Biliary, or hologenic, diarrhea is an unpleasant phenomenon that can affect both children and adults. However, while diarrhea with bile in newborns can be considered normal, in adults it can be a symptom of pathology in the body.
The appearance of bile in the stool primarily indicates problems with the gallbladder. Some factors provoke excessive secretion, which irritates the intestinal mucosa and causes diarrhea. These factors include:
- dysbacteriosis;
- viral diseases;
- food or alcohol poisoning;
- eating fatty foods in large quantities;
- gallbladder diseases;
- consequences of operations.
Causes of persistent diarrhea in adults
To understand why stool becomes liquid, let’s look at how thick, well-formed stool is normally formed.
Every day, about 9 liters of fluid enter the gastrointestinal tract (GIT) of an adult, of which 2 liters are food, and the rest is saliva, bile, pancreatic secretions, gastric and intestinal juices12. But we don't lose as much fluid in our stool because most of it is normally absorbed through the intestinal wall12. After such a “squeeze”, approximately 100-150 ml of water remains in the feces12.
Diarrhea develops if a “failure” occurs in the gastrointestinal tract12:
- fluid is released into the intestinal lumen too quickly;
- absorption through the intestinal wall is impaired;
- the volume of fluid entering the colon exceeds its absorption capacity;
- the motor activity of the intestine accelerates, and its contents move much faster than usual.
The listed mechanisms are interconnected, but each disease has its own predominant type5.
We will describe in detail below what specific factors provoke loose stools in an adult.
Irritable bowel syndrome
Irritable bowel syndrome (IBS) refers to periodic bowel movements and abdominal pain that are not associated with any pathology4. A doctor diagnoses IBS if these symptoms bother a person for more than six months and are present continuously over the last three months13, and the examination did not reveal other causes causing abdominal pain and loose stools2.
Pain in IBS is associated with bowel movements, occurs at least once a week, and is associated with changes in stool frequency and consistency13. IBS can occur with diarrhea, and sometimes diarrhea and constipation alternate7.
Diarrhea with IBS has the following features:
- Unpleasant symptoms usually become more pronounced due to stress and may disappear after bowel movement4.
- As a rule, diarrhea occurs in the morning after breakfast, in the first half of the day and does not bother you at night5.
- Although feces are passed more frequently, their volume usually does not increase over the course of a day5.
- Mucus is often present in stool5.
Diarrhea caused by bile acids (chologenic)
Bile acids are involved in the digestion of fats and are normally formed in the liver from cholesterol2. Together with bile, they enter the small intestine, where they are used to process food, and then are absorbed into the blood and again enter the liver2,14.
This process may be disrupted in the following cases6:
- for intestinal diseases (Crohn's disease)2;
- due to dysfunction of the biliary tract5;
- after infectious diarrhea2;
- after removal of the gallbladder2 or part of the intestine5.
If the reabsorption of bile is impaired, it enters the ileum and cecum5. Bile stimulates intestinal motility and the release of water and salts into its lumen5, causing diarrhea6.
Hologenic diarrhea manifests itself5:
- frequent, profuse loose stools;
- discharge of bright yellow or green stool;
- pain in the right lower abdomen (in most patients).
to come back to the beginning
Malabsorption in the small intestine
The absorption process in the intestine depends on the type of nutrient15. Under the influence of enzymes in the gastrointestinal tract, incoming food is processed with subsequent absorption of broken down substances15. When there is not enough enzyme to digest a certain food, diarrhea may occur4,5.
Most often, malabsorption in the small intestine is associated with:
- Celiac disease. This is a congenital intolerance to certain cereals, which is manifested by copious foamy stools after eating products made from wheat, rye, oats, and barley5.
- Lactase deficiency . It is observed if a person lacks lactase, an enzyme that is necessary to digest milk sugar (lactose)4. Without this enzyme, milk sugar is poorly digested4. Therefore, after consuming milk and dairy products9, watery diarrhea4 is observed.
Pancreatic insufficiency
We need pancreatic enzymes to digest fats, proteins and carbohydrates4. When the pancreas is damaged (for example, pancreatitis), its cells that produce enzymes are damaged4. Therefore, in the chronic course of the disease, a deficiency of digestive enzymes often occurs. Without pancreatic juice, the processing of nutrients is disrupted. The result is a violation of their absorption (malabsorption)4.
