Symptoms of the disease
Diseases of the pancreas are accompanied by:
- heaviness in the left hypochondrium;
- girdle pains of varying severity (they can be aching, stabbing, piercing, burning), which can occur both after eating and independently of it;
- loss of appetite and weight loss;
- frequent belching;
- nausea and vomiting;
- heartburn;
- sour taste in the mouth;
- flatulence;
- indigestion (constipation or diarrhea);
- vitamin deficiency;
- dry skin;
- brittle nails;
- cold sweat;
- general weakness.
With necrosis, in addition to the above symptoms, the temperature rises and blue spots appear on the stomach and sides.
In the absence of timely treatment of pancreatic diseases, pathological changes occur in the liver, which leads to the development of jaundice and dystrophy.
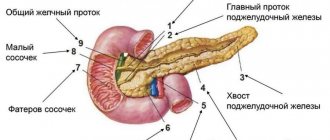
The pancreas and its role in digestion
Ultrasound as a diagnostic method
The location of the pancreas is usually not of much interest to a person until symptoms of its pathology appear. But the appearance of heaviness in the left side, intensifying after eating, girdle pain, bloating and nausea are signals to see a doctor without delay.
This raises the question, which doctor treats the pancreas? As the name of the organ itself suggests, it is located under the stomach, on the left side, and is part of the human digestive system. Therefore, a gastroenterologist is the specialist to whom it is logical to turn when problems arise.
Enzymes synthesized by the pancreas enter the duodenum, where they break down nutrients that pass through the stomach into microelements. The pancreas performs not only the function of external secretion (synthesizes pancreatic juice for digesting food), but also internal - it regulates the metabolism of carbohydrates, fats and proteins through the production of a number of hormones.
The endocrine (internal) function of the pancreas is the production of hormones and the regulation of metabolic processes: carbohydrate, fat and protein. Normally, it produces up to 1 liter of juice every day, as well as the enzymes amylase (breaks down carbohydrates), lipase (affects the absorption of fats), and trypsins, which are responsible for the digestion of protein foods.
Also, the endocrine function of the pancreas is to produce the hormones insulin and glucogen. Under the influence of insulin, the human body is able to absorb carbohydrates and glucose. The hormone glucagon protects liver cells from fatty degeneration. Thus, if the production of the hormones insulin and glucagon is disrupted, it is necessary to consult an endocrinologist.
The role of the pancreas is the most important in the activity of the entire human digestive tract: disturbances in its work lead to disruption of the entire state of health.
How to detect the disease?
First, the doctor examines the patient, palpates, asks about symptoms, and studies the medical history.
Then he gives a referral for instrumental and laboratory diagnostics:
- blood tests: general, biochemical and glucose;
- urine amylase test;
- coprogram;
- radiography;
- endoscopy;
- ultrasound examination (ultrasound);
- angiography;
- retrograde cholecystopancreatography;
- electrocardiography (symptoms of the abdominal form of infarction are similar to those of pancreatitis);
- computer and magnetic resonance imaging (CT and MRI).
When should you contact an endocrinologist?
The pancreas produces hormones vital to the human body: glucagon, insulin and somatostatin. All of them directly affect the metabolism of glucose in the blood. Inflammation of this organ can lead to its malfunction or even tissue necrosis, which threatens the development of diabetes mellitus. That is why consultation with an endocrinologist in such cases is vital. The doctor will register the patient with a dispensary, select the required dosage of insulin, if necessary, or prescribe other hormone replacement therapy.
The pancreas is a unique organ that not only participates in the digestion process, but also synthesizes vital hormones
Who to contact?
Depending on the severity of symptoms, you can contact:
- therapist;
- gastroenterologist;
- endocrinologist;
- surgeon;
- oncologist.
If the patient cannot independently choose the right doctor, then he should make an appointment with a therapist, who, if necessary, will refer him to a specialist.
Therapist
The therapist treats chronic pancreatitis without exacerbations and other diseases of the pancreas on an outpatient basis. He prescribes medication: selects analgesics and drugs that help digest food. If the therapist fails to cope with the disease, he refers the patient to a gastroenterologist.
Gastroenterologist
In case of acute pancreatitis, the patient is hospitalized and treated by a gastroenterologist. First of all, the specialist will select a strict diet. In the first few days, the patient drinks only alkaline water to restore the functioning of the organ. Then you can gradually eat light food.
The doctor will also prescribe special enzymes that will facilitate the work of the pancreas and help return it to normal, probiotics, vitamin complexes, and immunomodulators.
Endocrinologist
You will have to contact this specialist if blood tests show an increased glucose concentration, which may be a consequence of diabetes mellitus. Once the diagnosis is confirmed, the endocrinologist will prescribe a diet and insulin administration, and select the required dosage of the hormone.
