Esophageal candidiasis is a mycotic infection caused by fungi of the genus Candida. The disease manifests itself as difficulty swallowing, chest pain and discomfort. With the long-term existence of candidiasis, weight loss and severe vitamin deficiencies occur. The basis for diagnosing a fungal infection is examination of the esophagus during endoscopy, followed by morphological analysis of biopsy specimens to identify pathogen particles. Additionally, microbiological seeding of the biomaterial is carried out. To treat esophageal candidiasis, systemic antifungal drugs of different chemical structures are used.
General information
Esophageal candidiasis (candidal esophagitis) is considered an opportunistic infection. Among general patients, the incidence of the disease is 1-2%; in the presence of diabetes mellitus, mycosis occurs much more often - in 5-10% of cases. In patients with HIV infection and AIDS, the prevalence of fungal infection of the esophagus reaches 30%. The incidence of candidiasis among older people is 2 times higher than the average in the population, and in old age (after 75 years) it is 6 times higher. The infection sometimes occurs in children against the background of primary immunodeficiencies.
Candidiasis of the esophagus
Answers to popular questions
Is thrush contagious?
Yes, it's contagious. Often young children become infected from their mothers. To avoid this, it is recommended to cure the mother’s candidiasis, as well as treat nipples and household items (antiseptically).
I have candidiasis - does this mean I have diabetes?
No, it's completely optional. But, if you often encounter thrush, it would be a good idea to take a blood sugar test. With diabetes, the risk of recurrent candidiasis is higher.
Candidiasis is for life?
Absolutely not! If all doctor's prescriptions are followed, candidiasis can be successfully treated. It is worth paying attention to prevention to prevent relapse of the disease.
Causes
The causative agents of infectious diseases of the esophagus are fungi of the genus Candida. In total, there are more than 150 species of Candida fungi, but in 60-90% of cases the pathology is caused by C. albicans. With immunosuppression, the role of other species increases: C. glablata, C. kefir, C. lucitanies and C. krusei. Microorganisms in natural conditions are in the form of blastomycetes or pseudomycelium. A number of predisposing factors contribute to the development of candidiasis:
- Immunodeficiencies. Damage to the mucous membranes of the digestive tract by Candida fungi is one of the markers of progressive HIV infection. High incidence is observed in primary genetically determined immunodeficiencies: DiGeorge syndrome, Bruton syndrome, Wiskott-Aldrich disease, etc.
- Drug immunosuppression. The incidence of candidiasis increases with prolonged treatment with corticosteroids, which suppress the activity of the immune system. Radiation and chemotherapy for cancer patients, which disrupts local and general immune defense factors, has a negative impact.
- Endocrine diseases. The likelihood of mycosis increases in those suffering from diabetes mellitus, autoimmune polyendocrine syndrome, and hypothyroidism. Antifungal resistance decreases in obesity and other manifestations of metabolic syndrome.
- Local factors. Local causes of the mycotic process include chronic inflammatory and atrophic changes in the esophageal wall, xerostomia, and degenerative-destructive disorders in the oral cavity. The pathology is twice as common in those who use removable dentures.
Risk factors
Risk factors for the development of esophageal candidiasis: exhaustion, vitamin deficiencies, chronic somatic diseases accompanied by asthenia. The likelihood of mycosis increases after organ transplantation operations.
The wide prevalence of candidiasis in older people is associated with involutive decline of immune functions, microcirculation disorders due to atherosclerosis, and atrophy of the mucous layer of the esophagus. Polypharmacy, namely the uncontrolled use of antibiotics, hormones and antisecretory drugs, plays a large role in the formation of candidiasis.
Publications in the media
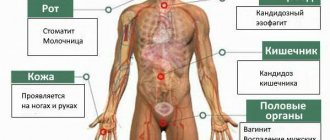
Candidiasis is an opportunistic mycosis that occurs with lesions of the mucous membranes and skin; in patients with severe immunodeficiency, disseminated forms are possible, most often affecting the lungs and gastrointestinal tract.
