Liver failure is a complex of complex symptoms that is characterized by a violation of the vital functions of the liver, caused by acute or chronic damage to the organ tissue.
Any abnormal liver function requires immediate medical intervention. There are acute and chronic liver failure. Chronic liver failure develops over several months or years, but acute liver failure can develop within a few hours.
What functions does the liver perform?
The content of the article
The liver is a large organ located in the abdominal cavity. This important organ performs various functions and takes a significant part in regulating the homeostasis of the body.
The most important functions of the liver:
- metabolic function - processing of carbohydrates, proteins, fats;
- storage - including iron and vitamins;
- detoxification - the liver is involved in the removal of harmful substances in food, as well as medications;
- production of bile, which is especially important when digesting fats;
- Immune function - Some liver cells play an important role in immune responses.
Prevention
Prevention of acute liver failure involves the prevention of infectious diseases and toxic damage to the organ. For this purpose, it is important to maintain personal hygiene and sexual hygiene, which excludes infection with viral hepatitis, adherence to safety measures when working with toxic substances, strict adherence to drug doses and refusal to take chemicals unless absolutely necessary. Prevention of chronic liver failure involves treatment of liver diseases, preventive courses of hepatorotectors, constant adherence to a diet, and sanatorium-resort treatment. alcoholism plays an important role .
What are the causes of liver failure?
There are acute and chronic liver failure.
Chronic liver failure is most often caused by cirrhosis and infection with hepatitis viruses (hepatitis B and C), which ultimately also leads to cirrhosis.
Cirrhosis
Cirrhosis is a disease in which fibrous reconstruction of the liver occurs, as a result of which its function is impaired. The most common cause of liver cirrhosis is alcohol abuse. Other, rarer causes include:
- autoimmune hepatitis;
- primary biliary cirrhosis;
- metabolic diseases;
- chronic use of certain medications.
Infection with hepatotropic viruses is a chronic infection. The liver is usually affected by viruses type B and C. In addition to cirrhosis, chronic hepatitis may predispose to the formation of hepatocellular carcinoma.
Acute liver failure is a sudden and rapid deterioration of liver function that after a few weeks leads to encephalopathy, bleeding disorders and, if untreated, death.
Causes of acute liver failure:
- acute viral hepatitis, mainly types A and B;
- some medications - most often paracetamol, halothane, sulfonamides, statins;
- poisoning;
- severe systemic diseases - shock, sepsis, portal vein thrombosis, etc.
3. Treatment of the disease
If liver failure caused by acetaminophen overdose is diagnosed early enough, the disease can sometimes be cured completely and all negative effects eliminated. Similarly in the case of a virus, if liver failure occurs due to a virus, supportive care in a hospital will help avoid serious consequences until the virus passes. In these cases, the liver can recover on its own.
For liver failure, when severe liver damage has already occurred, the first goal of treatment may be to preserve the part of the liver that is still able to function. If this is not possible, then a liver transplant is not required. But even in cases where a liver transplant is necessary, this operation is usually successful.
About our clinic Chistye Prudy metro station Medintercom page!
Symptoms of liver failure
Symptoms of liver cirrhosis develop slowly and are not noticed by the patient for a long time. At first, patients usually complain of weakness, itchy skin and jaundice. As the disease progresses, muscle atrophy and ascites appear - the patient's abdominal circumference increases, with rather thin limbs.
Other symptoms of liver cirrhosis:
- low-grade fever;
- lack of appetite, weight loss;
- vascular bundles on the skin;
- palmar erythema (redness);
- excessive hair growth in women;
- dilated venous vessels of the abdominal wall (“head of the jellyfish”);
- symptoms of hemorrhagic diathesis due to a deficiency of coagulation factors;
- ascites and pleural fluid - caused by albumin deficiency and leakage of fluid from blood vessels.
