Opportunistic infections, including mycoses, represent a pressing problem in modern medicine. Paradoxically, it was precisely the achievements of science that ensured the success of clinical medicine that led to an increase in the number of patients with opportunistic mycoses. In particular, advances in the treatment of a number of oncological and autoimmune diseases (the use of chemotherapy, anti-cytokine therapy, glucocorticosteroids and immunosuppressants) are associated with the emergence of a population of patients with acute and chronic iatrogenic immunodeficiency states. In turn, immunodeficiencies and local disorders of antimicrobial resistance in humans are the basis for the development of opportunistic mycoses, primarily candidiasis. Diagnosis and treatment of candidiasis of the mucous membranes of the digestive tract in some cases are associated with significant difficulties.
Fungi (Latin fungus, Greek mykes) are an independent vast kingdom of eukaryotic microorganisms, including about 90 thousand studied species. Until the end of the 1960s. Fungi were mistakenly classified as members of the plant kingdom. Among fungi, macromycetes and micromycetes are distinguished. The former are visible with the naked eye, the latter - with the help of microscopes. Unicellular (lower fungi, for example, Mucor) and multicellular (higher fungi, for example, Penicillium) forms of micromycetes are known [1].
Yeast-like fungi of the genus Candida are single-celled microorganisms 6–10 microns in size. These micromycetes are dimorphic: under different conditions they form both blastomycetes (bud cells) and pseudomycelia (threads of elongated cells). This morphological feature has, as will be shown below, important clinical significance.
Micromycetes of the genus Candida are characterized by ubiquity - widespread occurrence in the environment. Viable cells of Candida spp. can be found in soil, drinking water, food products, on the skin and mucous membranes of humans and animals. Thus, contact with these micromycetes of a person’s “open systems,” i.e., his skin and mucous membranes, is an ordinary fact.
Causes
Candidiasis (thrush) affects not only external but also internal organs. The cause of the disease is yeast-like fungi that live in the body of every person.
- Many factors can provoke intensive reproduction of the fungus. For example, hypothermia, illness, stress, changes in hormonal levels (during pregnancy or taking hormonal medications).
- When taking antibiotics, along with pathogenic bacteria, the beneficial microflora of the intestine and vagina, which controls the growth and development of Candida fungi, also dies. The presence of a chronic disease that reduces the activity of the immune system (HIV, sexually transmitted diseases, infections) very often causes candidiasis.
- Candidiasis may be accompanied by endocrine diseases (diabetes, obesity, thyroid dysfunction).
- Finally, candidiasis can be caused by a hot climate or wearing uncomfortable tight or synthetic underwear.
The source of infection with candidiasis, as a rule, is the body’s own flora (autoinfection), but infection can occur from the outside. When causing a disease, the fungus does not change its properties - the body changes its properties (local protection decreases). Attaching to epithelial cells, the pathogenic fungus begins to parasitize them, penetrating deep into the tissues.
In the body's fight against candidiasis, a dynamic balance often arises when the fungus tries to penetrate deeper into the tissue, but cannot, and the body tries to reject it and also cannot. In this case, the process can last for years; a shift in balance in one direction or another will lead either to recovery or to an aggravation of the process.
Candidiasis occurs in several forms depending on certain characteristics.
- Carriage. A person is a carrier of the disease. There are no symptoms of candidiasis and there is no need to treat.
- Acute. Accompanied by itching, rashes, and discharge. Treatment must be comprehensive and high quality. Young children are most often susceptible to infection.
- Chronic. Symptoms subside and manifest; relapses are possible. It develops if it is not treated correctly with antibiotics for a long time, or if hormonal contraceptives are used.
This disease has several varieties, since it does not have an exact localization in the body:
- Urogenital candidiasis in women.
- male.
- Thrush of the lips
- On skin folds (armpits, area between the buttocks, inguinal folds).
- Gastrointestinal tract (stomach, esophagus, intestines, anus).
Antifungal resistance
The outcome of contact with yeast-like fungi of the genus Candida is determined by the state of the human antifungal resistance system. In most cases, such contact represents a transient candidal carriage, when the structures and mechanisms of antifungal resistance ensure spontaneous decontamination of the human body. At the same time, in persons with disturbances in the antifungal resistance system, contact can form both persistent carriage and candidiasis. Thus, candidiasis of the digestive tract has typical features of an opportunistic infection. The disease of candidiasis of the mucous membranes is predetermined by the presence of the so-called fungi of the genus Candida. pathogenicity factors.
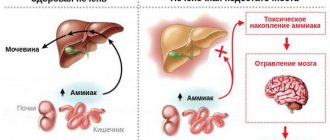
In particular, fungal cells can attach to epithelial cells (adhesion), and then, through transformation into a filamentous form (pseudomycelium), penetrate the mucous membrane, even “closed” systems (invasion), and cause necrosis of the tissues of the macroorganism due to the secretion of enzymes - aspartyl proteinases and fospholipases . The listed pathogenicity factors are naturally counteracted by numerous factors of antifungal resistance. In particular, the integrity of the epithelial layer of the digestive tract and mucopolysaccharides are of great importance. The protective role is played by the antagonism of yeast-like fungi and obligate bacteria of the digestive tract, the activity of digestive enzymes and the fungistatic effect of nonspecific humoral factors, such as lysozyme, complement, secretory IgA, transferrin, lactoferrin, etc.
