Symptoms of peritonitis are a set of signs of the development and course of a pathological process in the abdominal cavity. Peritonitis is defined as inflammation of the peritoneum as a result of infection, disruption of the integrity of internal organs or the abdominal cavity itself, or ingress of foreign bodies and fluids, such as the contents of hollow organs. Pathology has a number of clinical, objective and subjective signs, which the doctor relies on when conducting an initial diagnosis of the patient’s condition with suspected peritonitis. It is very important to establish as accurately as possible the clinical picture, intensity, duration and localization of symptoms in order to recognize specific forms of peritonitis and understand what therapeutic measures need to be taken.
First manifestations
It is important to know the first suspicious symptoms and manifestations of peritonitis, because with the development of inflammation of the peritoneum, literally every minute before the start of preparation for surgery matters for the patient. The longer the moment of entering a medical facility is delayed, the higher the possibility of an unfavorable outcome.
Content:
- First manifestations
- Main symptoms
- Symptoms of a ruptured appendix
- Symptoms of bile peritonitis
- Manifestations in women (pelvioperitonitis)
- Manifestations in children
- Ultrasound signs
- What does acute peritonitis look like?
- Signs of chronic disease
The clinical picture is represented by general and local manifestations. The appearance of general symptoms is due to increasing intoxication. Such signs are not specific and do not provide sufficient grounds for making a diagnosis. The patient experiences fever, tachycardia, general weakness, nausea, chills, body aches, and increased irritability. Considering that peritonitis is always a secondary syndrome, the patient exhibits symptoms of the underlying disease, be it appendicitis, peptic ulcer, cholecystitis or other diseases.
As for local symptoms, they are formed as a response to irritation of the layers of the peritoneum, foreign elements that have entered there - bacteria, fluids and other agents.
The first complaint that should alert you is constant and intense pain in the abdomen. The pain does not subside over time, but tends to intensify when changing position. In this case, the patient takes a forced position lying on his back or side, bends and pulls his knees to his stomach. Upon examination, strong tension in the anterior abdominal wall and symptoms of peritoneal irritation (Mendel syndrome, Shchetkin-Blumberg syndrome) are clearly expressed.
In addition, the patient complains of increased body temperature, dry mouth, constant nausea, and repeated vomiting. There may be dizziness, headache, darkening of the eyes.
It should be noted that it is almost impossible to establish a reliable diagnosis at home without resorting to a medical examination.
Main symptoms
Regardless of the form of the course and the degree of spread of the pathology in the peritoneum, there are a number of symptoms that are always present in a patient diagnosed with peritonitis. At the same time, they can appear with different intensities and different durations; they look brighter or blurry.
The picture of the main symptoms of peritonitis can be divided into three groups:
- local: muscle protection, accumulation of exudate and pain;
- functional disorders of the digestive and urinary organs;
- general signs caused by intoxication.
Acute abdominal pain is the most typical sign of developing inflammation of the peritoneum. It manifests itself especially strongly in perforated peritonitis. With inflammation not associated with a violation of the integrity of the walls of internal organs, the pain is less pronounced and intensifies gradually.
A rupture (perforation) of the wall of a hollow organ is usually accompanied by a sharp, shooting pain, when the patient tries to lie down and not move, since the slightest movement causes severe pain. Movement of the peritoneum during breathing and touching the anterior wall of the abdomen are also painful. Sometimes the pain is sharp and severe so much that the victim loses consciousness and his pulse becomes thread-like.
Pain caused by a wall breakthrough is first localized in the area where the rupture occurred, that is, at the point of peritonitis, then the localization shifts. Perforated appendicitis may be accompanied by pain in the epigastric region. The pain lasts in this place for quite a long time, and in the primary focus it gradually fades.
When the pain syndrome is particularly severe, the patient stops breathing through the stomach, breathing becomes frequent and shallow.
Even the most intense pain can subside after 12-36 hours - this trend is a sign of the transition of the reactive stage of peritonitis to the toxic stage.
If pain occurs when urinating, it means that the inflammation has moved to the area of the peritoneum covering the bladder.
During an acute course, pain often radiates to the area of the shoulder, heart, and chest.
Muscle defense is the constant tension of the abdominal muscle wall, which appears either along with pain or a little later. The state of muscle protection is due to reflex muscle contraction, which accompanies inflammation of the peritoneum.