Low-grade fever
Lack of appetite
Sexual dysfunction also appears. As a result of disturbances in the metabolism of sex hormones, men experience symptoms of feminization - hair loss on the chest and armpits and gynecomastia, as well as hypogonadism - loss of libido. Women are diagnosed with menstrual irregularities.
2. Symptoms of the disease
The initial symptoms of liver failure are often similar to those of other diseases, including the most common ones. Because of this, liver failure can be difficult to diagnose early in the disease. The first signs of liver failure may be:
- Nausea;
- Loss of appetite;
- Fatigue;
- Diarrhea.
As liver failure progresses, symptoms become more severe and require immediate medical attention:
- Jaundice;
- Minor bleeding;
- Constipation;
- Mental disorientation and confusion (hepatic encephalopathy);
- Drowsiness;
- Coma.
Visit our Hepatology page
Complications of liver failure and cirrhosis
Cirrhosis leads to a serious complication - portal hypertension. This is an increase in blood pressure in the portal vein system, which, when transferred to subsequent vessels, causes collateral circulation in the form of, among other things, esophageal varices. This is a serious complication that can lead to massive gastrointestinal bleeding. This may be the first sign of cirrhosis.
Other complications of liver cirrhosis:
- Ascites is the accumulation of fluid in the abdominal cavity caused by a deficiency of albumin in the blood plasma;
- Spontaneous bacterial peritonitis caused by the penetration of bacteria from the intestinal lumen into the peritoneum. Pathogens cause infection of ascites fluid. In this case, the symptoms are rarely typical for peritonitis; fever, abdominal pain, and encephalopathy are usually observed;
- Hepatorenal syndrome, that is, deterioration of renal function in liver cirrhosis. The occurrence of this syndrome is an indicator of poor prognosis, as renal function may rapidly deteriorate, leading to end-stage renal disease with the need for dialysis in the short term;
- Hypersplenism is excessive splenic function causing pancytopenia in some patients;
- Acute liver failure. This is a sudden and rapid impairment of liver function, which mainly manifests itself in the rapid development of encephalopathy and the appearance of plasma coagulation disorders.
- Hepatic encephalopathy is a collection of neurological and psychological symptoms resulting from impaired elimination of toxins from the body. They enter the central nervous system, causing disturbances in consciousness, dementia, behavioral disorders and brain damage.
Symptoms of acute liver failure are plasma ecchymotic coagulation disorders, bleeding, and in rare cases, overt bleeding, usually from the gastrointestinal tract.
Prognosis for acute liver failure
Acute liver failure before the use of modern therapy and liver transplantation led to death in 80% of patients. Currently, this figure has been reduced to 40%. The cause of the disease and the presence of complications are the main factors determining the prognosis.
Patients with acetaminophen-induced liver failure have a better prognosis than those in whom the cause of the disease is unknown. The presence of cerebral edema, renal failure, coagulopathy, or infectious complications worsens the prognosis. Severe hepatic encephalopathy grade 3-4 is also associated with a greater risk of death.
Diagnosis of liver failure
When diagnosing liver failure, the patient's medical history is key. The facts of alcohol abuse and the presence of situations that increase the risk of hepatotropic viral infection are mainly important. Signs of organ failure are identified, for example, the degree of blood clotting disorder is assessed.
During a physical examination, the gastroenterologist notes an enlarged liver - the organ is relatively noticeable when palpating the abdominal wall.
A useful tool in diagnosing liver failure is abdominal ultrasound. The examination helps to accurately assess the size of the liver, its structure, as well as the width of the portal vein (important in the case of portal hypertension) and possible complications, for example, the presence of fluid in the abdominal cavity.
Abdominal ultrasound
Additional tests are laboratory tests, mainly the determination of transaminases and bilirubin, which allow indirect assessment of liver function. These tests should be performed periodically, and the frequency of tests depends on the rate at which symptoms worsen.
