NB Bougienage is a method of diagnosis and treatment used for diseases of hollow organs, performed with special instruments (bougies) that make it possible to expand the lumen of the organ.
NB Bougie is an instrument for examining and expanding the lumen of a hollow organ. Bougies have been known since ancient times. Bronze bougies for dilating the urinary tract, similar to modern ones, were found during excavations in Pompeii, a city destroyed in 79 AD, almost two thousand years ago!
What is bougienage of the esophagus?
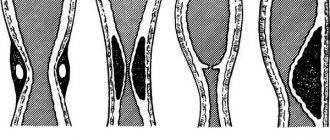
Bougienage is performed both in surgical hospitals, under fluoroscopy control, and in endoscopic departments. The use of sequential bougies of ever-increasing diameter makes it possible to significantly expand the esophagus and restore normal nutrition through the mouth. Bougies of various diameters
The radiograph shows a bougie inserted into the lumen of the esophagus.
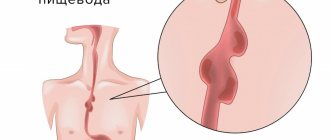
Is bougienage of the esophagus highly effective in patients with SCAR STRICTURES OF THE ESOPHAGUS?
Bougienage of the esophagus is a highly effective method of treating patients with SCAR STRICTURES OF THE ESOPHAGUS. Good results in these patients can be achieved; according to various researchers, they can be achieved in 75–85% of cases. Another thing is that such results can not be obtained in all groups of patients with SCAR STRICTURES OF THE ESOPHAGUS. In particular, with long strictures this method is much less effective than with short narrowings. In addition, a lasting effect in many cases is achieved only after several courses of bougienage. However, bougienage is the method of choice to avoid surgery in a significant proportion of patients with esophageal strictures.
Is surgical treatment indicated for patients with SCAR STRICTURES OF THE ESOPHAGUS?
As in many other situations, indications for surgery in patients with SCAR STRICTURES OF THE ESOPHAGUS arise when less traumatic and accessible types of treatment are ineffective. In particular, these are the impossibility of bougienage, or the ineffectiveness of bougienage with a rapid return of manifestations of the disease (recurrence of stricture).
What is the surgical treatment of patients with SCAR STRICTURES OF THE ESOPHAGUS?
In patients with peptic stricture of the esophagus (link to the section - “What is PEPTICA Stricture of the esophagus ...”), an organ-preserving operation is possible, when after bougienage a so-called fundoplication is performed, that is, a special cuff that prevents the reflux of gastric contents into the esophagus. In this case, conditions are created for the inflammation in the esophagus to subside and to prevent further development of the stricture. The first anti-reflux operation, fundoplication, was performed by Rudolph Nissen (1896–1981) in 1955.
NB Fundoplication is an antireflux operation that involves wrapping the fundus of the stomach around the esophagus, creating a cuff that prevents gastric contents from refluxing into the esophagus.
NB Reflux - (Latin refluo - flow backward) - reverse flow of the contents of hollow organs compared to its normal movement. Antireflux – preventing reflux.
However, the main method of treating patients with SCAR STRICTURES OF THE ESOPHAGUS is the so-called esophagoplasty, that is, an intervention in which a new esophagus is created. The material for creating the esophagus is usually the patient’s own stomach or intestines, from which a tube of the required diameter is formed. The patient’s own esophagus, depending on the indications, can be removed or preserved, with the formation of a new esophagus bypassing the old one (the so-called esophageal bypass surgery). Today, these interventions are becoming less traumatic and are performed using endoscopic techniques (link – section “For Specialists” - “Video Materials”).
Promising methods for treating patients with SCAR STRICTURES OF THE ESOPHAGUS?
This method should be considered stenting the esophagus, that is, placing a special tubular prosthesis into the lumen of the esophagus, which will not allow scars to narrow the esophagus. To date, these stents are only being developed and tested, but this direction is certainly promising. The use of endoscopic technology when performing operations on both the chest and abdominal cavity is undoubtedly relevant. Finally, an important and promising area of work for the department is performing repeated operations on the esophagus after unsuccessful attempts at intervention, as well as using previously injured or damaged organs (the so-called pathologically altered ones). For example, as mentioned earlier, a burn can damage not only the patient’s esophagus, but also his stomach. However, the department has developed technologies for using such a stomach to perform surgery, which can be demonstrated by describing a clinical observation.