Etiology. The causative agents are yeast-like fungi of the genus Candida. 90% of lesions are caused by Candida albicans (which also includes C. stellatoidea). Other pathogens - C. tropicalis, C. krusei, C. lusitaniae, C. parapsilosis, C. kefyr (formerly C. pseudotropicalis), C. guillermondii, C. (Torulopsis) glabrata and very rarely - C. rugosa, C. utilis , C. lipolytica, C. zeylanoides.
Risk factors • Hematogenous disseminated candidiasis •• Neutropenia •• Antibiotic therapy •• Long-term catheterization of blood vessels •• Previous hemodialysis • Mucocutaneous candidiasis •• Immunodeficiency conditions •• Antibiotic therapy •• Douching and chemical irritation of the vagina •• Vaginitis •• Wearing dentures • • Long-term use of GCs •• Taking oral contraceptives •• Hyperglycemia.
Epidemiology. Candida is widespread in nature, mainly on plant substrates, various household items, especially children's toys. Candida albicans is normally present in the mouth, gastrointestinal tract, vagina and sometimes on the skin. Candidiasis is registered only in humans. The incidence increased significantly with the introduction of antibiotics and is currently progressing. Candida is one of the most common causative agents of opportunistic mycoses. Any immunodeficiency state and disruption of normal microbial cenosis lead to the onset of the disease. The possibility of transmission of the pathogen through household contacts has not been determined, but children become infected when passing through the birth canal or during breastfeeding. Urogenital candidiasis is transmitted sexually.
Pathogenesis. With disseminated lesions, the formation of foci of necrosis and neutrophilic inflammatory infiltration is noted. The development of candidiasis is facilitated by damage to the skin, increased sweating, and maceration. Dry, intact skin is resistant to Candida albicans. Excessive growth of Candida albicans is facilitated by disturbances in the microbial cenosis of the body caused by inadequate use of broad-spectrum antibiotics or changes in the microenvironment. The development of candidiasis is facilitated by metabolic and hormonal disorders (for example, diabetes, pregnancy, and the use of oral contraceptives). Immunodeficiency states and the use of immunosuppressants (for example, GCs) can cause fulminant forms and chronic candidiasis of the skin and mucous membranes.
Genetic aspects. Candidiasis is a companion to numerous inherited immunodeficiencies. Examples: • Familial chronic candidiasis (114580, Â) is constantly accompanied by viral infections, alopecia, tooth loss are characteristic • Familial chronic mucocutaneous candidiasis (*212050, r) affects the skin, nails, characterized by constant thrush, iron deficiency • Autoimmune polyglandular type syndrome I • Hyperimmunoglobulinemia syndrome E (147060, Â) with a defect in the chemotaxis of neutrophil leukocytes • Jobe's syndrome.
Clinical picture
• Superficial candidiasis develops in areas of the skin with relatively high temperature and humidity, with maceration of the skin associated with regular contact with water •• Candidal intertrigo is observed with diaper rash: erythematous or vesiculopustular rashes with maceration (usually in the area of large skin folds in children ), which leads to the development of erosions; whitish necrotic areas of the epithelium with ulcerated edges •• Diaper dermatitis is most often caused by Candida albicans: scaly rash or vesiculopustular rash accompanied by inflammation and intense itching •• Paronychia and onychia are usually caused by Candida albicans; most often, lesions are observed during maceration of the hands and feet caused by constant contact with water (in dishwashers and laundresses); characterized by thickening and discoloration of the nail plates, less often - nail loss.
