose. If you are lactose intolerant, try drinking lactose-free milk (such as Lactaid) instead of regular milk. You can also take lactase tablets or drops to help digest dairy products. Instead of regular milk, you can also try using plant-based dairy products, such as almond or soy milk without added sugar.
| Meal time | Menu example 1 | Menu example 2 |
| Breakfast 7:30 |
|
|
| 9:00 |
|
|
| Snack 10:00 |
|
|
| 11:30 |
|
|
| Lunch 12:30 |
|
|
| 14:00 |
|
|
| Snack 15:00 |
|
|
| 16:30 |
|
|
| Dinner 17:30 |
|
|
| 19:00 |
|
|
| Snack 20:00 |
|
|
| 21:30 |
|
|
to come back to the beginning