Sources
- Acute Liver Failure. Mescape. Updated: Jun 13 2022 — https://emedicine.medscape.com/article/177354-overview
- Pediatric Liver Transplantation. Medscape. Updated: March 17 2019 —https://emedicine.medscape.com/article/1012910-overview
- Liver Transplants. Medscape. Updated: December 31, 2022 — https://emedicine.medscape.com/article/776313-overview
- Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Pubmed - https://www.ncbi.nlm.nih.gov/pubmed/19524577
- Fulminant Hepatitis. Family Practice —https://www.fpnotebook.com/GI/Lvr/FlmntHpts.htm#fpnContent-panel-id_2
- Acute Liver Failure in Children. Medscape - https://www.medscape.com/viewarticle/584466_1
- The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. PubMed —https://www.ncbi.nlm.nih.gov/pubmed/16879891
- Cirrhosis. Medscape. Updated: 30 July 2017 —https://emedicine.medscape.com/article/185856-overview
- MELD Score for End-Stage Liver Disease (NOT appropriate for patients under the age of 12). Medscape —https://reference.medscape.com/calculator/meld-score-end-stage-liver-disease
- Acute liver failure. PostgradMed —https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1743234/pdf/v081p00148.pdf
- Modern prognostic models of survival of patients with terminal stage diseases. Journal of Clinical and Experimental Surgery - https://www.cesurg.ru/ru/jarticlescesurg/60.html?SSr=40013379b601ffffffff27c_07df070a01282f-690 12.Overview of the Indications and Contraindications for Liver Transplantation. PMC _ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996378/
- Liver transplantation for acute hepatic failure. PMC—https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2131363/
- Indications and Contraindications for Liver Transplantation. International Journal of Gepatology - https://www.hindawi.com/journals/ijh/2011/121862/
- Liver transplantation for chronic liver disease: advances and controversies in an era of organ shortages. Postgraduate Medical Journal - https://pmj.bmj.com/content/78/917/135
- Extracorporeal liver support. Organogenesis —https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3082035/
- Lifestyle Changes to Manage Cirrhosis. Winchester Hospital —https://www.winchesterhospital.org/health-library/article?id=19276
- What Are the Treatments for Cirrhosis?. WebMd —https://www.webmd.com/digestive-disorders/tc/cirrhosis-home-treatment#2
- Cirrhosis and Chronic Liver Failure: Part II. Complications and Treatment. American Family Physician - https://www.aafp.org/afp/2006/0901/p767.html https://www.aafp.org/afp/2006/0901/p767.html
- The use of extracorporeal methods for the treatment of liver failure. Kutepov Dmitry Evgenievich - https://cyberleninka.ru/article/n/ispolzovanie-ekstrakorporalnyh-metodov-lecheniya-pechyonochnoy-nedostatochnosti
In the conclusions of forensic medical examinations and in the reports of pathological autopsies of those who died from cirrhosis and, less often, from some other liver lesions, liver failure (LF) is often indicated as the direct cause of death. The basis for such a statement is, as a rule, the presence of hyperbilirubinemia and jaundice, high activity of alanine and aspartate aminotransferase in the blood serum. At the same time, it is quite obvious that these laboratory indicators are not evidence of functional failure of the organ.
The methodological prerequisite for overdiagnosis of PN is the extrapolation of the term “failure” to the liver by analogy with the generally accepted concepts of “renal failure” and “circulatory failure”. For renal failure, there are clear criteria in the form of impaired excretion of fluid and waste with an increase in their concentration in the blood, etc. In case of PN, perhaps the only criterion for insufficiency of organ function is the severity of neuropsychic disorders associated with the so-called hepatic encephalopathy (hepatargia) and caused by impaired assimilation of ammonia and some other nitrogenous substances in the liver with an increase in their concentration in the blood. In clinical practice, their concentration is not determined due to insufficient equipment of laboratory departments with appropriate equipment.