• Mucocutaneous candidiasis is most often observed in the oral cavity and vagina. • Oral candidiasis (thrush) is a characteristic consequence of taking broad-spectrum antibiotics or immunodeficiency states. Typical manifestations are white or yellowish plaques on the surface of the mucous membrane; they are painless and do not merge. The lesions are often associated with diffuse erythema, thick dark brown deposits, deep fissures, and increased dryness of the mucous membrane. •• Vulvovaginal candidiasis caused by Candida albicans is widespread among women taking oral or intrauterine contraceptives, or who are in the third trimester of pregnancy (the condition is indirect). immunosuppressive effects of high concentrations of progesterone and serum a-globulin-related factor). It may be asymptomatic or cause intense itching or discomfort. It manifests itself as discharge such as leucorrhoea or films of varying thickness in the form of “pressed cheese”. Reddish spots are observed on the vaginal mucosa, labia, vulva and other areas of the perineum • Chronic mucocutaneous candidiasis is a rare pathology mediated by defects in T-lymphocytes; possible damage to the skin (including the scalp), mucous membranes (cheilitis, esophagitis), onychia and paronychia. In the most severe cases, granulomatous cutaneous candidiasis is observed with the appearance of infiltrates with unclear contours on the skin and nails, which are later covered with serous-sanguinary crusts, permeated with mycelium.
• Disseminated candidiasis (candidal sepsis, systemic candidiasis) is characterized by a severe course, high fever of the wrong type and damage to various organs (lungs, kidneys, brain, gastrointestinal tract, etc.). Dissemination of superficial candidiasis is rarely observed •• Candidal endocarditis. Symptoms: high body temperature, pain in the heart, heart murmurs, enlarged spleen, anemia •• Pulmonary lesions are accompanied by the development of infiltrates, including pseudomycelium of the pathogen, sometimes it grows into blood vessels. Symptoms: severe cough, initially dry, then with a small amount of viscous mucopurulent sputum, sometimes streaked with blood. X-ray infiltrates are more often detected in the lower lobes, disintegration with the formation of cavities and involvement of the pleura in the process is often observed •• Candidal septicemia is similar to sepsis of other etiologies •• Eye lesions: candidal retinitis and candidal panophthalmitis •• Candidal meningitis •• With candidiasis of the gastrointestinal tract, pain is noted in abdomen, intestinal bloating, diarrhea with blood in the stool •• Hepatic candidiasis is a combined granulomatous lesion of the liver and spleen with invasive growth of Candida albicans in people with immunodeficiency conditions. The main clinical sign is fever. Signs of oropharyngeal candidiasis are identified; pain or tenderness is possible on palpation in the right hypochondrium. Changes in liver function tests: moderate increase in bilirubin content and enzyme activity.
Diagnosis • Disseminated candidiasis •• Isolation of the pathogen from the blood (cultures from lysates or centrifugates are more preferable), cerebrospinal fluid, pericardial fluid. The diagnosis is more likely when the pathogen is isolated from several areas of the body •• If isolation results are negative, biopsy or aspiration of samples from the lesions •• Laparotomy or laparoscopy for liver candidiasis: small white nodules are found, not exceeding 5 mm in diameter • Mucocutaneous candidiasis • • Microscopy of clinical material treated with 10% KOH solution or Gram-stained (Gram-positive yeast cells are detected) •• Isolation of the pathogen is carried out by inoculation on conventional mycological media or blood agar •• X-ray with barium sulfate for candidal esophagitis: “cobblestone” syndrome is detected » and, less commonly, a fistula or dilatation of the esophagus (due to denervation) •• For esophagitis - endoscopic biopsy. The detection of thrush and dysphagia in HIV-infected people with a decrease in the severity of manifestations when taking antifungal agents allows us to establish a preliminary diagnosis of candidal esophagitis.
Differential diagnosis • Hematogenous disseminated candidiasis is differentiated from various cryptogenic bacterial infections, as well as from opportunistic infections in patients with neutropenia • Mucocutaneous candidiasis is differentiated from hairy leukoplakia and lesions caused by yeast or other yeast-like fungi.
TREATMENT
Mode • For disseminated candidiasis - inpatient • For mucocutaneous candidiasis - outpatient.
Management tactics • Disseminated candidiasis •• Fluid replacement and correction of electrolyte balance •• In severe lesions - support of hemodynamics and respiratory function •• In patients receiving daily amphotericin B, blood, serum electrolyte and creatinine levels should be examined at least twice a week. When isolating a blood culture, blood cultures must be repeated until a negative result appears • Examination of children and patients with severe immunodeficiency at each visit to the doctor with an appropriate physical examination and collection of a detailed medical history.