Clinical cases
To view clinical cases of patients with esophageal stricture, click on the link below. Please note that this information is intended for specialists and contains naturalistic photos and video materials.
- Thoracoscopic subtotal resection of the esophagus with simultaneous laparoscopically assisted gastric tube plasty
- Extirpation of the esophagus with simultaneous plastic surgery of a pathologically altered stomach
Read information about the features of thoracoscopic operations .
Surgical treatment of esophageal strictures can be performed as part of the provision of VMP. Read more about free high-tech medical care .
How to get treatment at the Department of Stomach and Esophageal Surgery of the Russian Scientific Center for Surgery.
To schedule a consultation, call:
+7 (499) 248 13 91 +7 (903) 728 24 52 +7 (499) 248 15 55
Submit a request for a consultation by filling out the form on our website and attaching the necessary documents.
Esophageal endoprosthetics with self-expanding stents
One of the problems with inoperable esophageal cancer, tumor recurrence in the anastomotic area, compression of the esophageal lumen, is the elimination of dysphagia and restoration of enteral nutrition and passage through the esophagus. For this purpose, as a rule, gastro- or enterostomy is performed in this category of patients. However, the presence of various stomas not only increases psychological trauma in patients, but is associated with a certain risk and the development of complications in weakened patients, regardless of the method (surgical, laparoscopic, endoscopic) of its application. Endoscopic methods of recanalization of the lumen of the esophagus - electro-, laser, argon plasma coagulation, bougienage or balloon dilation - allow to restore the lumen in most cases, but the effect is most often short-lived and repeated interventions are usually required. In this regard, in inoperable patients with stenotic tumors of the esophagus, endoscopic stenting is increasingly being used as one of the safest, minimally invasive and effective methods of treatment. Abroad, endoprosthesis replacement with self-expanding metal stents, which quickly replaced plastic tubular endoprostheses, has been used for quite a long time, especially for esophageal cancer, and to date, researchers have already accumulated a lot of experience. In Russia, I. Kh. Rabkin et al. (1989) performed X-ray endoesophageal prosthetics with a nitinol prosthesis for esophageal cancer in 3 patients back in February 1988, however, this technique began to be used more widely only in recent years.
The main goal of esophageal stenting is to improve the quality of life of inoperable patients.
Before placing a stent, a thorough examination of the patient is carried out. To establish a diagnosis and clarify the extent of the tumor, fluoroscopy with a barium suspension or water-soluble contrast agent and endoscopic examination with a biopsy are performed. Ultrasound, CT and MRI are used to stage the tumor and assess the patient's operability. Self-expanding stents such as South Korea, FerX-ELLA Boubella, Czech Republic, etc. are used for endoprosthetics.
Stenting is performed under X-ray control, with the patient in the left lateral position, under intravenous sedation using endoscopes. If it is possible to pass the endoscope through the narrowing, only endoscopic control can be carried out. During esophagogastroduodenoscopy, the diameter of the lumen and the extent of stenosis were determined to select an endoprosthesis. The upper and lower edges of the stent should be at least 2 cm above and below the boundaries of the stenotic area, in addition, it is necessary to take into account the fact that the stent will slightly shorten when it is expanded. Therefore, the length of the endoprosthesis should be 5-6 cm greater than the length of the lesion.
