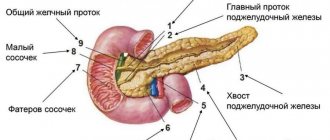
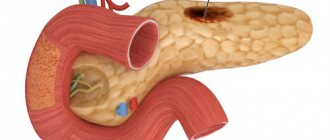
The pancreas is a unique organ of the digestive system that simultaneously performs two functions:
- endocrine – internal secretion of hormones (insulin, glucagon, somatostatin, vasoactive intestinal peptide) and pancreatic polypeptide;
- exocrine - external secretion of pancreatic juice, the basis of which are digestive enzymes.
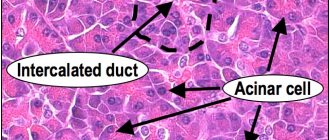
Parenchyma (organ tissue) consists of cells and stroma, including excretory ducts and blood vessels. Normally, the parenchyma should be homogeneous (uniform).
A heterogeneous, otherwise diffusely heterogeneous structure of the pancreas indicates the presence of pathological processes, dysfunction, and possible cell necrosis.
Detection of deviations
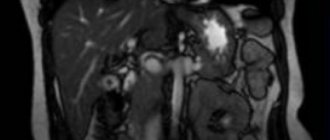
The primary methods for diagnosing pancreatic diseases are laboratory tests and ultrasound. Among the ultrasound parameters, the main ones are echogenicity (conductivity or the degree of reflection of ultrasound, indicating tissue density), contours and structure of the organ. Next, the sizes of the constituent parts of the gland (body, head, tail) are examined.
Normal indicators of an ultrasound examination of an adult
| Echogenicity | Outlines | Structure | Body | Head | Tail | Neoplasms |
| normal or isoechoic | clear | homogeneous | 2.5 cm | 3.5 cm | 3 cm | none |
Homogeneity on an ultrasound monitor is defined as a uniform gray coloration of the entire organ with a fine-grained or coarse-grained echostructure. The degree of ultrasound conductivity is determined by the presence and volume of liquid:
- isoechoicity – average, normal ultrasound reflection (gray parenchyma);
- hypoechogenicity – reduced conductivity (dark tissue);
- hyperechogenicity – increased conductivity (visualized in shades of white);
- anechoicity - ultrasound is not reflected (black parenchyma).
A diffuse-heterogeneous structure is most often characterized by hyperechogenicity of varying intensity, which indicates the development of pathological processes (inflammatory, tumor, fibrous, necrotic, etc.).
Diffusely heterogeneous changes mean a uniform violation of the homogeneity of the structure throughout the gland. Efficient parenchyma cells are gradually replaced by adipose or connective tissue that does not bear a functional load.
Ultrasound detection of a diffusely heterogeneous structure of the pancreas is not a diagnosis, but a sign of disorders indicating a particular disease. The patient may be prescribed additional diagnostic examinations (retrograde cholangiopancreatography, magnetic resonance and computed tomography).
Features of preparation for ultrasound
To objectively identify structural changes in the pancreas before performing an ultrasound, the patient must:
- 2-3 days before the examination, avoid alcohol-containing drinks and foods that cause intense gas formation (legume dishes, cabbage, fermented milk drinks, baked goods);
- the day before the procedure, start taking carminative drugs (Espumizan, activated carbon).
The fasting regime before an ultrasound of the abdominal organs is 8-12 hours.
What is echogenicity?
Depending on the number of reflectors that appear during the passage of ultrasonic waves, all structures are characterized as:
- isoechoic structures (medium echogenicity) are comparable in color to the comparison area;
- hypoechoic structures are darker in color than the comparison area;
- hyperechoic structures have a lighter shade relative to the comparison area. The more reflective surfaces, the higher the echogenicity, the whiter the image appears on the screen. Very dense structures such as bones and stones, as well as air, do not completely transmit ultrasonic signals.
- anechoic structures do not reflect signals at all during ultrasound, and therefore are displayed in black. Such objects, for example, include fluid structures (bladder, gallbladder, simple cysts).
Reasons for changes
Changes in the structure of the pancreas against the background of hyperechogenicity accompany acute inflammation, edema, fibrosis, and fatty deposits. The main diseases diagnosed based on the results of an ultrasound examination:
What does an ultrasound of the pancreas show?
