Diagnostics
Diagnosis of pancreatic cancer at the Oncology Center is carried out in a complex that includes physical, laboratory and instrumental research methods:
- Palpation (palpation) of the abdominal organs. An examination of the patient by a doctor can detect an increase in the size of the abdominal organs, which may indicate the development of the disease.
- Ultrasound. The method makes it possible to see the location of the tumor, but is not very effective in the early stages of the disease.
- Endosonography is an ultrasound examination using an endoscope inserted through the mouth. Allows you to study the area under study from the closest possible distance and gives an accurate picture of the location of the tumor.
- X-ray research methods. Using radiographic methods, you can examine the size and location of the tumor, and examine internal organs for the presence of metastases.
- Blood chemistry. Pancreatic cancer changes the biochemical composition of the blood: enzymes and bile acids increase, protein levels decrease.
- CT scan of the abdomen with contrast. Allows you to clearly assess the extent of the tumor, its connection with the great vessels, and provides information about the possibility of radical surgery.
- MRI. Indicated for acid forms of tumor, for mucinous neoplasm of the pancreatic duct.
Classification
The first symptoms of the disease are difficult to notice. The choice of treatment depends on the type of cancer classified by stage. The stages of the disease are determined in patients after examination.
According to the TNM classification, the following stages are distinguished:
- the disease is localized, there are no lesions of the lymph nodes and internal organs - stage zero;
- the tumor has increased in size, but there are no lesions of nearby lymph nodes and organs - 1A and 1B;
- the tumor has spread beyond the organ, internal organs and lymph nodes are not affected - stage 2A. If internal organs and lymph nodes are affected - stage 2B;
- internal organs and lymph nodes are affected, cancer cells are present in the vessels – 3;
- disease with metastases in the abdominal organs – 4.
Treatment
Treatment of pancreatic cancer is a complex task that requires prompt and coordinated actions between doctors and the patient.
In Oncology, the choice of technique depends on the stage of the disease and the presence of metastases. An integrated approach is used , combining chemotherapy and surgery (if the tumor is detected in the early stages). The operation involves partial or complete removal of the pancreas, as a result of which the patient is forced to take digestive enzymes and insulin for the rest of his life. The peculiarity of performing these operations in our oncology center is, on the one hand, maximum radicality (no-touch mobilization), on the other hand, minimal disability. A number of operations for pancreatic cancer are performed through punctures.
Read more about surgical treatment of pancreatic cancer.
Causes of pancreatic tumors
As with any other malignant diseases, pancreatic cancer is the result of a mutation in its epithelial cells. What exactly causes such mutations is still unclear. However, there are a number of factors that increase the risk of developing a tumor:
- various pathologies of the pancreas: chronic pancreatitis (its inflammation), diabetes mellitus, cysts, adenoma (benign tumor), etc.;
- smoking, which impairs blood supply to the pancreas;
- excess body weight associated with hormonal imbalance affecting gland cells;
- liver diseases, primarily cirrhotic lesions;
- peptic ulcer of the stomach and duodenum;
- nonspecific ulcerative colitis, Crohn's disease and other autoimmune diseases of the digestive system;
- improper diet with excessive consumption of sausages, fatty and fried foods, smoked meats, coffee, carbonated drinks, simple carbohydrates (sweets);
- low physical activity;
- various allergic pathologies, such as eczema, atopic dermatitis, etc.;
- oral diseases;
- chronic intoxications associated with poor environmental conditions or occupational hazards;
- tumor diseases of other organs and systems;
- age over 60 years;
- belonging to the Negroid race and male gender;
- some hereditary mutations (for example, in the BRCA2 or PKD1 gene);
- the presence of cancer pathologies in close relatives.
Types of pancreatic cancer
Pancreatic tumors are classified according to the types of cells from which they develop. The following types of tumors are distinguished:
- ductal, which is the most common;
- glandular-squamous;
- squamous;
- giant cell;
- mucinous;
- acinar.
In some cases, the histological origin of the neoplasm cannot be established, and then the tumor is classified as undifferentiated. Loss of differentiation (“specialization” of cells) is a poor prognostic sign. Such neoplasms develop very aggressively and begin to metastasize early.
GASTRINOMA
Clinical manifestations. The disease is characterized by the original Zollinger-Ellison triad: peptic ulcers with atypical localization and a fulminant, aggressive course, extreme hypersecretion of gastric contents and the presence of a non-P islet cell tumor of the pancreas. It can begin as a simple disease and end with the appearance of severe complications (perforation, obstruction, bleeding, refractoriness to therapy). Standard medical and surgical treatment is ineffective. There are cases accompanied by significant diarrhea and steatorrhea.
