The pancreas is a unique organ of the digestive system that simultaneously performs two functions:
- endocrine – internal secretion of hormones (insulin, glucagon, somatostatin, vasoactive intestinal peptide) and pancreatic polypeptide;
- exocrine - external secretion of pancreatic juice, the basis of which are digestive enzymes.
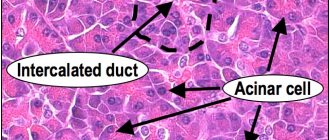
Parenchyma (organ tissue) consists of cells and stroma, including excretory ducts and blood vessels. Normally, the parenchyma should be homogeneous (uniform).
A heterogeneous, otherwise diffusely heterogeneous structure of the pancreas indicates the presence of pathological processes, dysfunction, and possible cell necrosis.
Detection of deviations
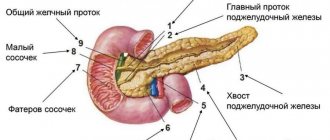
The primary methods for diagnosing pancreatic diseases are laboratory tests and ultrasound. Among the ultrasound parameters, the main ones are echogenicity (conductivity or the degree of reflection of ultrasound, indicating tissue density), contours and structure of the organ. Next, the sizes of the constituent parts of the gland (body, head, tail) are examined.
Normal indicators of an ultrasound examination of an adult
| Echogenicity | Outlines | Structure | Body | Head | Tail | Neoplasms |
| normal or isoechoic | clear | homogeneous | 2.5 cm | 3.5 cm | 3 cm | none |
Homogeneity on an ultrasound monitor is defined as a uniform gray coloration of the entire organ with a fine-grained or coarse-grained echostructure. The degree of ultrasound conductivity is determined by the presence and volume of liquid:
- isoechoicity – average, normal ultrasound reflection (gray parenchyma);
- hypoechogenicity – reduced conductivity (dark tissue);
- hyperechogenicity – increased conductivity (visualized in shades of white);
- anechoicity - ultrasound is not reflected (black parenchyma).
A diffuse-heterogeneous structure is most often characterized by hyperechogenicity of varying intensity, which indicates the development of pathological processes (inflammatory, tumor, fibrous, necrotic, etc.).
Diffusely heterogeneous changes mean a uniform violation of the homogeneity of the structure throughout the gland. Efficient parenchyma cells are gradually replaced by adipose or connective tissue that does not bear a functional load.
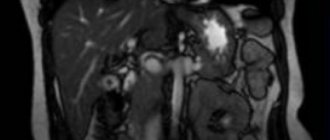
Ultrasound detection of a diffusely heterogeneous structure of the pancreas is not a diagnosis, but a sign of disorders indicating a particular disease. The patient may be prescribed additional diagnostic examinations (retrograde cholangiopancreatography, magnetic resonance and computed tomography).
Features of preparation for ultrasound
To objectively identify structural changes in the pancreas before performing an ultrasound, the patient must:
- 2-3 days before the examination, avoid alcohol-containing drinks and foods that cause intense gas formation (legume dishes, cabbage, fermented milk drinks, baked goods);
- the day before the procedure, start taking carminative drugs (Espumizan, activated carbon).
The fasting regime before an ultrasound of the abdominal organs is 8-12 hours.
Reasons for changes
Changes in the structure of the pancreas against the background of hyperechogenicity accompany acute inflammation, edema, fibrosis, and fatty deposits. The main diseases diagnosed based on the results of an ultrasound examination:
What does an ultrasound of the pancreas show?
- an increase in the volume of intracellular fat and replacement of parenchyma with adipose tissue - steatosis;
- accumulation of fluid (edema) is not an independent pathology, but a consequence of diseases of the gland itself, the duodenum, hepatitis, helminthic infestations, stones in the gall bladder, etc.;
- benign tumors (gastrinoma, insulinoma, glucagonoma);
- proliferation of atypical cells – pancreatic cancer;
- acute and chronic inflammation of the organ - pancreatitis;
- synchronous inflammatory damage to adjacent organs of the hepatobiliary system (pancreas and gallbladder) - cholecystopancreatitis;
- motor-tonic dysfunction of the gallbladder and bile duct sphincters - biliary dyskinesia;
- death of gland cells - pancreatic necrosis;
- diabetes mellitus (insulin-dependent type 1 with hereditary predisposition);
- proliferation of connective tissue and replacement of its working cells – fibrosis;
- pancreolithiasis - the presence of calcifications (calculi) in the ducts and parenchyma of the organ;
- a cavity in the parenchyma, devoid of epithelial lining and containing pancreatic secretion - a false cyst (pseudocyst), may not be single;
- poor circulation in the gland due to chronic venous stagnation;
- disruption of the blood supply to the organ due to pathologies of the splenic and gastric arteries;
- increased hydrostatic pressure in the portal vein – portal hypertension.
