Pancreatic necrosis is a dangerous pathology when, against the background of acute pancreatitis, parts of the pancreas are destroyed and necrotic areas are formed. This is the most severe complication typical for people of working age. Pancreatic disease disrupts the activity of other organs of the digestive system. The destructive disease leads to the development of multiple organ failure due to impaired fermentation.
It is important to diagnose pancreatic necrosis in a timely manner and begin immediate treatment. According to statistics, the mortality rate for pancreatic necrosis reaches 80%. The prognosis largely depends on adequate treatment tactics and timely surgical intervention.
Causes of the disease
Tissue death is provoked by the accumulated aggressive secretion, which dissolves the pancreas tissue. As a rule, stagnation is combined with an inflammatory process, infection of the body, and other pathologies. The complexity of the disease depends on the degree of damage to the gland. The development of pathology occurs in three stages:
- First, toxemia of a bacterial nature appears. Toxins appear in the blood, worsening the general condition of the patient.
- An abscess is characteristic of the second stage. In addition to the gland, inflammation often spreads to nearby organs.
- Without treatment, purulent changes occur in the tissues of the pancreas and retroperitoneal region.
Normally, enzymes participate in the digestive process only when in contact with bile. If the enzyme secretion does not enter the intestines, it breaks down the gland tissue: first fat cells, then protein compounds. As a result, the pancreas dies.
Research in the field of gastroenterology has shown that pancreatic necrosis is typical for lovers of fatty foods. These are people who allow occasional consumption of alcohol in large doses, as well as those who are prone to constant drunkenness. The first signs of pancreatitis are observed some time after the factors that provoke increased secretion production.
Some patients (about 30%) suffered from cholelithiasis for a long time. Stagnation occurs when the ducts through which the produced secretion is evacuated are blocked. Poor outflow of enzyme fluid may be caused by previous surgeries or injuries to the abdominal cavity.
Types of pathology
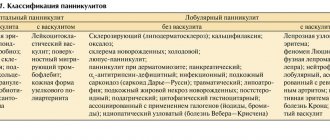
Depending on the pathogenesis, three types of the disease are distinguished:
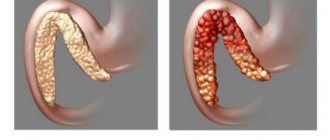
- Fatty pancreatic necrosis, in which the activity of the lipase enzyme is increased, due to which the fatty tissue of the pancreas is destroyed.
- The hemorrhagic form is due to the high activity of elastase, which impedes normal microcirculation, provokes swelling and thrombus formation. The disease is accompanied by internal hemorrhages in the internal organs and retroperitoneal space.
- Mixed form, in which the activity of lipase and elastase is at the same level.
Symptoms of pancreatic necrosis
The main symptom is acute pain of a girdling nature. Painful sensations occur in the back, left hypochondrium, and radiate to the pit of the stomach. The pain is constant, it happens:
- intensive, about 10% of patients are in a state of collapse during attacks;
- average, tolerable pain is experienced by about 44%;
- moderate, such pain is typical for 6% of patients.
The degree of pain depends on the course of the disease and always intensifies after eating. The pain subsides slightly when the patient lies down and presses his legs tightly to his stomach. When the pain radiates to the shoulder, it feels like a heart attack.
Other symptoms of pancreatic necrosis:
- vomiting, which does not bring relief, causes dehydration of the body, the skin becomes dry, and thirst develops;
- due to the concentration of active components in the blood, facial redness occurs;
- with severe pain, the skin becomes pale;
- upon palpation, painfulness of the tense peritoneum is manifested;
- when the level of alpha-amylase, which destroys blood vessels, increases, blue-violet spots appear on the buttocks, abdominal wall, and around the navel, and gastrointestinal bleeding is possible.
Tachycardia gradually develops, consciousness becomes clouded, and delirium is possible. The inflammatory process is accompanied by fever and a decrease in blood pressure.
Pathogenesis
The pathogenesis of pancreatic necrosis is based on a violation of the local protective mechanisms of the pancreas. Large intake of food and alcohol leads to a significant increase in external secretion, overstretching of the pancreatic ducts, and disruption of the outflow of pancreatic juices. An increase in intraductal pressure provokes swelling of the parenchyma, destruction of the pancreatic acini, premature activation of proteolytic enzymes, which lead to massive necrosis of the gland tissue (self-digestion).
Activation of lipase causes necrosis of fat cells, and elastase causes destruction of the vascular wall. Activated enzymes and tissue breakdown products, due to the action of elastase, enter the bloodstream, causing a toxic effect on all organs and tissues. The liver, kidneys, heart, and brain are primarily affected.
Diagnostics
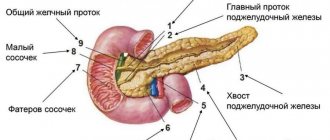
Laboratory diagnostics involves determining the concentration of elastase. A bad sign is progressive growth or a sharp jump in indicators. The amount of enzymes produced by the pancreas is constantly checked in the blood and urine. Instrumental diagnostics includes several hardware examinations:
- Plain radiography of the abdominal cavity is necessary to identify signs of the inflammatory process. When contrast is administered, the condition of fistulas and pancreatic ducts is determined.
- Retrograde cholangiopancreatography (RCPG) allows you to identify the localization of stagnant processes, areas of accumulation of secretions with active enzymes.
