Indications for the study
The location of the pancreas is such that the organ is practically impossible to examine when examined by a doctor. The ultrasound procedure is a widely used method of organ visualization.
Indications for ultrasound:
- pain in the left hypochondrium - prolonged, intense;
- unpleasant sensations of palpation of the abdomen in the projection of the pancreas;
- suspicion of an inflammatory or tumor process in this part of the abdomen;
- the need to exclude complications from previously performed diagnostic or therapeutic procedures;
- control of the treatment;
- additional examination to clarify the diagnosis.
Ultrasound examination of the pancreas is sometimes performed on an emergency basis - for example, in case of abdominal trauma and suspected rupture of internal organs. Modern ultrasound equipment allows examination even outside the medical institution - directly at the scene of the incident.
However, it is up to the doctor to determine whether an ultrasound of internal organs is necessary. He also evaluates the result. Self-diagnosis is not acceptable.
Decoding
The essence of the pancreas ultrasound procedure is that the dense organ reflects ultrasound waves, which are converted into electrical impulses - the doctor sees the image on the computer screen. It is by this that he judges the structure and functioning of the digestive structure.
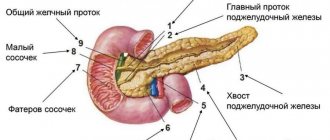
Ultrasound of the pancreas allows you to evaluate the following parameters:
- size - when they increase, an acute inflammatory process can be assumed, while when they decrease, a chronic course of pancreatitis can be assumed;
- shape and contours - clear delineation and smooth transition from the body of the organ to its tail and head, without jaggedness or discontinuity;
- structure – dense, homogeneous;
- echogenicity - reflection of ultrasonic waves, similar to that of the liver;
- structure of ducts - diameter, expansions, additional inclusions;
- the location of the organ relative to large vessels, as well as the spine.
All of the above parameters allow the doctor, who evaluates the ultrasound results, to get a complete picture of the condition and functioning of the pancreas.
Acute pancreatitis
This disease ranks 3rd in the structure of surgical pathology (after appendicitis and cholecystitis) and is initially an aseptic inflammation of the pancreas in the form of diffuse damage to the parenchyma in the edematous phase and volumetric organic lesions in the necrotic phase.
The edematous form is easier and can be treated conservatively, but in a hospital setting.
Necrotizing pancreatitis, especially purulent one, is extremely severe, with a mortality rate of 20-50%; the main method of treatment is repeated surgical interventions.
Leading reasons:
- violation of the outflow of pancreatic juice;
- abuse of alcohol and spicy, fatty foods;
- allergic reactions;
- surgical interventions on the pancreas.
Ultrasound protocol of a healthy organ
An ultrasound protocol with the following gland sizes will indicate a healthy and properly functioning digestive structure:
- The structure of the head is correct, the contours are clear, echogenicity is normal:
- length – from 2.5 cm to 3.5 cm;
- thickness – up to 3.2 cm;
- The body of the organ is dense, clearly visible on the screen, without additional inclusions:
- length – from 1.75 cm to 2.5 cm;
- thickness – up to 2.1 cm;
- The tail is clearly visible during examination, with clear contours and echo density of the liver:
- length – from 1.5 cm to 3.5 cm;
- thickness – up to 3.5 cm.
Normally, the structure of the gland is homogeneous - there are small lobules that are responsible for the production of digestive juice. Individual cells secrete the hormone insulin, which is important for regulating carbohydrate metabolism.
Each person has different organ sizes. They may differ slightly from the basic age parameters. This cannot indicate the course of any pathology. The doctor must compare the ultrasound results with information from laboratory tests.
Deviations in the structure of the organ and their possible causes
An acute inflammatory process according to ultrasound manifests itself in an increase in size, as well as a decrease in the echo density of the gland itself - due to tissue swelling.
Additional changes:
- pronounced heterogeneity of structure;
- dilation of the main duct of the gland;
- swelling in surrounding tissues;
- accumulation of fluid - in or near an organ;
- the formation of additional formations – pseudocysts – is possible.
Repeated acute inflammations later lead to chronic pathological changes in the pancreas structure. Signs indicate this:
- reduction in size;
- blurred contours, blurred isthmus;
- replacement of healthy cells with fatty elements;
- change in echogenicity.
In case of persistent pain and no effect from the treatment, the doctor also prescribes ultrasound monitoring to exclude oncological changes in the organ.
Signs of a tumor:
- focal defect in one of the lobes – mixed echogenicity;
- a clear contour of the additional inclusion with simultaneous deformation of the outer wall of the gland;
- persistent dilation of the duct;
- enlargement of nearby lymph nodes.
The final diagnosis is made by the attending physician, and not by an ultrasound specialist. Therefore, with the result of the diagnostic procedure, a person must consult his doctor.
Why is MRI prescribed for diseases of the pancreas?
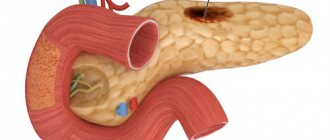
The pancreas is one of the most important organs of the human body. It simultaneously performs two completely different functions: endocrine and digestive. Diseases of the pancreas have been studied for many centuries. A lot of information has accumulated to date about the clinical manifestations and laboratory signs of various pathologies of this organ. This allows modern clinicians to identify and treat many known pancreatic diseases.