Surgeon
During an attack of acute pancreatitis or exacerbation of chronic pancreatitis, the patient is admitted to the surgical department. First, the surgeon applies conservative treatment: puts in IVs, prescribes painkillers and drugs that regulate the secretion of digestive enzymes. But if complications arise, he resorts to surgery. After the elimination of acute symptoms, further therapy is carried out by a gastroenterologist.
In case of extensive necrosis, the patient is taken to the intensive care unit or intensive care unit, where a resuscitator, together with a surgeon, treats him.
Oncologist
If malignant tumors are discovered during the examination, the patient is referred to an oncologist. He will prescribe a course of chemotherapy or recommend surgery.
After inpatient treatment, the patient is registered with a local therapist, who monitors his condition and periodically refers him to specialists.
Consultations with a doctor online Taking care of your health is a life priority for everyone.
Communicate with doctors online and receive qualified assistance without leaving your home. Try it Please note! The information on this page is provided for informational purposes only. To prescribe treatment, you must consult a doctor.
Causes of pancreatitis.
- Heredity.
- Bad habits: alcohol and smoking abuse. More than half of cases of pancreatitis are the result of an unhealthy lifestyle.
- Disorders in the human immune system - autoimmune problems.
- Blockage of the pancreatic duct or common bile duct.
- Damage to the ducts and pancreas during surgical procedures.
- Postoperative complications.
- Presence of Reye's syndrome.
- Presence of hemolytic uremic syndrome.
- Presence of hyperparathyroidism.
- The presence of hypertriglyceridemia, that is, a high concentration of triglycerides in the body.
- Poor blood circulation of the pancreas.
- Trauma to the pancreas as a result of an accident.
- Viral infections, including mumps and campylobacter.
- Diseases of the duodenum, small and large intestines, accompanied by constipation, such as enteritis, enterocolitis, diverticula.
- Long-term uncontrolled use of drugs, for example, estrogens, corticosteroids, thiazide diuretics and azathioprine.
- Metabolic disorders, especially fats.
- Poor quality nutrition, overeating.
Men and women aged 30–40 years are at risk of developing pancreatitis. Moreover, men here prevail over women.
People who abuse alcohol, smoking, or drug addiction are at greater risk of developing pancreatitis than people who are not exposed to bad habits.
In many cases, genetic predisposition becomes a decisive factor in the development of pancreatitis.
Pancreatitis leads to scarring of the pancreas.
In this condition, the pancreas stops producing the required amount of digestive enzymes. As a result of disruption of the functioning of the pancreas, it becomes impossible to digest certain microorganisms, in particular fats.
If the part of the pancreas that produces insulin is damaged, diabetes can develop.
If the therapist referred to an oncologist
Many people shudder at the mere mention of the word “oncologist.” But do not panic if the therapist has given a referral to this specialist, because a problem detected in time can be completely solved with the help of modern treatment methods.
Untimely treatment of pancreatitis may well lead to tumor diseases. They can be detected using ultrasound, CT, MRI and other studies that are carried out upon patient admission to the hospital. Cysts or cancerous tumors can form in the pancreatic tissue. In such cases, consultation with an oncologist is strictly necessary, because only he can establish an accurate diagnosis and prescribe adequate treatment. If necessary, a decision is made on surgery and chemotherapy.
Inflammation of the pancreas is a serious disease that requires at least consultation with a specialist who treats the organs of the gastrointestinal tract. You should not delay consulting a doctor, because in addition to the main illness, concomitant diseases pose a huge danger, the main one of which is diabetes.
Symptoms of pancreatitis
The main symptom of pancreatitis is severe pain. Along with it, nausea, vomiting, a slight increase in temperature, flatulence, stool disorders and some other symptoms may be observed.
Abdominal pain
The main symptom of acute pancreatitis is severe pain, which usually begins in the left side and then becomes encircling. The pain is not relieved either by antispasmodics (“no-spa” and analogues) or by painkillers (analgesics). Lying on your back may intensify. An attack of pain with pancreatitis is usually observed after eating or drinking alcohol. When eating against the background of pain, the pain intensifies.
Vomit
The onset of acute pancreatitis may be accompanied by bouts of vomiting. Vomit with pancreatitis usually contains bile. During this period, you must completely stop eating.
More about the symptom
Temperature
During an attack of pancreatitis, the temperature may rise to 37.5°C.
More about the symptom
Flatulence
The attack disrupts intestinal motility. This leads to bloating.
More about the symptom
Stool disorder
The lack of necessary enzymes does not allow food to be properly digested, which causes stool upset.