Typical manifestations of pancreatic insufficiency include4:
- fatty bulky feces;
- weight loss despite adequate food intake.
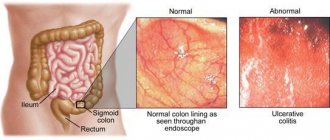
Inflammatory bowel diseases
When the intestinal mucosa is inflamed, a large amount of water and salts are released into its lumen, resulting in liquefaction of the stool1.
The main symptom of inflammatory bowel disease in adults is frequent loose stools with blood and mucus7. In the acute phase of the disease, body temperature usually rises, and
the frequency of bowel movements often reaches 30 times a day7.
Endocrine and metabolic disorders
Diarrhea is one of the manifestations of hormonal imbalance or metabolic disorders2,7 that occur with diabetes mellitus, thyroid dysfunction or adrenal insufficiency7.
In this case, diarrhea can occur for various reasons:
- strengthening the motor (motor) function of the intestines7;
- pancreatic enzyme deficiency6;
- Bacterial overgrowth syndrome6 (occurs when bacteria move from the large intestine to the small intestine)2.
Taking certain medications
According to statistics, up to 4% of cases of persistent loose stool can be caused by long-term use of certain medications2.
Currently, there are more than 700 drugs that cause diarrhea4. These include:
- drugs that normalize blood pressure (ACE inhibitors)2;
- magnesium preparations5;
- essential phospholipids (when prescribed in high doses)5;
- anticoagulants5;
- non-steroidal anti-inflammatory drugs5;
- antibiotics2;
- antiarrhythmic drugs2;
- antacids (reducing stomach acidity)5;
- antitumor agents2.
After discontinuation of the drug, diarrhea may stop within a day, but sometimes, if the intestinal mucosa is damaged, it takes longer for bowel movements to return to regularity4.
to come back to the beginning
Hologenic diarrhea: some aspects of pathogenesis and treatment
Hologenic diarrhea is a secretory diarrhea that occurs as a result of excess entry of bile acids (BAs) into the colon due to impaired reverse reabsorption in the ileum. The secretory effect of FA in the colon is carried out through a transmission mechanism - cyclic adenosine monophosphate, under the influence of which absorption is inhibited and the secretion of water and electrolytes in the colon is enhanced, which is the cause of diarrhea.
As is known, FAs, as the main component of bile, are involved in the breakdown and absorption of lipids and fat-soluble vitamins. The correct ratio of FA and cholesterol in bile prevents the precipitation of cholesterol and the formation of deposits in the gallbladder. Loss of fatty acids increases the risk of gallstone disease. In addition, FAs act as signaling molecules that regulate the activity of lipid and glucose metabolic pathways[1]. Their significant influence on the motor, sensory and secretory functions of the colon, as well as on the composition of the intestinal microflora is known[2]. Since the mechanisms of action of FAs are very complex, they can play an important role not only in the pathogenesis of gastrointestinal diseases, but also in the regulation of many metabolic processes.
In recent years, many works have appeared in the literature highlighting the mechanisms of FA absorption and their malabsorption, which results in diarrhea. There are three types of FA malabsorption. Type 1 has been studied for a long time and occurs during resection or inflammation of the ileum (Crohn’s disease, etc.) [3, 4]. Under physiological conditions, 95% of FAs are reabsorbed in the ileum and transported back to the liver. When the ileum is damaged, the absorption of fatty acids is impaired, and they enter in excess into the colon, causing hologenic diarrhea. A survey of 298 patients with chronic watery diarrhea showed the presence of positive tests characteristic of FA malabsorption in 15 (51.7%) of 29 people with Crohn's disease, in 40 (93.0%) of 43 patients after resection of the ileum, in all 12 (100%) patients after resection of the small intestine and in 2 (66.7%) out of 3 people after radiation damage to the small intestine[5].