Diagnostics. Manifestations typical of gastrinoma include high basal secretion rates of VAO/MAO (= or >0.6), hypertrophied gastric mucosal folds, fasting hypergastrinemia (>200 pg/ml) or paroxysmal increase in gastrin levels in response to secretin administration, imaging pancreatic tumor using CT.
Pathology and pathophysiology. Gastrinomas are non-β islet cell tumors of the pancreas that range in size from 2 to 10 mm. There is varying evidence in the literature regarding the malignant potential of gastrinomas, although rates equal to or greater than 90% have been reported. The presence of gastrinomas in the wall of the duodenum is observed. Neoplasms grow slowly and metastasize late; The cause of death is often peptic ulcer disease. Cases of gastrinomas have been described as manifestations of MEA-1 syndrome (Wermer's triad: pituitary gland, parathyroid glands, pancreas), in which the tumors are distinguished by the fact that they are multiple and benign.
Treatment. The original treatment method is gastrectomy. However, the use of histamine H2 receptor blockers and omeprazole with or without proximal selective vagotomy can control the condition of patients with disease that cannot be resected.
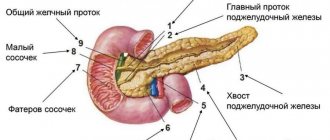
Localization of pancreatic cancer
Anatomically, this organ has three parts, each of which can be affected by a tumor. Accordingly, depending on the location it happens:
- gland head cancer. This is the most common type of pancreatic cancer, accounting for approximately 3/4 of all cases of this disease. Tumors of the head of the gland are usually smaller than tumors of other parts of the organ. But, since the head is located next to the bile ducts, it quickly begins to compress them. Therefore, a common symptom of pancreatic cancer in the early stages is the appearance of a icteric tint to the sclera and skin;
- gland body cancer. Tumors of this location account for about 18% of cases. Large neoplasms in this part of the gland often lead to compression of surrounding vessels, and therefore to disruption of the blood supply to nearby organs. In addition, due to damage to glandular tissue, these tumors are characterized by symptoms of diabetes mellitus;
- tail gland cancer. This is a fairly rare pathology that occurs in approximately 7% of cases of pancreatic malignancy. A special feature of this tumor is that it is difficult to detect on ultrasound, since the tail part of the gland is covered by organs such as the stomach, colon and lower parts of the lung.
OTHER ISLE CELL TUMORS
Lipomas can cause diarrhea, “pancreatic cholera”, WDHA syndrome (water diarrhea, hypokalemia, achlorhydria), 50% of them are malignant. Glkzagonoma is characterized by skin lesions (necrolytic erythema migrans), diabetes, glossitis, anemia, weight loss, depression and venous thrombosis; 75% of glucagon are classified as malignant tumors. The best treatment is resection. Clinical manifestations of somatostatin include diabetes, diarrhea, steatorrhea, achlorhydria, gallstones, malabsorption and abdominal pain. All of these symptoms are attributed to excess somatostatin levels. Streptozocin, dacarbazine, and doxorubicin are most often used in treatment.
Consultation on paid services
Show phone numbers
Treatment at various stages
Specialists at our Oncology Center in Moscow develop treatment regimens for pancreatic cancer on a strictly individual basis. Doctors take into account the histological type of tumor, its location, the patient’s general health, etc. But the most important parameter is the stage of development of the oncological process.
The most effective method of treatment at the moment remains surgery. It is almost always supplemented with pharmacological and radiation therapy. In the early stages of the existence of a malignant neoplasm, it can be eliminated by operations of various scales:
- Whipple operation - removal of the head of the gland;
- segmental resection - removal of the body of the gland with subsequent connection of its remaining parts;
- distal resection – removal of the body and tail of the gland;
- total resection – removal of the entire gland.
These interventions will be effective on:
- stage zero (the tumor is represented by only a certain number of malignantly degenerated cells in one place);
- first stage (the tumor is entirely in the gland, without affecting either the lymph nodes or other organs):
- second stage (the tumor has spread to the tissues and lymph nodes surrounding the gland, but has not yet grown through the walls of neighboring large vessels).
Also, all nearby lymph nodes are often removed for preventive purposes. In addition, at the second stage, those parts of other organs into which the malignant process has managed to spread are also subject to excision: areas of the duodenum, stomach, gall bladder, etc.
