How can you become infected with rotavirus?
The virus is transmitted from person to person directly or through objects. It is excreted in feces and spread through poorly washed hands. The patient is contagious for a week after the first symptoms appear.
To infect a child, the virus must get from the hands into the mouth. Children constantly taste the world around them, which means they are very susceptible to rotavirus infection. The virus can be transmitted to a baby from an adult who touches the baby's nipples and toys with poorly washed hands. Often infants get sick in families where older children are sick.
Outbreaks of rotavirus infection occur in winter and spring, which is facilitated by weakened immunity due to cold weather.
Symptoms of rotavirus
The first symptoms appear at the earliest 12 hours after infection. But it can take up to 5 days before the disease manifests itself.
The disease begins very rapidly - vomiting, acute watery diarrhea, in the first days there is a high temperature:
- temperature up to 39 degrees can persist for up to 4 days;
- repeated vomiting – up to 2 days;
- frequent diarrhea up to 14 days;
The stool is copious, usually watery, foamy, yellow or greenish in color and fairly uniform. In children under two years of age, the frequency of stool reaches 20 times a day.
In the first days of the disease, other symptoms are observed:
- Sharp, gripping pain in the upper abdomen that can spread throughout the abdomen
- Weakness, lack of appetite, dizziness and lethargy are signs of intoxication
- Sometimes mild nasal congestion, runny nose and dry cough occur
- Feeling bloated and gurgling in the abdomen
Rotavirus infection is more dangerous the younger the child. With vomiting and stool, moisture quickly disappears, and dehydration develops. Infants under one year old count by tens of minutes, not even by hours. It is important to notice signs of dehydration:
- Moderate dehydration: thirst, dry mucous membranes, pale skin, infrequent urination, deep-colored urine, crying without tears, sunken fontanel in infants
- Severe dehydration: dry skin, hoarseness of voice, sharpening of facial features, and convulsions.
The severity of the disease depends on the number of viruses that have entered the child’s body.
Call a doctor immediately if the following symptoms appear:
- Red blood in the stool or black and shiny stool may be the result of bleeding in the intestines.
- Severe abdominal pain also indicates intestinal damage
- Stool more than 10 times a day and vomiting more than 7 times are very dangerous due to dehydration.
- Rash on the body - may be a symptom of typhus
Rotavirus gastroenteritis in children
The incubation period lasts from 1 to 5 days when a child is infected with rotavirus gastroenteritis. The disease begins acutely or violently. Manifested by the following symptoms:
- stomach ache
- vomit
- rise in body temperature to 37.5-38 °C (rarely - up to 38 °C)
- bowel disorder.
The vomit is initially abundant, containing food impurities, then becomes watery in nature, and contains mucus impurities in the form of floating flakes.
The child constantly feels sick and his appetite is greatly reduced. Stool occurs from 5 to 15 times a day. It is rich and watery. The color of the stool is yellow or yellow-green. Foamy consistency, pungent odor. In some cases, the stool is cloudy-whitish or scaly, which is similar to the stool of children with cholera.
Older children complain of abdominal pain, which is mainly concentrated in the epigastric region or around the umbilical area. The pain can be either constant or severe cramping, which is similar to attacks of intestinal colic.
The urge to defecate occurs suddenly, almost always accompanied by rumbling in the stomach. Then there is a loud passage of gases and splashing stools. After bowel movement, relief occurs. The mucous membranes of the soft palate, uvula, palatine arches are partially hyperemic and slightly edematous. Enlargement of the liver and spleen is not observed. In severe cases, there may be symptoms such as headache, severe weakness, mild chills, dizziness, loss of consciousness, and convulsions.
Due to the rapid loss of water by the body, children under 12 months may develop isotonic or hypertonic dehydration. In such cases, body weight falls, bloating is observed, etc.
In the peripheral blood in the first days of the disease there may be moderate leukocytosis with neutrophilia; at the peak of symptoms, leukopenia with lymphocytosis is most often found, ESR is within normal limits.
Flow. The disease occurs cyclically. In the first 2-3 days after the onset of rotavirus gastroenteritis, children experience an increase in temperature and intoxication. Diarrhea lasts from 3 to 6 days. In general, the disease lasts from 1 week to 10 days, in severe cases – longer.
The prognosis is favorable in almost all cases. Isolated cases of illness in infants under 12 months of age result in death, when severe dehydration and cardiovascular and renal failure develop.
Complications can arise due to the addition of a bacterial or viral-bacterial infection and almost always occur in young children.