There is a dependence of the severity of diarrhea syndrome on the volume of resection of the small intestine[6]. Excess fatty acids, secondary to damage to the site of their absorption, served as the basis for the name of this type of hologenic diarrhea - secondary. This type is the most common and well studied.
Type 2 (idiopathic, or primary) was first described by E. H Thaysen and L. Pedersen in 1976 and received its name due to the absence of pathohistological signs of damage to the ileum [7]. It was considered rare for a long time. However, recent studies indicate that the small number of patients with this type of hologenic diarrhea was due to the complexity of its diagnosis. Recent research suggests that among patients with irritable bowel syndrome (IBS) with diarrhea, more than 30% have hologenic diarrhea and its prevalence may be as high as 1% in Western Europeans[8].
The etiology of idiopathic hologenic diarrhea remains unclear to date. Several of its pathophysiological mechanisms are considered. Evidence has emerged that the idiopathic variant of FA malabsorption is associated with rapid transit of intestinal contents[9, 10]. Other researchers believe that the cause is genetic defects in the regulation of transport and synthesis of FAs or the molecular mechanisms responsible for these processes [11]. Type 3 - mixed, includes conditions in which hologenic diarrhea may also occur: for example, previous cholecystectomy, bacterial overgrowth syndrome, pancreatitis, microscopic colitis, celiac disease, etc. [12, 13].
In recent years, the effect of taking the hypoglycemic drug metformin on impaired fatty acid reabsorption due to increased secretion of glucagon-like peptide 1 has been actively studied, however, these data are very contradictory, and the mechanisms of such an effect are not fully understood [14]. Thus, the central link in the pathogenesis of hologenic diarrhea is a violation of the enterohepatic circulation of fatty acids due to various reasons.
It is known that the synthesis of primary FAs (cholic and chenodeoxycholic) occurs in the liver from cholesterol. It is provided by the enzyme 7αhydroxylase, which is one of the forms of cytochrome P450 (P450 7A1 or CYP7A1). During the process of conjugation—the addition of ionized glycine or taurine molecules to the carboxyl group of FA—glycine and taurine conjugates of FA are formed. The excretion of FA into the bile capillaries mainly occurs with the help of a transport protein designated as the bile salt export pump. Some FAs in the intestine are exposed to bacterial enzymes, which cleave glycine and taurine, as well as the hydroxyl group of FAs, forming secondary FAs. Secondary FAs: deoxycholic acid, formed from cholic acid, and lithocholic acid, formed from chenodeoxycholic acid, are less soluble and are absorbed more slowly in the intestine than primary ones. Normally, a small part of the fatty acids not absorbed in the ileum (about 0.3–0.6 g/day) is excreted from the body with feces. With an increase in the amount of secondary fatty acids in the colon, the secretion of sodium and water increases, and hologenic diarrhea occurs.
Absorption in the terminal ileum and the entry of FA into the cells of the small intestine occurs through both passive diffusion and the apical sodium-dependent FA transporter - the ASBT (apical sodium bile acid transporter) protein located on the enterocyte; and FA delivery to the portal vein system is carried out by the so-called organic solute transporter α/β. FAs penetrate into hepatocytes with the participation of sodium taurocholate cotransporting polypeptide (NTCP) and organic anion transporting polypeptide (OATP) [15]. These transporters allow the transfer of FAs from the blood into hepatocytes against a high concentration gradient and electrical potential.
Providing a balance between the synthesis, uptake and excretion of hepatobiliary transporters is tightly regulated by nuclear receptors. Enterocytes and hepatocytes have a receptor (FXR), stimulation of which in enterocytes by FA induces transcription of the hormone fibroblast growth factor 19 (FGF19) [16, 17]. This process is triggered by all FAs, although it occurs more intensively with the help of chenodeoxycholic and glycochenodeoxycholic acids. Subsequently, released from the enterocyte and circulating in the portal vein system, FGF19 interacts with the FGF4 receptor on the hepatocyte membrane through indirect regulation of the constant endoplasmic reticulum protein klothoβ[18]. As a result of this process, CYP7A1 is inhibited and the synthesis of new FAs is suppressed through the proteins of the so-called small heterodimer partners [19]. At the same time, the expression of transport proteins NTCP and OATP in hepatocytes and the active absorption of FA from the portal vein system decrease. Disturbances that occur at various stages of regulation, reabsorption, synthesis and transport of FAs in the enterohepatic circulation of FAs can lead to the occurrence of hologenic diarrhea.