- an increase in the volume of intracellular fat and replacement of parenchyma with adipose tissue - steatosis;
- accumulation of fluid (edema) is not an independent pathology, but a consequence of diseases of the gland itself, the duodenum, hepatitis, helminthic infestations, stones in the gall bladder, etc.;
- benign tumors (gastrinoma, insulinoma, glucagonoma);
- proliferation of atypical cells – pancreatic cancer;
- acute and chronic inflammation of the organ - pancreatitis;
- synchronous inflammatory damage to adjacent organs of the hepatobiliary system (pancreas and gallbladder) - cholecystopancreatitis;
- motor-tonic dysfunction of the gallbladder and bile duct sphincters - biliary dyskinesia;
- death of gland cells - pancreatic necrosis;
- diabetes mellitus (insulin-dependent type 1 with hereditary predisposition);
- proliferation of connective tissue and replacement of its working cells – fibrosis;
- pancreolithiasis - the presence of calcifications (calculi) in the ducts and parenchyma of the organ;
- a cavity in the parenchyma, devoid of epithelial lining and containing pancreatic secretion - a false cyst (pseudocyst), may not be single;
- poor circulation in the gland due to chronic venous stagnation;
- disruption of the blood supply to the organ due to pathologies of the splenic and gastric arteries;
- increased hydrostatic pressure in the portal vein – portal hypertension.
A separate genetic disease is cystic fibrosis, in which the pancreatic secretion has a too thick consistency that blocks the ducts. Pancreatic juice does not enter the intestines, enzyme deficiency leads to digestive disorders and lack of nutrients.
As well as rare congenital pathologies: Shwachman-Diamond syndrome and Johanson-Blizzard syndrome, characterized by secretory pancreatic insufficiency in combination with bone marrow dysfunction.
Temporary structural changes provoke:
- overeating and drinking alcoholic beverages;
- acute infectious and inflammatory diseases not related to the pancreas (influenza, ARVI, intestinal infections, pneumonia, etc.);
- side effects of antibiotics, statins and other medications;
- sudden nervous shock.
The non-pathological cause of the moderately diffuse-heterogeneous structure and increased echogenicity is old age. As the body ages, all organs and systems of the body undergo pathological changes.
Congenital cysts on ultrasound of the pancreas in children
Congenital cysts are a consequence of abnormal development of the bile ducts. They can be multiple. Multiple congenital cysts may be found in Hippel–Lindau syndrome, although this usually occurs much more frequently in the older age group rather than in the pediatric population.
Duplication of the pancreas
This pathology on ultrasound in children is quite common and occurs when the ventral and dorsal parts of the pancreas do not merge and each has its own separate excretory duct.
Annular pancreas
An annular pancreas occurs when the abdominal and dorsal segments surround the duodenum in a ring. It causes obstruction at the exit of the stomach, usually in the second part of the duodenum, and appears early in life in children.
Ectopic pancreas
Ectopic pancreas is typically found in the gastric submucosal region and most commonly occurs around the antrum or proximal small intestine. It is associated with other congenital intestinal anomalies, particularly associated with duodenal malrotation and atresia.
Factors influencing the development of diseases
In most cases, pancreatic pathologies develop as a result of chronic pancreatitis. The disease is characterized by a progressive inflammatory process and includes several varieties, which are classified according to the causes of their occurrence.
| View | Cause |
| biliary | violation of the outflow of bile due to inflammatory diseases (cholangitis, cholecystitis), cholelithiasis |
| alcoholic | chronic alcoholism |
| destructive | structural destruction of gland cells |
| medicinal or medicinal | incorrect therapy with diuretics, cardiovascular drugs, antiviral drugs, antibiotics, statins, hormones, psychomotor and psychotropic drugs |
| parenchymal | inflammation of the parenchyma caused by impaired enzyme production |
| pseudotumorous | proliferation of connective tissue, formation of cysts and calcifications |
One of the reasons for the development of dysfunction and the formation of a diffusely heterogeneous structure of the pancreas is considered to be eating behavior: the predominance of fatty foods, smoked foods in the diet, an unhealthy addiction to confectionery, hot spices and seasonings, and abuse of alcoholic beverages. An unhealthy diet provokes a failure of metabolic processes; alcohol and its breakdown products poison the tissues and cells of the gland.