A separate genetic disease is cystic fibrosis, in which the pancreatic secretion has a too thick consistency that blocks the ducts. Pancreatic juice does not enter the intestines, enzyme deficiency leads to digestive disorders and lack of nutrients.
As well as rare congenital pathologies: Shwachman-Diamond syndrome and Johanson-Blizzard syndrome, characterized by secretory pancreatic insufficiency in combination with bone marrow dysfunction.
Temporary structural changes provoke:
- overeating and drinking alcoholic beverages;
- acute infectious and inflammatory diseases not related to the pancreas (influenza, ARVI, intestinal infections, pneumonia, etc.);
- side effects of antibiotics, statins and other medications;
- sudden nervous shock.
The non-pathological cause of the moderately diffuse-heterogeneous structure and increased echogenicity is old age. As the body ages, all organs and systems of the body undergo pathological changes.
Echogenicity of the pancreas
When performing an ultrasound, the echogenicity of pancreatic tissue is compared with the echogenicity of the liver. Normally, it should be of medium echogenicity, i.e. comparable in shade to a healthy liver. However, this characteristic varies widely.
If the pancreas turns out to be lighter or darker than the liver, this may be a sign of pathology. But the echogenicity characteristic alone does not mean that the patient necessarily has some kind of disease. The doctor must evaluate other ultrasound parameters of the organ, as well as the presence or absence of complaints from the patient, changes in his laboratory tests. And only on the basis of all this, an experienced doctor makes a final diagnosis and prescribes the necessary treatment.
Increased echogenicity on ultrasound of the pancreas
Increased echogenicity of the pancreas on ultrasound may indicate the presence of the following diseases:
- lipomatosis of the gland,
- chronic pancreatitis,
- sclerosis of the gland in elderly and senile people.
As a rule, in the absence of chronic pancreatitis, patients with this symptom do not present any complaints from the gastrointestinal tract.
Lipomatosis develops as a result of the replacement of normal organ tissue with adipose tissue. Typically, this change is observed in patients suffering from obesity, type 2 diabetes and is part of the metabolic syndrome. Such patients rarely survive to develop pancreatic insufficiency, since the reserves of the exocrine function of the pancreas are quite large, and more often they die from pathology of the cardiovascular system.
This image shows the pancreatic duct (indicated by the abbreviation “pd” in the image). You may notice that it is lighter than nearby areas (increased echogenicity). The diagnosis was pancreatic lipomatosis.
In chronic pancreatitis, increased echogenicity of the pancreas due to fibrosis is recorded, however, such areas are more often identified as light spots and located in isolation. The occurrence of calcifications and stones in the gland tissue also contributes to increased echogenicity.
In old age, the echogenicity of the pancreas is increased as a result of its sclerosis, replacement with fibrous tissue. The increase in echogenicity can be strongly or moderately expressed. A moderate increase most likely means the presence of some temporary factors affecting the reflectivity - diet, diet, long-term cold moment of examination. With a repeated echographic examination, as a rule, the picture becomes normal. If a significant increase in echogenicity is detected, then most likely there is a serious pathology that requires further examination and treatment.
Decreased echogenicity of the pancreas
Hypoechoic pancreatic tissue may also indicate the presence of pathology. In mild cases of acute pancreatitis, swelling and an increase in the size of the gland are observed, which is manifested by a pronounced decrease in echogenicity. In this case, the patient is bothered by intense abdominal pain, and his blood and urine tests show an increase in pancreatic enzymes.
This patient, who complains of abdominal pain, has pronounced hypoechogenicity of the pancreas, which indicates acute pancreatitis.
In chronic pancreatitis, which develops due to alcohol abuse, the pancreatic parenchyma can also become hypoechoic. But at the same time, unevenness of its contours, expansion of the main pancreatic duct or alternating light areas of fibrosis are also revealed.
In some cases, “hypoechoic parenchyma” may be mistakenly perceived and in fact represent a sharply dilated main pancreatic duct, which can occupy almost the entire volume of the gland against the background of its atrophy in the late stages of chronic pancreatitis.
In adolescence and childhood, quite often the normal pancreas has a pronounced hypoechoic structure, which can be mistakenly interpreted as edema in acute pancreatitis. The difference is the normal size of the pancreas.