Along with this, hypoproteinemia, hypoprothrombinemia, hypofibrinogenemia, hypoalbuminemia, hypoglycemia associated with a decrease in the destruction of insulin by the affected liver, and hypokalemia due to secondary hyperaldosteronism can be considered signs of liver failure [1]. A forensic medical expert or pathologist does not always have this kind of data. In addition, even if they are present, they should be interpreted as a manifestation of PN only if other causes of a decrease in these indicators are excluded (blood loss, hemodilution, consumption coagulopathy, etc.) and only in their totality.
The activity of serum transaminases cannot be considered as an indicator of PN, since it reflects only the severity of damage to the liver parenchyma, but not the degree of its functional failure. This, for example, is the same as the activity of the MB fraction of creatine kinase indicates myocardial necrosis, but not the degree of heart failure. The activity of ALT and AST in the blood can only conditionally be explained by “cytolysis”, since even with dystrophic changes in hepatocytes, the activity of these enzymes increases [2], which is associated with their release (from the English leakage - seepage, leakage) outside the cell, the main structural components which can remain intact.
The content of total bilirubin in the blood without data on its fractions does not allow us to talk about PN. An increase in the amount of direct bilirubin in the blood indicates its reflux at the level of the hepatic beams or portal triads in conditions of blocking the outflow of bile, but not a violation of the liver. Unconjugated hyperbilirubinemia, in addition to hemolytic conditions and hemoglobinemia associated with the resorption of extensive hematomas, may be based on a number of “pre-hepatic” causes, such as a decrease in hepatic blood flow and, accordingly, the rate of acceptance of unconjugated bilirubin by the liver, an absolute insufficiency of transport albumin circulating in the blood, and its relative insufficiency , caused by the “occupancy” of part of the albumin by toxic or medicinal substances in the blood, or by conformational changes in part of the bilirubin molecules under conditions of changes in the physicochemical properties of the plasma, which makes fixation and delivery of unconjugated bilirubin to the liver impossible [3]. This also has nothing to do with the functional state of the liver.
Only parenchymal jaundice, in which indirect bilirubin is not fully captured by the altered hepatocytes and does not bind to glucuronic acid, but directly from the collapsing hepatocytes enters through the spaces of Disse into the tissue fluid, lymph and ultimately into the blood, can serve as an indirect indicator of PN.
In the presence of proven PN, in most cases the question of it as a possible direct cause of death is controversial.
In terms of its compensatory capabilities, the liver, which performs about 500 functions in the body, is a unique organ. Even with severe ischemic lesions, the volume of necrotic parenchyma does not exceed 46% [2], while according to experimental data, 10% of surviving hepatocytes is sufficient to maintain the vital functions of the body.
The high compensatory capabilities of the liver are also evidenced by cases of favorable outcomes in clinical practice with extensive resections of the organ. Chronic PN cannot be the direct cause of death. For the occurrence of death from acute PN, the decisive factor is the total or subtotal nature of the damage to hepatocytes, which is very rare. Such conditions include the fulminant form of viral hepatitis B with the development of “acute yellow toxic liver degeneration” or “subacute red toxic liver degeneration”, some poisoning with hepatotropic poisons: carbon tetrachloride, aflatoxin in case of poisoning with some low-quality plant products contaminated with fungus (in RF is not found) [4], fallotoxin and amanitotoxin in poisoning with pale grebes [5]. The development of acute PN as a reaction to certain drugs (rifampicin, isoniazid, paracetamol, etc.) has been described [4]. The author performed an autopsy on the corpse of a young man who was poisoned with fluorotane, which he used to achieve drug intoxication. It must be borne in mind that even if acute PN develops in such situations, it is not always the direct cause of death. During intensive therapy, patients and victims may die not from it, but from complications that have developed: for example, from abscess pneumonia [6]. The real basis for a conclusion about death from PN can only be records in the medical history about the clinical picture of hepatic encephalopathy (hepatic coma) when a corresponding liver lesion is detected at autopsy.