Drugs of choice
• For disseminated candidiasis •• Fluconazole. 400 mg IV on the first day, then 200 mg/day for 1 week, then at the same dose IV or orally for at least 2 weeks after clinical recovery and normalization of bacteriological parameters. For hematogenous disseminated candidiasis, the drug is as effective as amphotericin B, but less toxic for patients without neutropenia, HIV infection and severe immunosuppression after organ transplantation •• Amphotericin B is an alternative drug for hematogenous disseminated candidiasis and the drug of choice for patients with neutropenia and immunosuppression . Start with a test dose of 1 mg, then it is gradually increased to the therapeutic dose (0.3–0.7 mg/kg/day). Sometimes the entire therapeutic dose is administered after a test dose, for example in critically ill patients. The duration of treatment depends on the patient's condition and the form of hematogenous disseminated candidiasis. Treatment is usually continued for 2–10 weeks. The total dose of the drug per course of treatment is 0.2–2.0 g.
• For mucocutaneous candidiasis •• For vulvovaginal candidiasis ••• Miconazole - daily before bedtime intravaginally in the form of a 2% cream or suppository of 100 mg (for 7 days) ••• Clotrimazole daily before bedtime intravaginally in the form of a suppository of 100 mg for 6–7 days or 200 mg for 3 days, or in the form of 1% cream for 6–7 days ••• Nystatin in the form of cream, 100,000 units/g 1 r/day or intravaginal tablets, 100,000 U/g 2 times a day for 7 days ••• Fluconazole orally 150 mg 1 time / day twice with an interval of 7 days (or one tablet 450 mg once) •• For candidiasis of the oral cavity and pharynx ••• Clotrimazole: tablet (lozenge) 10 mg, keep in mouth for 20 minutes, 5 times a day for 7–14 days (48 hours after the disappearance of thrush) ••• Lozenges with nystatin, 1–2 pieces, 4–5 times a day for 7–14 day (48 hours after the disappearance of thrush) ••• Nystatin suspension for oral administration, 5–10 ml, before swallowing, rinse your mouth for 20 minutes 4–5 times a day (treatment), 2–5 times a day (prevention of relapse) .
• For candidal esophagitis • Ketoconazole orally 200–400 mg 4 times/day for 14–21 days •• or fluconazole orally: first dose 200 mg, then 100 mg 4 times/day for 10–21 days.
• For gastrointestinal candidiasis - fluconazole 200 mg orally 4 times a day for 14–21 days.
Alternative drugs • For disseminated candidiasis •• Fluconazole - for infection caused by Candida lustaniae, resistant to amphotericin B •• Amphotericin B - for infection with Candida krusei, resistant to fluconazole •• Other synthetic antifungals - imidazole and triazole derivatives, depending on their activity and safety • For mucocutaneous candidiasis •• For vulvovaginal candidiasis ••• Fluconazole 150 mg 1 time per day twice with an interval of 7 days ••• Any antifungal creams or suppositories to prevent relapse can be used every month a few days before menstruation — for women at risk (with an IUD, as well as for those taking oral contraceptives, antibiotics) •• For candidiasis of the oral cavity and pharynx ••• Ketoconazole 200–400 mg orally 4 times a day for 14–21 days •• • Fluconazole 50-200 mg orally 4 times a day for 14-21 days • For candidal esophagitis - amphotericin B (doses vary).
Complications • With disseminated candidiasis •• Pyelonephritis •• Endophthalmitis •• Endocarditis, myocarditis, pericarditis •• Arthritis, chondritis, osteomyelitis •• Pneumonia •• CNS infection • With mucocutaneous candidiasis •• Patients with immunodeficiency often develop severe complications. The severity of complications in immunodeficiency depends on the degree of impaired immune status (a widely used marker is the number of CD4+ cells). Moderate suppression of the immune system (CD4+ cell count 200–500/μl) can lead to the development of chronic candidiasis. In severe immunosuppression (CD4+ cells less than 100/μl), thrush can cause damage to any system of the body, especially the kidneys (candiduria).