If necessary, marking the boundaries of the stenosis is carried out in several ways. Under X-ray control, focusing on the image of the distal end of the endoscope, radiopaque marks were placed on the skin at the level of the upper and lower edges of the narrowing, which were fixed with an adhesive tape. The tumor boundaries can be marked with clips using an endoscopic clipper or by injecting 1 ml of water-soluble contrast agent into the submucosal layer. It is most convenient and reliable to mark the boundaries of the lesion, if necessary, by clipping or the injection method, since the marks on the skin easily move even with a slight change in the position of the patient’s body, and when the lesion is localized in the intestine, it is generally very difficult to navigate along them. After marking the boundaries, a guide wire was installed under visual control below the affected area. For this purpose, in a number of cases small-caliber endoscopes were used. In case of lesions of the esophagus, cardia, or esophageal anastomosis, the endoscope was removed, leaving the guidewire. Further manipulations are performed under X-ray or endoscopic control. The stent is supplied by the manufacturer complete with a special device for its insertion. This device with a compressed metal mesh stent inside is inserted into the affected area along a guide string, focusing on previously installed marks. After this, the sheath is gradually, very slowly tightened, holding the stent in the assembled state, controlling radiographically or visually the position of the stent and the degree of its opening. In addition to markers marking the boundaries of the tumor, the stent itself also contains radiopaque markers, which greatly facilitates control of the position of the endoprosthesis. The hand holding the delivery device must be pressed tightly against the body, that is, its position must be fixed, otherwise the stent may be displaced when the outer sheath is pulled together. It is possible to correct the position of the stent together with the delivery device by tightening, but it is impossible to move an already partially deployed stent forward due to the risk of damage. If there is a need to move the stent forward, you should first remove the stent back into the outer case. This can be done if the stent has been deployed less than halfway (before passing the control mark on the delivery device). In the unaffected part of the digestive tube, the stent opened completely, in the area of stenosis - partially, approximately 60-80%. After the stent was fully deployed, the outer sheath, the delivery device with the olive at the distal end, and the string were removed. Then the position of the endoprosthesis is endoscopically controlled.
2-3 hours after the intervention, patients are allowed to drink cold drinks. Full deployment of the prosthesis occurs after 24-72 hours, which is determined by plain fluoroscopy; evacuation is assessed by radiography with a water-soluble contrast agent or liquid barium suspension.
If the prosthesis was in adequate position, the patient was allowed to eat semi-liquid and mushy food. Subsequently, patients were recommended to eat split meals of mushy food, ending each meal with a few sips of warm water to rinse the stent.
In the immediate period after prosthetics, almost all patients experience chest pain, but constant pain persists in less than 10 - 15% of patients. The most intense pain occurs when stenting high strictures and when using large-diameter stents. Almost all patients report discomfort and a feeling of pressure behind the sternum after installation of the prosthesis, and therefore, in the first 3 days they are prescribed non-narcotic analgesics. Early complications such as bleeding, perforation, aspiration, fever and fistulas develop in 10-20% of patients. Deaths associated with the stent placement procedure are rare and are more often associated with profuse bleeding or aspiration.
The migration rate of bare stents is 0-3% and increases to 6% when stenting the cardia area. The migration rate of covered stents ranges from 10% to 30% and increases with stenting of the esophagogastric junction. Rare cases of tracheal compression have been reported after stenting of strictures of the upper third of the esophagus. If migration has occurred, the position of the stent can be corrected during esophagoscopy: using biopsy forceps, the prosthesis is pulled into an adequate position using a lasso.
Repeated interventions (endoscopic recanalization during restenting) are not uncommon (8-35%) and are primarily performed when tumors invade bare stents. Retrospective studies have shown that recurrent dysphagia due to tumor invasion of uncovered stents occurs in 60% of cases. With covered prostheses, repeated dysphagia develops due to tumor growth of the proximal or distal edges of the stent, and in half of the cases due to the growth of non-tumor tissue (mucosal hyperplasia, granulation, fibrosis). Complications such as erosive bleeding occur in 3-10% of cases, ulcerative esophagitis - in 7%, perforation or fistulas - in 5%, fracture or destruction of the stent structure - in 2%. MQ Wang et al. found that life-threatening complications (massive bleeding, perforation, fistulas, tracheal compression) most often develop with stenting of the proximal third of the esophagus. Nd:YAG laser ablation, PDT, argon plasma coagulation, ethanol injection, or repeat stenting can be used to treat recurrent esophageal stenosis.
Endoprosthesis replacement with self-expanding stents provides a fairly wide lumen of the esophagus, adequate nutrition, as a rule, does not require repeated therapeutic interventions, and is accompanied by moderate pain, which improves the quality of life of this category of patients.