And yet, the active development of science, the emergence of new, high-precision research methods, such as, for example, the MRI method, contribute to earlier and more reliable diagnosis of known pathology, as well as the identification of new, previously undiagnosed diseases. It is an undeniable fact that the modern rhythm of human life, urbanization, and active work contribute to disruption of the work and rest regime and diet. In combination with this, the decrease in the quality of the food products themselves, as well as the deterioration of the environment, have a pronounced negative (including carcinogenic) effect on the human body in general, as well as its organs and systems in particular. This contributes to a significant “rejuvenation” of various diseases, incl. and diseases of the pancreas.
The decrease in the working capacity of young people is the most important economic and social problem of the present, requiring modern medicine to be active in matters of the earliest possible detection of the pathological process and timely initiation of treatment.
MRI is one of the modern and most highly accurate diagnostic methods that helps resolve the issues raised.
The most common pathology that clinicians have to deal with is inflammatory processes in the pancreas – pancreatitis.
There is acute pancreatitis, characterized by the activation of the digestive enzymes of the gland even before they enter the intestine and, accordingly, the effect of these enzymes on the tissue of the gland itself.
Clinically, this process is manifested by severe “girdling” pain in the upper abdomen with irradiation to the shoulder blades or left clavicle, to the posterior parts of the lower ribs on the left. In addition, there is vomiting, repeated, painful, not bringing relief; tachycardia; bloating.
Acute pancreatitis.
Acute pancreatitis with the formation of parapancreatic abscesses.
Chronic pancreatitis is a progressive inflammatory disease of the pancreas with periods of remissions and exacerbations of the pathological process, leading to dystrophic changes in the organ, the growth of connective tissue in it and a decrease in the production of enzymes and hormones.
Clinically, periods of exacerbation of chronic pancreatitis are not much different from an attack of acute pancreatitis.
Pathomorphologically, the following types of chronic pancreatitis are distinguished:
Chronic atrophic pancreatitis is characterized by local or diffuse reduction in the size of the pancreas, fibrosis, calcification and fatty degeneration of its parenchyma.
Chronic atrophic pancreatitis.
Chronic pseudotumor pancreatitis is characterized by a local or diffuse increase in the size of the gland, fibrosis, calcification, fatty degeneration of the parenchyma, and the presence of pseudocysts.
Pseudotumorous form of chronic pancreatitis.
Pseudotumorous form of chronic pancreatitis.
IPMN (Intraductal Papillary Mucinous Neoplasms) – intraductal papillary tumor.
Chronic fibrocystic pancreatitis.
When identifying tumor diseases of the pancreas, the MRI method is the most informative among other diagnostic methods.
MRI allows you to clearly visualize the tumor, regardless of its size; carry out differential diagnosis of various types of tumors and metastatic lesions of the pancreas; reliably detect biliary hypertension and dilation of the Wirsung duct.
The pancreas is susceptible to the development of tumor processes such as adenocarcinoma and cystadenocarcinoma (poorly and highly differentiated), insulinoma (neuroendocrine tumor), lymphoma, and metastases.
It is a malignant tumor arising from the cells lining the pancreatic duct.
Clinically, it usually does not manifest itself for a long time until it reaches a large size. The first symptoms are abdominal pain and weight loss.
Pancreatic body cancer (adenocarcinoma). Reliable visualization of the tumor without increasing the size of the gland, expansion of the Wirsung duct of the tail of the gland.
In most cases, the tumor is localized in the head of the pancreas, i.e. in maximum proximity to the duodenum and the common bile duct. When large in size, the formation leads to the development of obstructive jaundice. Manifested by icteric staining of the skin and sclera.
Cancer of the head of the pancreas.
This is a cystic multilocular tumor with the presence of nodes and septa of varying thickness, characterized by expansive growth. With large sizes, obstruction of the pancreatic duct and the development of obstructive jaundice are also possible.
Pancreatic cystadenocarcinoma.
It is a hormonally active tumor of pancreatic β-cells that secretes excess insulin, which leads to hypoglycemia.
Attacks of hypoglycemia with insulinoma are manifested by tachycardia, tremor, paresthesia, cold sweat, feelings of hunger and fear, as well as visual disturbances. Speech and behavioral disorders.
In severe cases, hypoglycemic coma develops.
Small insulinoma of the tail of the pancreas.
In addition to primary tumors, the pancreas is also susceptible to metastasis from other organs. The pancreas is most often affected by metastases from gastric cancer. With sarcoma, melanoma, hepatoma, chorionepithelioma (cancer of the female genital organs), lung, ovarian, breast and prostate cancer, metastasis to the pancreas occurs much less frequently.
High detection of liver metastases and high contrast of pancreatic tail tumors on MRI.
Multiple metastases to the pancreas.
Pancreatic tumors, even often small ones, can lead to obstruction of the biliary tract with the development of biliary hypertension.
Small-sized mass formation of the pancreas (1); biliary hypertension (2).