Forecast. The mortality rate of patients with hematogenous disseminated candidiasis is 40–75%, mortality from candidemia is 15–37%.
Prevention • Disseminated candidiasis. The use of fluconazole at a dose of 400 mg/day in patients who have undergone bone marrow transplantation or undergoing treatment for acute leukemia reduces the incidence of candidiasis • Mucocutaneous candidiasis: wearing cotton underwear.
Synonyms • Thrush • Candidiasis • Yeast mycosis • Moniliasis • Oidiomycosis.
ICD-10 • B37 Candidiasis
Notes • Most candidal infections are associated with endogenous flora • Person-to-person transmission is rare • Candidal vaginitis can be sexually transmitted (rare) • Oral candidal leukoplakia may be a precancerous condition (rare) • In patients with severe immunodeficiency, esophageal candidiasis may appear together with other infectious (eg, HSV, CMV) esophagitis • Skin tests, often used to diagnose or rule out anergy, are positive in 70–85% of individuals • Angular cheilitis (zaeda, angulitis) - inflammation and fissure in the area of the corner of the mouth; predisposing factors - decreased bite height (when wearing removable dentures), malnutrition, allergic dermatitis or fungal infection (Candida albicans).
Pathogenesis
The first stage of the disease development mechanism is the adhesion (attachment) of fungal cells to the surface of the esophageal mucosa. Subsequently, microorganisms are able to transform into a filamentous form and penetrate into the deeper layers of the esophageal wall. Tissue damage occurs due to the production of specific enzymes by the pathogen. Defects in the T-cell component of immunity play a great role in the manifestation of candidiasis.
The nature of the infection is determined by the state of the body's antifungal defense factors. When the immune system functions properly, transient carriage occurs. In cases of immune defects, persistent carriage without clinical symptoms usually occurs. If a person has one or more prerequisites, typical candidiasis develops.
Classification
According to the anatomical classification, damage to the esophagus by candida fungi refers to superficial forms of candidiasis. In practical gastroenterology, endoscopic classification is widely used, which is necessary to systematize the various options for damage to the esophageal mucosa. Clinicians distinguish 3 options for changes in the esophagus with candidiasis:
- Catarrhal esophagitis. It is characterized by hyperemia of the esophageal mucosa and moderate swelling. A candidal infection is indicated by a thin cobweb-like coating on the epithelium and contact bleeding.
- Fibrinous esophagitis. In the esophagus, whitish-gray plaques form in the form of plaques up to 0.5 cm in size. Hyperemia, swelling and bleeding of the mucous membrane are more intense than in the catarrhal form.
- Fibrinous-erosive esophagitis. Candidiasis is manifested by multiple plaques of a dirty gray color, after removal of which erosions are visualized on the mucous membrane. Spontaneous bleeding is characteristic.
Classification of candidiasis according to the severity of the disease:
| BY SEVERITY: | A COMMENT | ||
| by severity:: | Lightweight | a comment: | I am concerned about slight tightness and the appearance of a small amount of white plaque. |
| by severity:: | Average | a comment: | Itching appears, eating is difficult, white plaque is clearly visible |
| by severity:: | Heavy | a comment: | In addition to itching, there is pain, bleeding, eating is almost impossible, and fever is possible |
Symptoms of esophageal candidiasis
Typical signs of esophageal candidiasis are difficulty and pain when swallowing. A person experiences discomfort when eating solid and dry food, while when drinking, discomfort does not bother them. Pain is felt as a bolus of food passes through the esophagus. Some patients wash down each bite of food with water to relieve pain and burning.
Characterized by discomfort behind the sternum, which occurs regardless of the consumption of food. Belching with an unpleasant odor and heartburn appear less frequently. With severe damage to the esophagus, there is very severe pain while eating, so patients reduce the size of portions and the frequency of meals. Due to prolonged malnutrition, loss of body weight is noted, and symptoms of vitamin deficiency are added.