The presence of liquid exudate is a common sign of peritonitis. The fluid that accumulates in the abdominal cavity can be purulent, fecal, serous, fibrinous, hemorrhagic, that is, contain various impurities. The presence of exudate can be detected using the abdomen. In this case, the sound of the blow is shortened in the lateral areas of the abdomen, and tympanitis is noted on the anterior wall.
Typical functional disorders that usually accompany peritonitis:
- hiccups and belching;
- vomit;
- retention of stool and flatulence;
- flatulence and diarrhea (rare).
Vomiting almost always begins along with pain, or joins the picture of symptoms some time after the development of intense pain. Vomit contains remnants of undigested food, gradually its volume decreases, and the consistency becomes viscous, thick, with an admixture of bile. If peritonitis is ulcerative in nature, the patient’s vomit contains blood or “coffee grounds.” Over time, the frequency of vomiting increases, and the patient begins to experience excruciating thirst because of this. It is impossible to quench the feeling of thirst, since any liquid taken is immediately rejected by the body.
If a patient has hiccups, then they are persistent and cannot be stopped. The cause of the symptom is irritation of the phrenic nerve, or the area of the peritoneum that lines the diaphragm.
Paresis and subsequent paralysis of the intestines is another typical symptom of inflammation; it develops as a result of stool retention, when gases do not pass away, but accumulate in the intestines, causing flatulence and bloating. The abdomen swells, its skin tightens, becomes smooth and shiny. With percussion, tympanitis is heard, and the dullness of sound in the hepatic zone disappears.
The development of paresis causes further intestinal paralysis, paralytic obstruction, and the onset of fecal vomiting, which greatly complicates the patient’s condition.
Paresis can spread to the bladder, in which case urinary retention develops.
General symptoms characteristic of different types of peritonitis characterize the degree of change in the state of the central nervous system caused by intoxication. The development of peritonitis is accompanied by disturbances in cardiovascular activity, dehydration and disturbances in water and electrolyte balance. It should be noted that exhaustion, severe pain and thirst, as well as a general feeling of weakness leave a specific imprint on the victim’s appearance - his facial features become sharper, his eyes seem to sink into the skull, and become dull. A dangerous symptom of intoxication is sleep disturbance, insomnia accompanied by periods of euphoria.
Cardiovascular disorders are manifested by a slowing of the pulse, its drop to threadlike, and then a gradual increase, sometimes to significant, critical levels, cardiac arrhythmia develops. As the general condition worsens, blood pressure decreases.
The next symptom accompanying peritonitis is fever and chills, but in some cases the temperature may remain normal.
In a typical febrile course, the temperature quickly reaches 38-39 degrees, and remains at this level, practically without decreasing.
With perforated peritonitis, body temperature may drop sharply after perforation, below normal, but after some time fever still develops.
If fever, together with other syndromes, preceded the development of peritonitis, the onset of inflammation only intensifies its manifestations, for example, if we are talking about postpartum or septic peritonitis.
Fever is most typical of common purulent peritonitis. In such cases, the temperature curve fluctuates from low to high values. It should be noted that one should not rely on body temperature when making a diagnosis of peritonitis. However, such a parameter as a significant difference between the readings measured in the axillary region and rectally has significant diagnostic significance. With diffuse peritonitis, the difference reaches 2-3 degrees.
In addition, the acute course of peritonitis is accompanied by a change in the functional capacity of the kidneys, a decrease in diuresis is noted, and renal failure develops.
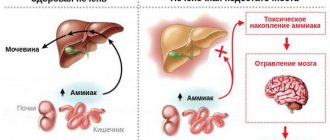
If pathological processes affect the liver, the patient may develop jaundice and the detoxification ability of the organ is impaired.
Treatment
Treatment of peritonitis is always surgical, with mandatory preoperative drug preparation.
The latter is aimed at replenishing the balance of fluids, salts and normalizing the patient’s condition, as well as adequate pain relief and normalizing blood pressure. During surgery for peritonitis, the source of infection is eliminated, pus and peritoneal effusion are removed, the abdominal cavity is washed with antiseptic solutions and drained. Postoperative management of the patient includes a course of powerful antibiotic therapy, drips with detoxification solutions, medications to support the functioning of the cardiovascular system, respiratory system and nervous system.
Author:
Pugonina Tatyana Alekseevna, Therapist
Symptoms of a ruptured appendix
The rupture of the appendix is preceded by its blocked and infected state, against which gangrene forms. As a result, the appendix literally ruptures, and its contents enter the peritoneum. The longer the time passes from the moment of rupture, the stronger the symptoms appear and the patient’s general condition worsens.