Diagnosis of rotavirus infection
Rotavirus infection is diagnosed by the presence of typical signs of the disease: fever, vomiting and diarrhea.
It is important to know that you can get sick from rotavirus infection in an atypical form. In this case, the disease progresses more easily. Only 1-2 signs may be expressed or not expressed at all. In this case, the person releases the virus and is infectious.
There are various stool tests that can detect the virus. However, treatment must begin immediately when the first symptoms appear, without waiting for test results.
Treatment
There is no cure for rotavirus. Treatment tactics consist of maintaining impaired body functions. The first task is to replenish the loss of fluid and salts.
Dehydration is the most dangerous symptom. It is important to determine its severity in order to choose the right treatment tactics. A doctor will help with this. For mild to moderate cases, oral rehydration is used - drinking with a special solution, which is not difficult to prepare yourself. In case of severe dehydration, IV drips are prescribed.
What can parents do before the doctor arrives?
- If the temperature is high, give a child's antipyretic.
- Continue to feed your baby every 3-4 hours. This is important for restoring micronutrients and preventing weight loss. Add salt to food during diarrhea.
- Provide plenty of fluids. But do not let your child drink a large amount at once, as this may cause vomiting. Offer a few spoons every 10-15 minutes.
What to drink?
A solution for oral rehydration (replenishment of fluid loss) can be bought at a pharmacy or prepared independently by dissolving 3 grams of table salt (a full teaspoon) and 18 grams of sugar in one liter of water. This recipe is recommended by WHO (World Health Organization).
The product that you buy at the pharmacy has a slightly more complex composition, but its purpose remains to replenish the loss of water and salts.
Warm the solution to body temperature so that it is absorbed faster.
How much fluid to give?
WHO recommends giving as much as the child wants to drink. In the first 3-4 hours, let's drink little and often. Watch for symptoms of dehydration, they should go away. After replenishing fluid loss after each episode of diarrhea, give the following amount:
- children under 2 years old: 50-100 ml of liquid;
- children from 2 to 10 years: 100-200 ml;
- For older children and adults: as much liquid as they want.
What cannot be used to treat rotavirus infection?
Do not give sugar-sweetened drinks: juices, soda, sweet tea. All of them worsen diarrhea.
What medications to take for rotavirus
WHO recommends introducing 10-20 mg zinc supplements into a child's diet for 10-14 days. This will reduce the severity of diarrhea and the risk of dehydration.
Other medications depend on the type of infection and can only be prescribed by a doctor.
Is it possible to be treated at home?
Treatment is prescribed by your doctor based on the degree of dehydration and the presence of other infections. Offer your child something to drink until the doctor arrives. The parent's job is to prevent severe dehydration.
Rotavirus - treatment and prevention
Moiseeva Tatyana Sergeevna
Pediatrician, Infectious disease specialist
April 25, 2021
intestinal infections sooner or later. After acute respiratory viral infections (ARVI and influenza), this is the most common reason for visiting a doctor in childhood. They are a problem not only for the child, but also for the whole family. Perhaps the most common intestinal infection at the moment is rotavirus or, as parents often call it, “intestinal flu”.
Regardless of the social status of the family and the sanitary and hygienic situation in the house, from birth to 5 years, almost all children suffer from rotavirus gastroenteritis . According to statistics, more than 137 million people worldwide suffer from this infection every year, approximately a quarter of whom are hospitalized. Unfortunately, there are cases with fatal outcomes, including in children. Rotavirus gastroenteritis is most severe in children when they first encounter the virus, which usually happens between the ages of 6 and 18 months. In babies who are bottle-fed, the risk of infection and a more severe course is slightly higher.
Adults are also susceptible to this infection. You can become infected repeatedly during your life, since natural immunity to the virus is type-specific (it protects only against a specific type of rotavirus and does not protect against others). With repeated contact with the virus, the disease is usually less severe, but the person is contagious and can spread the infection.
So, what is rotavirus? There is an opinion that rotavirus got its name because it enters the human body through the mouth, this is not true, the virus is called that because its external structure resembles a wheel (from the Latin - rota), hence the name. There are several types, slightly different from each other in structure, but causing the same clinical picture of the disease.
The route of transmission of this infection is fecal-oral, that is, to put it simply, it is a “disease of dirty hands.” The virus is very contagious; just 10 particles of the virus are enough to make you sick. Rotavirus persists for a long time on any surface, even with thorough cleaning. Therefore, very often several family members, including adults, are sick with this infection at the same time, and outbreaks occur in children's groups. It is worth noting that you can only become infected from a sick person; pets do not get sick from “human” rotaviruses.