Treatment of candidal esophagitis
Candida under a microscope
Currently, there are many methods for treating various diseases. This disease is characterized by some difficulties in treatment. Sometimes the recovery process can take a long time, since not all methods are effective for one person.
It also sometimes happens that certain medications or procedures can lead to a number of serious side effects. Therefore, doctors approach the treatment of Candida esophagitis with great caution. Usually the patient is in the hospital under the supervision of a doctor. He is prescribed a number of medications, a special diet, and in severe cases, a hunger strike for several days.
Nutrition can also occur through a tube, but this is also in already complicated cases. The diet implies the exclusion of all foods that can damage the mucous membrane of the intestinal tract. These include alcohol, fatty foods, sweets, coffee, everything spicy and hot. In addition, cigarette lovers should give up their bad habit during treatment. For more effective treatment, sit on water for a couple of days or eat only fruits and vegetables.
Complications
The most common consequence of undiagnosed candidiasis is the formation of a stricture in the upper half of the esophagus - observed in 8-9% of cases. Cicatricial deformation of the organ is accompanied by constant dysphagia of both solid and liquid food and requires surgical correction. A dangerous complication is the dissemination of a mycotic infection with the development of deep candidiasis of internal organs and sepsis.
Due to the contact vulnerability of the mucous membrane, constant low-intensity bleeding is typical when the esophagus is injured by pieces of poorly chewed food. Chronic bleeding leads to iron deficiency anemia. Patients suffering from thrombocytopenia may experience profuse bleeding with hemorrhagic shock. Perforation of the esophagus is very dangerous, which manifests itself as painful shock, pneumomediastinum and subcutaneous emphysema of the neck.
Classification of candidiasis according to clinical course:
| ACCORDING TO CLINICAL COURSE: | A COMMENT | ||
| according to the clinical course:: | Superficial candidiasis | a comment: | Damage to the skin, mucous membranes and even nails occurs |
| according to the clinical course:: | Chronic widespread granulomatous candidiasis | a comment: | All mucous membranes are affected (the mucous membrane of the genital organs and oral cavity), the skin of the face, head, hands, and damage to internal organs is often found. In this case, the disease is chronic, i.e. long course with constant relapses. |
| according to the clinical course:: | Candidiasis of various organs |
Diagnostics
With esophageal candidiasis, there are no pathognomonic symptoms, so the diagnostic search includes a number of laboratory and instrumental methods. Sometimes, during an examination, a gastroenterologist notices foci of fungal infection of the oral cavity, which indirectly indicates the mycotic etiology of dysphagia. To confirm the diagnosis, the following research methods are used:
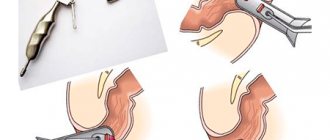
- Esophagogastroduodenoscopy. During endoscopic examination of the mucosa, typical changes are visualized, which are described in detail in the classification. During EGD, a biopsy of the area with suspicious plaque is taken. To exclude concomitant gastrointestinal diseases, the stomach and the initial parts of the duodenum must be examined.
- Biopsy examination. Cytological and histological analysis of biomaterial of the esophageal mucosa is the “gold standard” for diagnosing esophageal candidiasis. After special staining, blastomycetes are revealed under a microscope, which indicates the carriage of Candida fungi, or pseudomycelium - a sign of an active infection.
- Culture method. Sowing plaque from the esophagus onto nutrient media is performed to detect the species of the pathogenic fungus. Then a test is carried out to determine the sensitivity of the pathogen to the main antimycotic drugs, which is necessary for the rational selection of a treatment regimen.
Treatment of esophageal candidiasis
The basis of treatment for candidiasis infection is specific antifungal agents. They inhibit the synthesis of chemicals included in the cell wall of fungi. There are 3 groups of antimycotics, which differ in the degree of absorption when taken orally. Most often in clinical practice, azole antifungals are used, which must be taken for 2-3 weeks.