The main symptom of peritonitis with a ruptured appendix is severe and sharp pain. Initially, the sensation appears on the right side of the lower abdomen, has an increasing character, and manifests itself in impulses. After some time, the pain may change its location and spread throughout the abdomen.
The moment of rupture is accompanied by:
- an attack of severe shooting or cutting pain that covers the entire lower abdomen;
- severe nausea and persistent vomiting;
- increase in body temperature.
It should be noted that if the patient did not seek help, but decided to wait out the condition in the hope that it would improve on its own, some relief of symptoms may be possible. When peritonitis passes from the reactive to the terminal stage, paralysis of the nerve endings occurs, due to which the manifestation of pain is somewhat dulled. However, this process cannot be called an improvement - on the contrary, a lull indicates a worsening of the patient’s condition.
Symptoms of bile peritonitis
The course of the pathology and its manifestations directly depend on the rate of penetration and volumes of bile entering the abdominal cavity, as well as the area of infection. With slow effusion, the patient develops chronic or subacute peritonitis, in which the symptoms are mild. The rapid entry of a large amount of bile provokes the manifestation of acute peritonitis. The development of pathology goes through several stages, the symptoms of which have their own distinct features.
The formation of the disease and the first obvious manifestation of the clinical picture occurs several hours after the start of the release of bile from the biliary tract. During this period of time, inflammation has time to develop in the peritoneum, and serous or fibrous-serous exudate begins to accumulate. Severe cutting or stabbing pain suddenly appears, radiating to the right hypochondrium, right scapula or collarbone.
Simultaneously with the pain, or a little later, reflex vomiting, belching and heartburn occur. After this, a strong deterioration in well-being occurs, the patient is literally unable to stand on his feet, he tries to take a position lying on his side or on his back, pulling his knees to his stomach. The face is pale, the features are pointed, cold sweat and shortness of breath appear. Body temperature rises, which indicates the onset of fever; palpation of the abdomen is accompanied by severe diffuse pain.
The toxic stage begins on the second day after the first symptoms appear. The patient's state of intoxication increases, inflammation becomes generalized, and overall health deteriorates: stupor-stupor is observed, interspersed with periods of excitement, dry mouth appears, excruciating thirst against the background of unabated vomiting. The vomit that comes out is brown in color and has a strong, unpleasant odor. The skin is moist, cool, and becomes bluish. The patient's breathing is frequent and shallow, while he tries not to breathe from his stomach. Body temperature reaches 39-40 degrees. On palpation, strong tension in the anterior abdominal wall is felt. Intestinal paresis is manifested by constipation, difficult passage of gases.
The terminal phase of biliary peritonitis begins 2-3 days later and is very difficult. The patient has a state of stupor, sometimes he screams, and practically does not react to external stimuli. The face takes on an earthy tint, the eyes are sunken, and the facial features are very pointed. Despite severe bloating, there is no reaction to palpation or any manifestations of peristalsis.
Manifestations in women (pelvioperitonitis)
Female peritonitis has its own characteristics, as it can be associated with complications after childbirth, with a cesarean section or instrumental examination of the uterine cavity, as well as with inflammatory processes in the fallopian tubes, uterus or ovaries.
Peritonitis in women can be limited or widespread, but is always a secondary condition caused by certain pathological processes. If the uterus is perforated, ruptured, or after a cesarean section, the development of peritonitis in the patient takes no more than two days. If an infection is introduced during childbirth or during an abortion and its lymphogenous spread, peritonitis can develop by 7-8 days after the intervention.
The course of peritonitis in obstetrics is divided into typical stages: reactive, toxic and terminal.
Initially, the woman experiences obvious intoxication, but if before the onset of the pathology the patient underwent intensive antibiotic therapy, the clinical symptoms are blurred, and signs of peritoneal irritation can only be detected after some time.
The transition to the toxic phase is characterized by an increase in intoxication, since during this period the concentration of microbes in the body increases significantly, and toxins are practically not eliminated. Against this background, signs of central nervous system damage and metabolic disorders clearly appear.
The terminal stage is the final and most severe during pelvioperitonitis, occurs acutely or subacutely, and may be accompanied by the formation of abscesses in the abdominal cavity. The patient experiences motor and nervous retardation, decreased blood pressure, flatulence and bloating, and decreased urine output.
Dystrophic changes and dehydration occur in tissues and organs. At this stage, bronchopneumonia, pulmonary edema, purulent inflammation of the pericardium and anterior mediastinum may occur.