Another factor in reducing functional abilities and changing the morphological characteristics of the gland is prolonged neuropsychological stress (distress) and depressive states. Psycho-emotional instability causes hormonal disruptions that negatively affect the functioning of the entire body, including the hormone-producing pancreas.
Benign pancreatic tumors
Symptoms of benign pancreatic tumors are determined by the type of tumor. Hormonally inactive neoplasias are usually a diagnostic finding because they do not have any symptoms until they reach a significant size and compress neighboring organs, stretch the organ capsule or impair blood flow. Typically, such tumors are detected during instrumental diagnostics of other diseases.
A number of signs allow them to be preliminarily distinguished from malignant ones: the absence of clinical symptoms (including manifestations of intoxication syndrome: weakness, decreased appetite, fatigue, nausea, low-grade body temperature), slow growth with normal levels of tumor markers in the blood. If a large benign tumor of the pancreas compresses neighboring organs, pain is possible. The pain is constant, aching, and can intensify when changing body position; its localization depends on the location of the neoplasia.
Neoplasms of the head of the pancreas are characterized by pain in the right hypochondrium and epigastrium, the body of the organ - in the upper abdomen, the tail - in the left hypochondrium, and lumbar region. The tumor can compress the pancreatic or common bile ducts, which is manifested by signs of obstructive jaundice: icterus of the sclera and skin, itching, dark-colored urine, discoloration of feces. If any part of the intestine is compressed, intestinal obstruction may develop.
Hormone-producing benign tumors have specific characteristics that are determined by the hormone secreted. Insulomas (insulinomas) produce the hormone insulin, which affects blood sugar levels. Signs of such a neoplasm are symptoms of hypoglycemia: weakness, excessive sweating, dizziness, irritability, tachycardia; with a significant decrease in blood glucose, hypoglycemic coma is possible.
Gastrinoma is manifested by the development of multiple gastroduodenal ulcers, refractory to pharmacotherapy. Ulcers can be located in the stomach, bulbar region, and sometimes even in the jejunum. Patients feel intense pain in the epigastric region; Characterized by sour belching and heartburn. Due to hyperproduction of gastrin, a large amount of hydrochloric acid enters the lumen of the gastrointestinal tract, which leads to impaired intestinal motility, damage to its mucous membrane and deterioration of absorption processes.
Symptoms of glucagonoma are determined by increased blood sugar levels. Typically significant weight loss, the appearance of necrolytic migratory erythema (red-brown rash on various parts of the body, mainly in the buttocks, thighs, groin), peeling of the skin, damage to the mucous membranes (gingivitis, stomatitis, vaginitis). Against the background of glucagonoma, diabetes mellitus can develop, the distinctive features of which are the fairly rapid achievement of compensation, often only with diet therapy, as well as the rare development of ketoacidosis, angiopathy and nephropathy.
The main symptoms of the inflammatory process
The symptoms of pancreatitis most often manifest themselves when diffusely heterogeneous changes in the structure of the organ are clearly defined and echogenicity is increased. The main manifestations include:
- heaviness in the epigastric (epigastric) region, nausea, vomiting;
- severe pain syndrome;
- subfebrile (37-38℃) body temperature;
- dyspepsia (painful and difficult digestion);
- intense gas formation;
- constipation (constipation), alternating with diarrhea (diarrhea);
- dry mouth, heartburn.
External symptoms include yellowness of the eyeballs, pallor, loss of body weight, and bloating.
Clinical signs - deviations in test results:
- Complete blood count: decreased hemoglobin and red blood cells, increased ESR, leukocytosis (significant increase in white blood cells).
- Blood biochemistry: high levels of enzymes (amylase, phospholipase, lipase), increased bilirubin, glucose, urea, decreased amount of total protein and protein fractions.
- Coprogram (stool analysis): steatorrhea - excess fat, the presence of undigested food fragments, increased elastase levels.
- Urinalysis: amylasuria (increased amylase), proteinuria (presence of protein), dark color.
When analyzing insulin, elevated levels of the hormone are recorded.