One such disorder is FGF19 deficiency, first discovered by GR Walters et al. in patients with idiopathic type of hologenic diarrhea. The lack of this hormone via a feedback mechanism leads to the activation of the synthesis of new FAs in the liver, an increase in their amount in the small intestine and the occurrence of hologenic diarrhea[12]. A rare disorder leading to idiopathic hologenic diarrhea is a genetic defect in the ASBT protein, which results in impaired reabsorption of fatty acids from the intestinal lumen into the enterocyte[20]. The clinical picture of hologenic diarrhea is characterized by frequent watery stools, combined with pain in the right abdomen, often in the projection of the cecum, as well as a burning sensation in the rectum and anus [21, 22]. The absence of clinical symptoms of disease progression, despite its duration, often leads to an erroneous diagnosis of IBS. The table shows the differential diagnostic features of hologenic diarrhea and diarrhea in IBS.
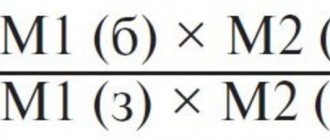
Table Differential diagnostic signs of hologenic diarrhea and diarrhea in irritable bowel syndrome (IBS)
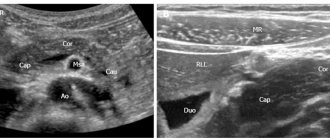
To diagnose hologenic diarrhea, methods for detecting FA malabsorption have been developed, but there are difficulties in reproducing them, and they are not always publicly available [23]. Quantitative assessment of FAs in feces is labor-intensive and requires a specially equipped laboratory.
Diagnosis of FA malabsorption can be made using the SeHCAT test, which is based on the use of an analogue of conjugated FA (75Se homocholyltaurine), passing through all stages of the enterohepatic circulation, the loss of which is recorded 7 days after oral administration of this substance using a γ camera. Retention of SeHCAT in the body 7 days after oral administration of less than 15–10% of the initial value indicates the presence of FA malabsorption. However, due to the use of special expensive equipment, this method is not always available. Using high-resolution liquid chromatography, it is possible to measure the serum level of the FA precursor, 7αhydroxy4cholestene31 (C4), the increase of which also indicates increased FA synthesis, characteristic of hologenic diarrhea[13]. C4 levels are significantly increased in patients with hologenic diarrhea, with sensitivity and specificity of 90% and 79%, respectively. Moreover, the C4 content correlates well with the SeHCAT index. Given its simplicity and cost-effectiveness, C4 level testing is more attractive as a screening test for diagnosing hologenic diarrhea[24].
Determination of FGF19 concentration in blood serum by enzyme immunoassay can also be used as a test for diagnosing FA malabsorption [25]. Previous studies have shown that median FGF19 levels are significantly lower in patients with idiopathic hologenic diarrhea than in controls (120 pg/ml vs. 231 pg/ml), and fasting C4 levels are significantly higher than in controls (51 ng/ml versus 18 ng/ml), which confirms the deficiency of feedback inhibition by the hormone FGF19, which results in overproduction of FAs and hologenic diarrhea[12]. For the quantitative determination of FA in feces, a spectrophotometric enzyme method is used. In an alcoholic extract from stool samples weighing 1–1.5 g, the concentration of FAs is determined using an enzymatic method, followed by the calculation of their daily excretion, taking into account the number of feces per day. According to L.M. Krooms et al., in healthy individuals, the loss of FA in feces ranges from 100–200 mg/day. In patients who underwent resection of more than 100 cm of the ileum, the average loss of FA was 2250.7 ± 685.3 mg/day. In the group of those who underwent cholecystectomy, the average content of FA in feces also exceeded the norm and averaged 786.4 ± 103.7 mg/day [21].
The recommendations of the British Society of Gastroenterology and the American Gastroenterological Association suggest empirical administration of the FA sequestrant cholestyramine as a test for the presence of FA malabsorption. A positive clinical effect from its use may indicate malabsorption[26].