The patient's general condition is characterized as serious; she complains of severe thirst and dry mouth, shortness of breath, fever, nausea and vomiting. Breathing becomes chesty, the stomach is swollen and does not participate in the breathing process. Initially, vomit consists of the contents of the stomach, and over time, bile and contents of the small intestine are added to it.
The clinical picture of peritonitis after cesarean section may have an atypical appearance. So, the patient has a high temperature, a frequent superficial pulse and shortness of breath, against this background moderate flatulence appears, and there are no signs of intestinal paresis. The course is undulating, periods of deterioration of health are replaced by temporary relief.
If the development of peritonitis is associated with salpingo-oophoritis, the patient suddenly experiences cutting pain of great intensity and collapse develops. Initially, the pain does not have a clear localization, and after a while it subsides in the area of purulent inflammation. In the same place there is rigidity of the muscles of the anterior abdominal wall.
Conducting a vaginal examination, the attending physician notes severe soreness of the uterus, its displacement and blurred contours. When palpating the posterior vaginal fornix, the victim feels pain. The posterior arch may be slightly protruded.
Peritonitis occurring during antibiotic therapy may not have pronounced symptoms. The pathology clinic is slowly increasing, while the general condition of the patient can be considered satisfactory. After about 3-5 days, the manifestations of the disease become typically acute.
Preoperative preparation and monitoring
- For successful surgical intervention, it is necessary to carry out preoperative preparation.
- The patient must have a peripheral and central vein and bladder catheterized and premedicated.
- Midazolam (5 mg) and 10–20 mg of cerucal are administered on the operating table. Atropine administration is contraindicated, as there is a high probability of developing bradycardia.
- Medicines are administered that help reduce the acidity of gastric juice (about 40 mg of omeprazole or famotidine/ranitidine 50 mg into a vein).
- During the operation, infusion therapy is carried out in an amount of at least 1.5 liters of physiological solution, and plasma and blood products are added if necessary.
- Perform artificial ventilation and administer oxygen.
In the case when the patient lies on the operating table and there is more than 25 ml of contents in the stomach, there is a real threat of aspiration. This is the name for the entry of stomach contents into the lumen of the bronchial tree. Gastric juice can cause a burn to the mucous membrane of the bronchi and trachea. Complications of aspiration include multiple pulmonary atelectasis, bronchospasm, respiratory failure, and pulmonary edema.
Aspiration of small amounts of gastric juice can subsequently lead to aspiration pneumonia.
Therefore, in anesthesiological practice in patients with peritonitis, ganglioblockers and anticholinergics - drugs that can reduce the tone of the lower esophageal sphincter - are not used.
Antibacterial therapy is carried out with a combination of antibiotics that act on both Gram-plus and Gram-minus bacteria. For community-acquired peritonitis, this is intravenous administration of cefotaxime and metronidazole. For in-hospital use - cefepime and metronidazole. If peritonitis develops in the hospital during antibiotic therapy, carbapenems are used.
Manifestations in children
The development of peritonitis in children is also characterized by some atypical symptoms. For example, acute pain syndrome in a child is the exception rather than the rule. The child’s body is in the formative stage, so peritonitis usually begins with a general deterioration in health, and, in general, the symptoms are not as pronounced as in adults. If the pathology begins after injury, appendicitis or an infectious lesion, children experience:
- general weakness and lethargy;
- loss of appetite;
- tearfulness and moodiness;
- sleep disorders, insomnia;
- temperature increase;
- stool disorder (more often constipation than diarrhea);
- bloating;
- lower abdominal pain;
- dry skin, thirst.
As for the primary form of peritonitis, the rapidly passing reactive phase proceeds similarly, after which the toxic stage begins with the following symptoms:
- very high temperature (up to 40 degrees);
- pain in the lower abdomen;
- nausea and frequent vomiting;
- loose stools;
- body aches, muscle pain;
- paleness of the skin;
- the tongue is dry, covered with a white coating.
With diffuse peritonitis, the child experiences severe discomfort on the right side of the iliac region, an increase in temperature to 37.5-38 degrees, weakness, body aches, and joint pain.
Appendiceal peritonitis is accompanied by an infectious-inflammatory syndrome, as well as signs of abdominal damage:
- diffuse abdominal pain without clear localization;
- muscle tension in the anterior abdominal wall;
- feeling of fluid accumulation in the peritoneum;
- sleep disturbance;
- increased body temperature;
- frequent persistent vomiting;
- weight loss;
- yellowness of the skin and sclera;
- hypoxia;
- general depression, lethargy and weakness.