Mixed echogenicity on ultrasound of the pancreas
The average echogenicity of the pancreas (pancreas) is characterized by a homogeneous structure. But quite often, ultrasound reveals mixed echogenicity, manifested by a heterogeneous, spotty structure with alternating zones of increased and decreased echogenicity. This picture is, as a rule, not constant and can change with each subsequent examination under the influence of a variety of reasons.
It can be detected in chronic pancreatitis, with focal forms of lipomatosis, metastases, as well as with inadequate preparation for the study and the presence of a large amount of gas in the intestine, which shields the pancreas area.
What to do if changes in the echogenicity of the pancreas are detected?
If an ultrasound examination reveals a change in the echogenicity of the pancreas in a patient against the background of any complaints from the gastrointestinal tract, this requires further thorough examination and identification of the cause.
To do this, first of all, you need to take a general and biochemical blood and urine test. And then the gastroenterologist collectively evaluates all the data obtained and either, if the picture is unclear, prescribes additional examination methods or a repeat ultrasound, or, when making a diagnosis, prescribes treatment and diet.
In any case, having received the results of an ultrasound scan of the pancreas with any deviations from the norm, you need to consult with a specialist, and not try to deal with the indicators of echogenicity of the pancreas on your own.
Factors influencing the development of diseases
In most cases, pancreatic pathologies develop as a result of chronic pancreatitis. The disease is characterized by a progressive inflammatory process and includes several varieties, which are classified according to the causes of their occurrence.
| View | Cause |
| biliary | violation of the outflow of bile due to inflammatory diseases (cholangitis, cholecystitis), cholelithiasis |
| alcoholic | chronic alcoholism |
| destructive | structural destruction of gland cells |
| medicinal or medicinal | incorrect therapy with diuretics, cardiovascular drugs, antiviral drugs, antibiotics, statins, hormones, psychomotor and psychotropic drugs |
| parenchymal | inflammation of the parenchyma caused by impaired enzyme production |
| pseudotumorous | proliferation of connective tissue, formation of cysts and calcifications |
One of the reasons for the development of dysfunction and the formation of a diffusely heterogeneous structure of the pancreas is considered to be eating behavior: the predominance of fatty foods, smoked foods in the diet, an unhealthy addiction to confectionery, hot spices and seasonings, and abuse of alcoholic beverages. An unhealthy diet provokes a failure of metabolic processes; alcohol and its breakdown products poison the tissues and cells of the gland.
Another factor in reducing functional abilities and changing the morphological characteristics of the gland is prolonged neuropsychological stress (distress) and depressive states. Psycho-emotional instability causes hormonal disruptions that negatively affect the functioning of the entire body, including the hormone-producing pancreas.
The main symptoms of the inflammatory process
The symptoms of pancreatitis most often manifest themselves when diffusely heterogeneous changes in the structure of the organ are clearly defined and echogenicity is increased. The main manifestations include:
- heaviness in the epigastric (epigastric) region, nausea, vomiting;
- severe pain syndrome;
- subfebrile (37-38℃) body temperature;
- dyspepsia (painful and difficult digestion);
- intense gas formation;
- constipation (constipation), alternating with diarrhea (diarrhea);
- dry mouth, heartburn.
External symptoms include yellowness of the eyeballs, pallor, loss of body weight, and bloating.
Clinical signs - deviations in test results:
- Complete blood count: decreased hemoglobin and red blood cells, increased ESR, leukocytosis (significant increase in white blood cells).
- Blood biochemistry: high levels of enzymes (amylase, phospholipase, lipase), increased bilirubin, glucose, urea, decreased amount of total protein and protein fractions.
- Coprogram (stool analysis): steatorrhea - excess fat, the presence of undigested food fragments, increased elastase levels.
- Urinalysis: amylasuria (increased amylase), proteinuria (presence of protein), dark color.
When analyzing insulin, elevated levels of the hormone are recorded.
Is this feature dangerous?
The granular structure is only a sign of deviation, but not an independent disease. If the structural feature of the gland was discovered in a timely manner, the prognosis is very favorable. After a course of treatment, it is possible to restore the structure of the organ and get rid of granularity.
If the granularity of the pancreas is detected too late, when it is completely covered with large grains, there is a high risk of developing pancreatic necrosis, that is, tissue necrosis. In this situation, surgical intervention is necessary, during which the entire organ or part of it will be removed.
We recommend that you read: Increased echogenicity of the pancreas.