Cholestyramine is a synthetic anion exchange resin used to absorb fatty acids into the small intestinal lumen. Just as in the case of the use of carbon enterosorbents, the removal of FAs from the enterohepatic circulation leads to an increase in their hepatic synthesis, consequently, to a decrease in the concentration of cholesterol in the blood plasma. Cholestyramine is a fine powder of a strong base resin in chloroform, administered as a shake with fruit juice or milk and has a distinctly unpleasant taste. This circumstance, as well as the frequent occurrence of constipation while taking this drug, forced the development of a number of other synthetic resins for removing fatty acids, in particular cholestipol, colesevelam. The latter enterosorbent has 4–6 times greater affinity for fatty acids than cholestyramine and, being a swelling hydrogel, has practically no constipatory effect [27].
Despite the pronounced positive therapeutic properties, drugs that bind FAs have a number of negative effects. These include the absorption of drugs, the absorption of fat-soluble vitamins, etc. This requires monitoring the level of vitamins during long-term use of these drugs[28]. In addition to polymer ion exchange sorbents for the treatment of hologenic diarrhea, it is possible to use natural dietary fiber, chitosan-based enterosorbents and carbon adsorbents, but their therapeutic effect is somewhat lower than that of cholestyramine, so they are not always effective.
Experimental drugs currently used to treat hologenic diarrhea include obeticholic acid. There is evidence of an increase in serum FGF19 levels in patients with idiopathic hologenic diarrhea and with sparing (less than 45 cm) ileal resection after the use of obeticholic acid[29]. Obeticholic acid (also known as INT747 and 6αethylCDCA) is a potent FXR receptor agonist and can stimulate FGF19 production in a dose-dependent manner[30].
CONCLUSION Hologenic diarrhea is a nosological form that is found in more than 30% of patients diagnosed with functional diarrhea or irritable bowel syndrome.
The most sensitive and specific method for diagnosing bile acid malabsorption is the SeHCAT test. The simultaneous use of other diagnostic methods (measurement of the level of 7α-hydroxy-4-cholestene-3-1 or fibroblast growth factor 19) and further study of the pathogenesis of various types of hologenic diarrhea will make it possible to more accurately establish the diagnosis and prescribe adequate treatment. The main therapeutic agents for hologenic diarrhea are cholestyramine and other enterosorbents.
Symptoms of diarrhea in adults
The main symptom of diarrhea is an increase in fluid content in the stool10. Diarrheal syndrome is characterized10 by:
- discharge of unformed, liquid or mushy feces more than 3 times a day;
- increase in its weight (more than 200 grams);
- the presence of impurities - mucus, blood or particles of undigested food.
If such changes bother a person for more than 4 weeks, diarrhea is considered chronic2.
Diarrhea may also cause:
- urgent painful urge with a feeling of incomplete emptying5.
- fecal incontinence1;
- flatulence5;
- abdominal pain5;
- discomfort in the rectum7;
- malaise and fatigue7;
- decreased appetite and weight loss7.
- redness and irritation of the skin around the anus5;
- fissures in the anal area5.
Since diarrhea can be a sign of chronic illness, it is important to first find out the cause. To do this, consult a doctor - a therapist or gastroenterologist.
Make an appointment with a specialist as soon as possible if2:
- less than 3 months have passed since the onset of symptoms;
- loose stools are a constant concern;
- your weight has decreased significantly.
Treatment of persistent diarrhea in adults
Treatment of chronic diarrhea should be comprehensive8. First of all, it is necessary to find out the causes of loose stools and, if possible, eliminate them12. Various drugs are used as adjuncts to relieve symptoms of diarrhea1,3.
For example, the following can be used as symptomatic treatment:
- antidiarrheals3;
- adsorbents and astringents (activated carbon, bismuth, drugs that bind bile acids)3;
- enzymes to improve food digestion1;
- drugs that restore the composition of intestinal microflora1.
In the absence of blood in the stool and fever, antidiarrheal drugs based on loperamide9, for example, Imodium® Express, can be prescribed. The drug helps stop diarrhea: it suppresses excessive intestinal peristalsis (contractions) and slows down the movement of feces11. Loperamide also increases the tone of the anal sphincter, promoting fecal retention11.