Postoperative period
Antibiotic therapy for peritonitis is mandatory
In the postoperative period, some problems may arise related to the normal functioning of the intestines, severe pain, and the development of purulent complications. Recommended:
- observation of the patient, hourly assessment of respiratory rate, pulse, diuresis, central venous pressure, drainage discharge;
- infusion therapy with colloid and crystalloid solutions is carried out;
- to warm patients, infusion media are heated to body temperature;
- the lungs are ventilated for 72 hours to ensure sufficient oxygen supply to organs and tissues;
- a glucose solution is administered through a nasogastric tube;
- early restoration of intestinal motility;
- prevention of pain syndrome. Narcotic analgesics are used in combination with non-steroidal anti-inflammatory drugs. Fentanyl, morphine, ketorolac are used.
Ultrasound signs
The ultrasound method for diagnosing peritonitis is the most accessible non-invasive research method, especially in the early postoperative period, as well as in acute peritonitis before surgery. It should be noted that it is impossible to determine the direct cause of peritonitis based on ultrasound results - the diagnostic method only shows the presence of pathology. For example, with bacterial peritonitis, using ultrasound it is not possible to differentiate changes caused by a specific pathogen, but it is possible to detect perforation or rupture of the appendix, leakage of an infected substrate into the abdominal cavity, as well as hematogenous dissemination in the tuberculosis form.
Aseptic peritonitis on ultrasound is manifested by echogenic thickening of the peritoneum, as well as a small amount of limited fluid in the abdominal cavity. Ultrasound diagnostics also show local or diffuse intestinal paresis with a local increase in intestinal fluid contents.
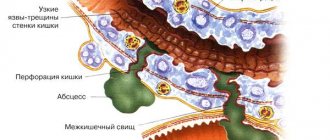
An abdominal abscess, which develops as a complication of peritonitis, is visible on ultrasound as a localized fluid formation. It has a noticeable clear wall, forming a capsule with heterogeneous contents in the form of an echogenic suspension or thread-like structures. The presence of gas is reflected as a reverberation effect.
Perforation of a hollow organ is a perforation of its wall, in which the contents of the organ extend beyond its boundaries, that is, into the abdominal cavity. In this case, the presence of free air in the cavity is determined, sometimes under the anterior abdominal wall. On ultrasound, the sign is displayed by reverberation. In addition, perforation can be determined by the presence of free fluid in the abdomen.
In addition to peritonitis, free fluid in the abdominal cavity may indicate the presence of ascites or acute abdominal pathology in which the peritoneum is involved. Often this sign indicates the presence of a closed injury to the abdominal organs. Typical sites for free fluid detection are the perihepatic or perisplenic space, the pelvic area, and the left and right lateral canals. Fluid on ultrasound is visible as local zones of reduced echogenicity without clear contours. When changing body position, they change shape. The amount of such fluid is important for diagnosis, although it is difficult to measure it using ultrasound results.
Postoperative complications of peritonitis, including tertiary peritonitis, can be detected by the presence of intra-abdominal abscesses or accumulations of exudate.
In addition, typical ultrasound signs of peritonitis are the following:
- dilation of intestinal loops;
- loops full of liquid;
- the presence of free fluid in the abdominal cavity;
- interloop or subphrenic abscesses;
- thickening of the intestinal walls.
What does acute peritonitis look like?
The classic picture of acute peritonitis is accompanied by severe abdominal pain, which constantly intensifies, nausea and persistent vomiting, and progressive fever. In addition, upon palpation the patient feels significant pain and tension in the anterior abdominal wall. After some time, during an acute course, the so-called syndrome of imaginary well-being occurs (temporary lull), when partial paralysis of pain receptors develops, due to which the pain subsides somewhat, but after 2-3 hours the pain syndrome progresses.
Classification
Peritonitis is of the following types:
- bacterial – caused by microbial flora;
- abacterial - with aseptic or toxic-chemical inflammation of the peritoneum due to its irritation by aggressive non-infected fluids (blood, digestive enzymes and secretions of internal organs, urine);
- special forms - parasitic, rheumatoid, carcinomatous and granulomatous.
According to the course of the disease, peritonitis is divided into acute and chronic.
According to the area of the affected peritoneum, inflammation can be limited, local (with damage to 1-2 anatomical areas), diffuse (covering three or more areas) and general (with total inflammation).
In its development, the disease goes through an early phase (less than twelve hours), late (less than five days) and final (from one to three weeks from the onset of inflammation).