If the standard regimen is ineffective, the antimycotic is changed or switched to parenteral administration of the drug. The drug is taken until the clinical and laboratory symptoms disappear completely. For patients with AIDS, a prerequisite for cure is a decrease in viral load and an increase in the level of CD4 cells. For this purpose, modern antiretroviral therapy regimens are recommended.
Types of disease
The clinical picture of oral candidiasis is classified:
- For clinical and morphological.
- With the flow.
- By localization.
Clinical and morphological is divided into:
- Hyperplastic.
- Erosive-ulcerative.
- Pseudomembranous.
- Atrophic.
The clinical picture, classified according to the course, is divided into:
- Chronic.
- Spicy.
By localization:
- Cheilitis.
- Gingivitis.
- Glossitis.
- Stomatitis.
- Tonsillitis, etc.
Based on the clinical picture, oral candidiasis comes in several types:
- Chronic hyperplastic.
- Candida infection.
- Chronic atrophic.
- Acute pseudomembranous.
- Chronic pseudomembranous.
- Acute atrophic.
Prognosis and prevention
The likelihood of complete recovery depends on the conditions and causes that caused candidiasis. People with normal immune status have a favorable prognosis; cure requires 1 course of antifungal therapy. If the patient belongs to the category of carriers of HIV infection or takes immunosuppressants for health reasons, there is a risk of relapse of the fungal infection.
Primary prevention measures include controlled administration of immunosuppressants and antibiotics, early detection and treatment of oropharyngeal candidiasis. To prevent relapses, immunocompromised patients are advised to take a low-dose antifungal drug daily. Less often they resort to prophylactic weekly doses of doubled dosages of antimycotics.
You can share your medical history, what helped you in the treatment of esophageal candidiasis.
Prevention of relapses of oral candidiasis
For local and general prevention of candidiasis of the oral mucosa, medications prescribed by dentists and therapists are used.
Taking the following steps may help reduce your risk of developing the disease:9,10,11
- Regular oral hygiene: teeth should be brushed at least twice a day, flossed at least once a day
- Don't forget about dental brushes, a tongue scraper, and an irrigator. Even more careful hygiene must be carried out if you have a braces system or dentures, crowns, or implants.
- Mouth rinses can provoke candidiasis, so they should be used only as prescribed by a doctor.
- Caring for your dentures: They should be cleaned every day. Dentures should be removed before going to bed and cleaned with special solutions, brushes and pastes.
- Regular dental visits: Dental checkups should be done regularly, even if a person has no or few teeth. You need to visit the dentist once every 6 months. This is especially important for people who have chronic diseases, such as diabetes.
- Diabetes therapy: Saliva with a high sugar content provides a favorable environment for the growth of Candida albicans. Therefore, people with diabetes should monitor their blood sugar levels to reduce the amount of sugar in their saliva.
- Watch your diet: Eating foods rich in sugar and yeast can also promote the growth of Candida, so consumption of foods such as bread, beer and wine should be limited.
- Mouth rinse. People who use an inhaler for bronchial asthma must rinse their mouths after using such drugs. Inhaled corticosteroids suppress the immune system to help prevent inflammation that causes asthma. Unfortunately, they often also disrupt the immune mechanisms in the throat that control Candida albicans.
- Limit smoking: Inhaled tobacco smoke dries out the mouth and disrupts microbial balance, which can lead to Candida overgrowth.
Local preventive measures
1 If the causes of candidiasis of the oral mucosa are not eliminated, then 7–14 days after treatment, an anti-relapse course of local antifungal agents is administered. But it is better to immediately remove all risk factors.
2 Continuation of antiseptic treatment of the oral cavity for 10–14 days after treatment of mucosal candidiasis.
3 Restoration of normal microflora of the oral cavity is required.
4 Maintaining individual hygiene of the oral cavity and orthopedic structures (crowns, bridges) - includes cleaning the teeth, tongue, interdental spaces, care of dentures and their antiseptic treatment once a day.
5 Regular observation with microbiological examination when clinical manifestations of the disease occur.