Imodium® Express is available in a convenient dosage form of lozenges. They do not need to be washed down with water - they dissolve on the tongue within a few seconds11.
Any antidiarrheal drug, including those containing loperamide, should be taken with caution and only after consultation with a specialist9. Imodium ® Express should not be used as primary therapy for exacerbation of ulcerative colitis or pseudomembranous enterocolitis (diarrhea caused by antibiotics)11. The drug is contraindicated for women in the 1st trimester of pregnancy and during lactation. Imodium ® Express in the 2nd and 3rd trimester is prescribed only by a doctor11.
to come back to the beginning
Diet and drinking regime
The primary and leading method of combating chronic diarrhea is diet8. If diarrhea occurs or gets worse after eating certain foods, eliminate them from your diet. When creating a menu, keep in mind that there are foods that have a fixing effect, and those that can worsen diarrhea.
| Products recommended for diarrhea16 | Foods to avoid if you have diarrhea |
|
|
To replenish the volume of fluid lost in feces, drink diluted fruit juices, flavored soft drinks, and give preference to liquid foods - soups and broths9. It is very important that the food is complete; its daily calorie content should be approximately 2500–2600 kcal8.
Not every frequent or loose stool is considered diarrhea. The frequency of bowel movements and the volume of stool largely depend on nutrition, the amount of water drunk, and the quality of digestion in the intestines1. To stop diarrhea, you must first determine its cause. Antidiarrheal drugs can be used as an additional treatment for persistent diarrhea in adults, but in some cases they are contraindicated. Therefore, before taking any medications, consult your doctor.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
to come back to the beginning
Gallstone disease (calculous cholecystitis) - symptoms and treatment
In the mid-twentieth century, the following method of treating cholelithiasis was studied in animal experiments: the gallbladder was cut, the stones were taken out, and sutured back. However, over time, the stones formed again, which is understandable, since gallstones are only a manifestation of the disease, and not the disease itself. Chronic inflammation of the gallbladder did not disappear, which led to relapse of the disease.
The next attempt to cure cholelithiasis without surgery was shock wave lithotripsy (similar to the treatment of urolithiasis). But this type of treatment caused rupture of liver tissue or the wall of the gallbladder with the formation of abscesses, hematomas and peritonitis. Fragments of stones, even if they were crushed, migrated into the ducts, causing choledocholithiasis and obstructive jaundice. The method had to be left in the past.
Some gastroenterologists recommend their patients take various choleretic drugs, as well as different types of “dubages” for the purpose of conservative treatment of cholelithiasis. Under the influence of this therapy, stones can easily migrate from the gallbladder into the extrahepatic bile ducts, causing choledocholithiasis and obstructive jaundice, which in turn will require emergency surgical intervention.
Thus, the only method of radical cure for gallstone disease is its removal - cholecystectomy.[3]
Initially, this operation was performed through a traditional (laparotomy) approach, which led to a large number of complications both in the early and late postoperative period. With the development of new technologies, the operation began to be performed laparoscopically.[7]
Cholecystectomy is performed as follows:
- through a centimeter incision above the navel, a tube (trocar) and a laparoscope are inserted into the abdominal cavity, the abdominal cavity is filled with carbon dioxide, thus forming a space for surgery;
- additionally install another centimeter and 25 mm trocars;
- with the help of special instruments, the gallbladder is mobilized, separated from the bed, the cystic duct and the artery are clipped with titanium clips;
- The gallbladder is removed through periumbilical or epigastric access.
The operation is performed under general anesthesia and lasts on average for an hour. Thanks to the low-traumatic laparoscopic approach, postoperative pain is minimal, and already in the evening on the day of surgery the patient can get up and walk without experiencing severe pain.
If the postoperative period is smooth, the patient can be discharged the next day after surgery, which is especially important for people of working age. The cosmetic defect of the operation is minimal; already a month after the operation, the scars become almost invisible.[6]
In parallel with laparoscopic cholecystectomy, cholecystectomy from a minilaparotomy approach arose. However, due to the difficulty of visualizing the elements of the hepatoduodenal ligament and the high risk of trauma to neighboring organs, this approach is practically not used.