It should be noted that unsubstantiated judgments about the presence of PN in a patient are made not only after autopsy of the deceased. They are very often found in clinicians’ notes in medical records [7]. Even if the underlying disease (lesion) turns out to be correctly recognized, such records, when conflict situations arise, can serve as a reason to question the qualifications of the specialist who made them, with the extension of this view to his other conclusions.
Treatment of chronic liver failure
Drug therapy
| Ascites, edema | Salt-free diet, diuretics (spironolactone, furosemide) |
| Hepatic encephalopathy | Lactulose for detoxification, extracorporeal methods - MARS or Prometheus systems (FPSA), mannitol or barbiturates for cerebral edema |
| Infectious complications | Broad-spectrum antibiotics (cephalosporins) |
| Portal hypertension | Propranolol (prevention of bleeding from the veins of the esophagus) |
| Blood clotting disorder | Vitamin K, platelet transfusion, fresh frozen plasma, blood clotting factor preparations |
Drug therapy options are limited. Early diagnosis and prevention of complications are of primary importance. In case of alcoholic hepatitis, the use of ethyl alcohol, even in minimal doses, is strictly prohibited.
The only treatment method that can save the life of a patient with severe chronic liver failure is liver transplantation.
How long can a person live if the liver fails?
How long a patient can live with liver failure depends on the cause of the pathological condition. Considering the multifunctionality of the organ, when it is severely dysfunctional, not only the hepatobiliary system suffers, but the entire body. The prognosis depends on the severity of symptoms and treatment tactics. So, a person can live from a couple of days to several years.
Normal functioning of the body without the liver is impossible, therefore, if there is no chance of drug restoration of the functioning of the gland, its transplantation is performed. However, with continued exposure to the provoking factor, a relapse of the disease and repeated organ failure are possible.
Causes of chronic renal failure
The etiology of hepatic cell failure is varied:
- poisoning with alcohol, poisons;
- viral, fungal, bacterial, parasitic liver lesions;
- hepatitis C and B;
- cirrhosis;
- Botkin's disease;
- overuse of medications;
- ischemia;
- fatty liver degeneration.
Risk factors are:
- bleeding from the digestive tract;
- liver injuries due to road accidents, operations;
- cholelithiasis;
- chronic heart failure;
- intoxication.
Cherepenko Lyudmila Vikentievna
doctor - therapist • doctor - cardiologist
Rare causes of liver failure may include autoimmune diseases, abdominal surgery on the liver or nearby organs. Get a timely consultation with our doctor to identify the cause of the pathology and begin treatment.
Online consultation
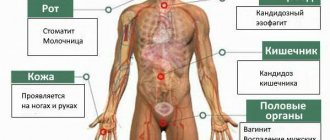
Liver Failure Symptoms
Signs of liver failure in humans are quite varied. They indicate damage not only to the hepatobiliary tract (gland, biliary tract), but also to other internal organs. This indicates the involvement of both the digestive and cardiovascular, nervous and circulatory systems in the pathological process.
Signs of liver failure include:
- jaundice;
- neuritis;
- hyperthermia up to 40 degrees;
- swelling of the limbs, ascites;
- encephalopathy;
- decreased libido;
- change in psycho-emotional state (irritability or apathy).
If the liver fails due to chronic glandular insufficiency, the person or his relatives may complain of:
- tremor of the limbs;
- disturbance of consciousness;
- disorientation;
- behavior change;
- slurred speech;
- inadequacy;
- severe swelling of the legs and abdomen;
- frequent nasal bleeding, prolonged menstruation;
- blurred vision.
If the pathology has an acute course, the following symptoms of liver failure in a person are observed:
- severe malaise;
- nausea, vomiting;
- hyperthermia;
- increased severity of jaundice;
- “liver” odor from the mouth;
- pain in the area of the right hypochondrium;
- lethargy;
- liver shrinkage.