The incubation period for rotavirus infection ranges from several hours to 5-7 days. It is characterized by general malaise, weakness, refusal to eat, increased body temperature and symptoms of damage to the gastrointestinal tract (frequent watery loose stools, vomiting, abdominal pain). At the first signs of illness, you must seek medical help! After examining the child, the doctor will assess his condition, the need for hospitalization, and prescribe examination and treatment.
To diagnose the infection, stool testing for rotavirus is used using the PCR (polymerase chain reaction) and ELISA (enzyme-linked immunosorbent assay) method; the result is usually ready in 1-2 days. But treatment must begin at the first symptoms of the disease, without waiting for results. Therapy is carried out according to symptoms, and practically does not depend on test results. Tests are prescribed to make sure that it is a rotavirus infection and in case of complications, so that doctors understand what exactly they are dealing with.
To treat children who do not need hospitalization and remain at home under the supervision of a pediatrician, so-called pathogenetic therapy is used, aimed at replacing the fluid that the child loses during illness with loose stools and vomit.
The most important rule for a mother with rotavirus is to give her child a few sips every 5-10 minutes. If the child refuses, then feed him from a spoon or from a syringe (after removing the needle). You should not let your child drink large amounts of liquid at one time, even if they are very thirsty, as this may cause vomiting. You need to be patient and constantly, despite the protests, give him water, water, water. It is desoldering that helps avoid dehydration and hospitalization.
In addition to water, special saline solutions from the pharmacy are used to water the child, containing salts that are lost by the body during illness (Hidrovit, Humana, Electrolyte, Gastrolit, Regidron, etc.). In the absence of special drugs, you can use a homemade solution until you purchase them. You can prepare it by taking a liter of boiled water, adding 1-2 tablespoons of sugar (without a slide), half a teaspoon of table salt and one-third of a teaspoon of baking soda. The prepared solution can be stored for no more than a day. Children should not be fed with milk, juices, fruit drinks, vegetable broths, or carbonated drinks.
The second important component of the treatment of rotavirus infection is diet therapy . During the acute illness and 2-3 weeks after it, the child is prescribed a gentle diet, with the exception of dairy products, juices, raw fruits and vegetables. The child should eat more often than usual, in small portions. Food should be as gentle as possible on the stomach - not spicy, not fatty, not hot, not fried.
For young children who are breastfed or bottle-fed, the issue of further feeding is decided individually with a pediatrician. If frequent loose stools persist in bottle-fed children, the option of temporarily switching to a formula with a reduced lactose content (lactose-free, low-lactose, etc.) is possible. For infants, the issue of partially replacing breast milk with a formula with a reduced lactose content or adding special enzymes to breast milk that help the milk to be absorbed in the baby’s intestines (lactase enzyme preparations) is being resolved.
Also used in therapy are such groups of drugs as: enterosorbents (Smecta, Filtrum-sti, Enterosgel, etc.), probiotics (Enterol, Linex, Bifiform, Acipol, etc.), prebiotics (Hilak-forte, Duphalac, etc.), enzymes (Creon 10000, Mezim-forte, Pancreatin). You should not give these drugs to your child on your own; you should consult a doctor, as you need to understand the advisability of taking them at different periods of the disease.
, antiviral and immunomodulatory therapy can be carried out . The decision to prescribe drugs in this group is made only by the doctor.
Antibacterial therapy is worth considering separately. Antibacterial therapy is not carried out for uncomplicated rotavirus infection. But in some cases, doctors still prescribe antibiotics. And it's not just a matter of habit. This is due to the fact that acute intestinal infections are not only of a viral nature, but also of a bacterial nature (Escherichia coli, Salmonella, Yersinia and some others). And it is not always possible to determine with 100% accuracy from the symptoms what caused the symptoms: a viral infection, a toxic infection or a bacterial one. There are also mixed causes and atypical course of the disease, so the issue of prescribing antibacterial drugs remains at the discretion of the attending physician.
Very important! If watering the child turned out to be ineffective and the child continues to vomit, weakness increases, he urinates less than usual (the interval is 3-4 hours), then there are direct indications for hospitalization of the baby in a hospital, where he will be prescribed infusion therapy (intravenous fluid).
Currently, there is a unique opportunity to protect your baby from rotavirus infection . The Rotatek® vaccine has been certified in Russia and has been successfully used abroad for several years. The vaccine protects against the five most common types of rotavirus and prevents severe forms of other types of the virus. For a full course of vaccination, 3 vaccines must be administered. The convenience of using the vaccine lies in the fact that it is presented in the form of drops for oral administration, and not in the form of a syringe for intramuscular injection. The first dose of the vaccine is at 6-12 weeks of age, then 2 more at an interval of at least 4 weeks. Revaccinations, that is, repeated injections of the vaccine after a full course of vaccination from 3 stages, are not required.