Relatively recently, laparoscopic cholecystectomy began to be performed from a single approach. When performing this operation, a single incision 3-4 cm long is made above the navel. This access is especially relevant if the patient has an umbilical hernia, as it allows you to solve two problems through one incision.
NOTES surgery—operations through natural orifices—is gaining increasing popularity. Thus, laparoscopic cholecystectomy can be performed through an incision in the vagina or rectum, which does not leave scars on the abdomen, but is fraught with infectious and other complications.
Bibliography
- Kushnir I.E. Diarrhea syndrome: diagnostic and therapeutic tactics // Faces of Ukraine. – 2010. – No. 7 (143). – pp. 42-45 https://www.health-medix.com/articles/liki_ukr/2010-08-16/10IEKITT.pdf
- Arasaradnam RP et al. Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology, 3rd edition Gut 2018; 67:1380–1399.
- Peter AL Bonis, J Thomas Lamont. Approach to the adult with chronic diarrhea in resource-rich settings. Official reprint from UpToDate. 2020 https://www.uptodate.com/contents/approach-to-the-adult-with-chronic-diarrhea-in-resource-rich-settings?search=diarrhea&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3
- Descoteaux-Friday GJ, Shrimanker I. Chronic Diarrhea. [Updated 2020 Nov 17]. In: StatPearls Publishing; 2022 Jan- URL: https://www.ncbi.nlm.nih.gov/books/NBK544337/
- Tarasova L.V., Trukhan D.I. Differential diagnosis for diarrhea. Experimental and Clinical Gastroenterology 2015; 124(12):105–110
- Burgers K, Lindberg B, Bevis ZJ. Chronic Diarrhea in Adults: Evaluation and Differential Diagnosis. Am Fam Physician. 2022 Apr 15;101(8):472-480. — URL: https://pubmed.ncbi.nlm.nih.gov/32293842/
- Sarsenbaeva A. S., Lazebnik L. B. Diarrhea in adults. Clinical recommendations. Project. Experimental and clinical gastroenterology. 2020;178(6): 4–41.
- Loranskaya I.D. Diarrhea in diseases of the digestive system // Attending physician. – 2007. – No. 6
- LaRocque R et al. Approach to the adult with acute diarrhea in resource-rich settings // Uptodate: Professional Version 2022. – URL: https://www.uptodate.com/contents/approach-to-the-adult-with-acute-diarrhea-in -resource-rich-settings#H24
- Chronic diarrhea syndrome in the practice of a therapist: examination tactics, basic principles of treatment: textbook. allowance / L. I. Butorova, G. M. Tokmulina. – M.: Prima Print, 2014. – 112 p.: ill. – ISBN 978-5-9905962-0-7.
- Instructions for use of the drug Imodium®Express// Registration number N016140/01// RF GRLS. – URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=fdbc42af-4580-4ecd-93d8-2e9a965c707a&t= (access date: 06/26/2021)
- Shvets N.I., Bentsa T.M. Pharmacotherapy of diarrhea syndrome. Rational pharmacotherapy, 4 (13)' 2009. - URL: https://rpht.com.ua/ru/archive/2009/4%2813%29/pages-38-44/farmakoterapiya-diareynogo-sindroma
- Abdominal pain and visceral hypersensitivity in patients with irritable bowel syndrome. Rome criteria IV and clinical practice / Ardatskaya M.D., Topchiy T.B. – M.: Prima-Print 2022. – 63 p.: ill. – ISBN 978-5-9907557-9-6.
- Great Medical Encyclopedia (BME), edited by Petrovsky B.V., 3rd edition. Volume 8. Bile acids
- Metelsky S.T. Physiological mechanisms of absorption in the intestine. Ross. magazine gastroenterol., hepatol., coloproctol. 2009; 3:51-56.
- Leslie Bonci. Diet Strategies for Managing Chronic Diarrhea: International Foundation for Gastrointestinal Disorders, 2022. — URL: https://mk0iffgd43a85spvyq6.kinstacdn.com/wp-content/uploads/208-Diarrhe…