At the third (tumor growth through the walls of large vessels) and fourth (metastases in distant organs) stages, palliative surgical interventions are mainly performed. Their goal is to improve the patient’s quality of life and eliminate the most severe symptoms of a pancreatic tumor. These can be operations on:
- removal of those parts of the tumor that put pressure on surrounding organs, disrupting their functions, or compress blood vessels and nerve pathways;
- removal of the largest metastases, often in combination with HIPEC (Hyperthermic Intra Peritoneal Chemotherapy), an innovative method of hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis.
- elimination of obstruction of the biliary tract or intestines, including by applying stents and anastomoses;
- suturing pathological holes in the walls of adjacent hollow organs.
REASONS FOR THE APPEARANCE
In many diseases characterized by chronic inflammation, including chronic pancreatitis, there is a certain risk of developing malignant neoplasms. The most likely reason for this is cell proliferation or genomic damage secondary to inflammation . The exact pathophysiological mechanisms of tumor transformation are still unknown. 4-8% of patients with chronic pancreatitis develop cancer within 20 years of the onset of the disease, which is 15 times higher than the incidence of cancer among other groups. The influence of the cause of pancreatitis on the risk of developing cancer has been clearly proven. For example, tropical pancreatitis, the pathogenesis of which has not yet been determined, is associated with the development of cancer 100 times more often than cases of cancer without underlying pancreatitis.
The influence of various environmental factors, in particular smoking, is possible. The relationship between smoking and the development of chronic pancreatitis, which in turn can transform into cancer, has been proven. The risk of developing cancer in those who smoke one pack of cigarettes per day is 4 times higher than in non-smokers, and when smoking more than 40 cigarettes per day, the risk of developing cancer increases 10 times.
Special importance is attached to the consumption of animal fats and proteins. In countries with high consumption of meat and animal fat (New Zealand, Denmark, USA, Canada), high mortality from pancreatic cancer is noted. At the same time, in Japan, Italy and Israel, where consumption of these products is much lower, mortality rates are lower. In Japan, there was a 2.5-fold increase in the risk of cancer in people who eat meat compared to those who eat seafood. Where a large amount of fish is eaten, cancer is much less likely to occur. The importance of alcohol in the occurrence of cancer has not been proven and, most likely, indirectly: first acute, then chronic pancreatitis, and then transition to cancer.
Conservative treatment
In the treatment of this malignant pathology, the administration of traditional cytostatic drugs is widely used. In addition, oncology today offers more effective means for the treatment of pancreatic cancer. This is, first of all, targeted therapy, in which the active substances of drugs act on specific target molecules of tumor cells, disrupting the processes of their growth and reproduction. Targeted treatment is highly selective, practically without affecting healthy tissue, and therefore produces much fewer side effects. In addition, radiation therapy also demonstrates some effectiveness for pancreatic tumors.
Before surgery, conservative therapy can be prescribed in order to slow down the growth of the tumor as much as possible and reduce its size, destroying as many malignant cells as possible. After surgery, the main point of using these methods is to combat possible metastases and relapses. And in the later stages of the development of the oncological process, when radical operations seem inappropriate, conservative therapy becomes the basis of treatment.
Prevention of pancreatic cancer
The following rules will help reduce the risk of this pathology:
- Quitting smoking and drinking alcohol.
- Reducing the amount of sweets, baked goods and fatty foods in the diet.
- Increasing the consumption of plant fiber.
- Normalization of body weight.
- Constant moderate physical activity.
- Use of personal protective equipment in hazardous industries.
- Periodic preventive examinations by a gastroenterologist for the timely detection and treatment of pathologies that are considered precancerous (pancreatitis, cysts and pancreatic adenomas).
List of sources:
- Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362(17):1605-1617.
- Li D, Xie K, Wolff R, et al. Pancreatic cancer. Lancet. 2004;363(9414):1049-57.
- National Cancer Institute. SEER stat fact sheets: pancreas cancer. NCI website. Published April 28, 2016.
- "Pancreatic Cancer Treatment (PDQ®) Patient Version." National Cancer Institute. National Institutes of Health. 17 April 2014.
- Ryan DP, Hong TS, Bardeesy N (September 2014). "Pancreatic adenocarcinoma". The New England Journal of Medicine. 371(11):1039–49.
- Bazin I.S. Basic principles of management of patients with pancreatic cancer // Effective pharmacotherapy. - 2014. - No. 47. - P. 10-17. — ISSN 2307-3586.
- Kubyshkin V. A. Pancreatic cancer. // Consilium medicum. Vol. 5, No. 8 (2003).
- Lockhart K., Rotenberg M. L. et al. Adjuvant cancer therapy. Per. from English N. D. Firsova (2017)