The vaccine is intended for children from 6 weeks to 32 weeks , and is not used in adults. This is due to the fact that the first encounter with the virus and the most severe course of the disease occurs during this period. In the future, after the immune system has become “acquainted” with the virus, the likelihood of developing a serious illness decreases and immunoprophylaxis with a vaccine is no longer so relevant.
Rotavirus in a newborn
Infants become dehydrated very quickly, so the general course of rotavirus infection is usually quite severe. The recommendations also include drinking plenty of fluids. Breastfed babies get most of their fluid from breast milk. Therefore, it is important to put your baby to the breast frequently. Mom can notice that the child himself began to ask for the breast more often during illness - this is not hunger, but the need to replenish water losses.
It is also important to put mixed-fed babies to the breast more often, and to switch formula-fed babies to a low-lactose or lactose-free formula for the period of illness and recovery. You can order this mixture with fast delivery throughout Moscow and all of Russia in our online store.
Rotavirus infection - symptoms and treatment
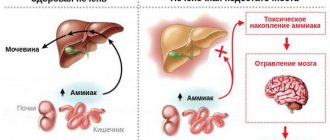
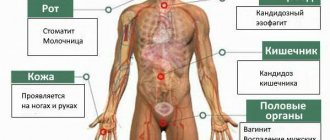
Complications of the disease include dehydration syndrome, secondary bacteremia and candidemia (penetration of Candida bacteria and fungi into the blood), convulsions, aseptic meningitis, encephalitis, myocarditis, bronchopneumonia, hepatitis and acute renal failure.
One of the most common complications is dehydration syndrome , which develops with the loss of water and electrolytes. Determining its severity is extremely important to determine fluid replacement tactics for a particular patient.
When assessing the patient's condition, it is necessary to take into account the degree of dehydration - the type of fluid lost (extracellular and/or intracellular) and its volume. In children with rotavirus gastroenteritis, fluid loss usually occurs primarily from the extracellular space.
The amount of extracellular fluid lost is objectively measured by the change in weight from baseline. Since the weight before the disease is often not reliably known, a number of clinical signs (thirst, decreased urination, lethargy, irritability), as well as capillary refill time and objective examination data (pulse and respiratory rate, blood pressure, skin turgor) are used to assess the degree of dehydration. speed of skin fold straightening). Based on the totality of these data, dehydration is divided into degrees of severity:
- mild (loss of 3-5% fluid) - clinical signs may be absent or minimal;
- moderate (loss of 6-9% fluid) - tachycardia, gradual drop in blood pressure, decreased skin turgor, dry mucous membranes, irritability, prolongation of capillary refill time to 3 seconds, rapid shallow breathing, decreased urine volume, lack of tears, in infants - sunken fontanel;
- severe (loss of ≥ 10% fluid) - clinical picture of shock.
It should be noted that clinical signs of dehydration are reliable indicators in a comprehensive assessment: individually, each of them lacks sensitivity and specificity.
a clinical dehydration score in 2008 . It takes into account 4 parameters: general appearance, condition of the eyeballs, mucous membranes and the presence of lacrimation. According to this scale:
- A score of 0 indicates no dehydration;
- 1-4 points correspond to a mild degree of dehydration;
- 5-8 points - moderate and severe severity.
Another fairly common complication is seizures . They manifest themselves in the form of short focal seizures within 1-2 days and have a favorable prognosis.
All neurological complications of rotavirus gastroenteritis (convulsions, transient loss of consciousness, encephalopathy) are manifestations of extracellular dehydration and are caused by the development of hyponatremia - a decrease in sodium levels in the blood. The severity of symptoms is determined by the degree of hyponatremia and the rate of its increase. In addition, rotavirus RNA has been found in the cerebrospinal fluid (CSF) of patients with rotavirus diarrhea and seizures and/or encephalitis, but the diagnostic significance of this finding remains unclear.
If fever persists or resumes after the third day of rotavirus infection, it is necessary to exclude bacteremia and the development of secondary bacterial complications. The exact mechanism of their occurrence is unknown, but it is believed that infected enterocytes become more vulnerable to bacterial invasion during the course of the disease.
In addition to complications caused by gastroenteritis, rotavirus infection can serve as a trigger for the onset of type 1 diabetes mellitus in genetically predisposed individuals [4][5][7][8][10][11].