- Ultrasound identifies stones in the bile ducts, foci of necrosis, and diagnoses enlargement and changes in the structure of the gland.
- CT and MRI of the pancreas visualize pathological changes in detail and help to accurately determine the localization of necrosis.
- Diagnostic laparoscopy is used in difficult cases. Surgery is necessary to make a diagnosis when surrounding tissues are damaged. Low-traumatic surgical intervention is performed under ultrasound guidance.
Research methods are selected after a visual examination of the patient and anamnesis.
General information
Pancreatic necrosis is the most severe complication of pancreatitis, affecting mainly young able-bodied people, accounting for 1% of all cases of acute abdomen. The pathogenesis of pancreatic necrosis is based on a failure of the mechanisms of internal protection of the pancreas from the destructive action of pancreatic enzymes.
Recently, the number of acute pancreatitis in Russia has been increasing - this pathology comes in second place after acute appendicitis in surgical hospitals. The number of destructive forms of pancreatitis, in particular pancreatic necrosis, is also growing - up to 20-25%. In different clinics, mortality due to destruction of the pancreas reaches 30-80%. The leading way to reduce mortality in pancreatic necrosis is timely diagnosis, hospitalization and early initiation of pathogenetic treatment.
Pancreatic necrosis
Treatment of pancreatic necrosis
The best treatment tactic is urgent hospitalization of the patient in the surgical department for a comprehensive examination and emergency measures. Conservative therapy is effective when there is a chance of recovery. The patient is given drugs that block the production of secretions. A complete refusal to eat for several days is required. Cell nutrition is carried out intravenously. If the bile ducts are blocked and the required amount of bile is not produced, intravenous feeding is indicated for a long time.
Dehydration is eliminated, intoxication is relieved, and if necessary, hemosorption is carried out when the blood is cleansed of toxic components.
Treatment requires rest of the inflamed organ. Analgesia using analgesics provides adequate pain relief. Novocaine blockades are practiced. After taking diuretics, the swelling of the gland subsides, the tension of the pancreatic capsule is weakened. For purulent complications, antibiotics are prescribed.
In a hospital setting, if necessary, anti-shock measures are carried out aimed at relieving pain and improving the outflow of enzymes produced by the gland. Complex therapy also includes drugs that restore the functions of other digestive organs and the cardiovascular system.
Diet
Pancreatitis requires a diet, and pancreatic necrosis of the pancreas requires an even more strict diet.
If surgery is indicated, then a few days before and a few days after it, the patient is transferred to clinical nutrition: intravenous or tube feeding. This is necessary to reduce enzyme activity as much as possible. At the same time, patients receive food enriched with proteins, vitamins and antioxidants.
After recovery, the patient will have to go on a strict diet forever. Alcohol, fatty, fried, smoked, spicy, sweet, canned food, too cold or too hot food are prohibited.
Surgical intervention
When the patient's body does not respond to conservative therapy, more effective treatment methods are required. Operations are performed in severe cases when mechanical restoration of the transport of pancreatic enzymes to the intestine is required. A surgical operation is performed to ensure constant drainage of secretions and resection of destroyed tissue. Foci of necrosis are removed and the ducts are expanded.
Surgical intervention is allowed only after a hardware examination and an accurate diagnosis has been established. Surgical intervention tactics are developed taking into account the assessment of the level of gland necrosis. It is important to consider possible risks:
- the occurrence of complications after surgery;
- possibility of secondary infection.
Punctures, laparoscopy, and laparotomy operations are performed. When fluid accumulates in the abdominal cavity, drainage is practiced.
Information verified by an expert
Vasiliev Vyacheslav Alekseevich
Chief physician. Urologist-andrologist, family doctor, surgeon, ultrasound specialist. Candidate of Medical Sciences Work experience - 30 years
ICD-10
K85 Acute pancreatitis
- Causes of pancreatic necrosis
- Pathogenesis
- Classification
- Symptoms of pancreatic necrosis
- Complications
- Diagnostics
- Treatment of pancreatic necrosis Conservative therapy
- Surgery
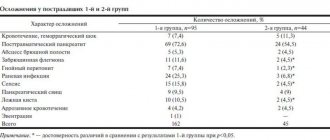
Complications
These pathological changes in the body lead to the formation of multiple organ failure against the background of severe toxic hepatitis, nephritis, carditis, and respiratory disorders. Pancreatic necrosis can be complicated by shock, peritonitis, abdominal abscess, and gastrointestinal bleeding.
Local complications often include abscess, cyst or false cyst of the pancreas, enzyme deficiency, fibrosis of the pancreas, phlegmon of the retroperitoneal tissue, gastrointestinal ulcers, thrombosis of the portal and mesenteric veins.
Prognosis and prevention
Making a prognosis for patients with pancreatic necrosis is a very difficult task, as it depends on many circumstances. The prognosis is significantly worsened in the presence of one or more of the following factors: age over fifty-five years, leukocytosis more than 16x109/l, hyperglycemia, hypocalcemia, metabolic acidosis, arterial hypotension, increased levels of urea, LDH and AST, significant loss of fluid from the bloodstream into the tissue . The presence of seven of these criteria ensures 100% patient mortality. Prevention of pancreatic necrosis involves timely seeking medical help and early initiation of treatment, including surgery.