However, the function of phagocytic cells, primarily polymorphonuclear leukocytes, and to a lesser extent, mononuclear phagocytes and natural killer cells, is of decisive importance in the system of antifungal resistance. The specific antifungal humoral response is realized due to the synthesis by B cells of specific anti-candidal antibodies of the classes IgA, IgM, IgG and, to a certain extent, IgE. Finally, the complex cooperation of dendritic and other antigen-presenting cells, helper types 1 and 2, and regulatory cells ensures an adequate specific immune response.
Symptoms of candidiasis
The disease is widespread. Pathogens of candidiasis have been found in the air, soil, vegetables, fruits, and confectionery products. Yeast-like fungi are found as saprophytes on healthy skin and mucous membranes.
Manifestations of candidiasis, and therefore symptoms and signs, depend on the location of the source of the disease.
Candidiasis of the oral mucosa (oral candidiasis, infantile thrush) most often occurs in children; as a rule, they become infected from the mother through the birth canal. Symptoms:
- the mucous membranes of the cheeks, pharynx, tongue and gums become red,
- swelling appears,
- then pockets of white cheesy plaque appear on the oral mucosa.
With candidiasis of the skin and its appendages, the lesions are most often located in large folds:
- inguinal-femoral,
- intergluteal,
- armpits,
- under the mammary glands.
The skin in the interdigital folds may be affected, more often in children and adults suffering from serious illnesses - on the skin of the palms, feet, smooth skin of the torso and limbs. Lesions in large folds look like small 1-2 mm bubbles, which soon open to form erosions. Erosion increases in size and merges, forming large areas of damage.
Foci of candidiasis have an irregular shape, dark red color, and around the lesion there is a strip of exfoliating epidermis. Outside the folds, the lesions look like red spots with peeling in the center, and occasionally small blisters may appear around the lesion.
Vaginal candidiasis (candidiasis, thrush) is an infectious disease of the vaginal mucosa, which often spreads to the neck of the uterus and vulva. Almost every woman has encountered this disease, and some signs of candidiasis are constantly disturbing. Most often occurs in women of reproductive age, but can occur in girls
Intestinal candidiasis (dysbacteriosis) often accompanies vaginal candidiasis or develops in isolation. Typically, intestinal candidiasis appears after taking antibiotics or previous intestinal infections. Fungi of the genus Candida settle in the small intestine. Symptoms characteristic of this type of candidiasis: white curdled flakes are often found in the stool of a patient suffering from intestinal candidiasis.
Esophageal candidiasis is a disease that is very difficult to identify among all those available in the field of gastroenterology. The disease is characterized by a discrepancy between the severity of the disease, the level of damage and the condition of the patient himself.
Oral candidiasis - symptoms and treatment
If treatment is untimely or incorrect, acute candidiasis can become complicated and become chronic or invasive, which is difficult to treat. In addition, complications such as fungal esophagitis, tracheitis, gastrointestinal candidiasis, and candidal sepsis may occur. There is a high probability of inflammation of the genital organs in women and men.
Candidal esophagitis (inflammation of the esophagus). Symptoms: signs of intoxication of the body, bloating, heartburn, sore throat, dysphagia (difficulty swallowing solid food), bitterness in the mouth or sour taste. Can lead to esophageal ulcers, rupture of the esophageal tube, internal bleeding, stricture (narrowing of the lumen) of the esophagus.
Candidal tracheitis (inflammation of the trachea). Symptoms: increased body temperature up to 37 °C, severe pain in the trachea, chest, shortness of breath and a feeling of suffocation when coughing, itching, burning, pain behind the sternum or between the shoulder blades, the appearance of ulcers on the skin. Through abscesses on the walls of the trachea, the fungus can penetrate into the blood, which will subsequently lead to sepsis.
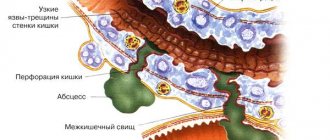
Candidiasis of the gastrointestinal tract . Candida penetrates the intestines and injures the mucous membrane, causing a severe form of dysbiosis. Symptoms: nausea, vomiting with blood and whitish films, increased body temperature to 37-38 °C, bloating and pain in the upper abdomen, diarrhea mixed with white flakes. If the stomach wall is perforated, serious consequences can occur, such as peritonitis (inflammation of the peritoneum) or internal bleeding.
Also a severe complication of oral candidiasis is candidal meningitis , which can be fatal. Most often, the complication occurs in patients with severe concomitant diseases (immunodeficiency, decompensated diabetes mellitus) and in people with reduced immunity. Candidal meningitis is manifested by the following symptoms: increased body temperature to 37.2-37.9 °C, cephalalgia (constant headaches), drowsiness, hemorrhagic rash throughout the body, vomiting, which does not bring relief to the patient, often without preceding nausea. Neurological symptoms may appear: disturbances of consciousness, higher nervous activity, movement disorders, sensitivity, vision.
The danger of the disease lies in a sharp decrease in the body's immunity and the rapid spread of infection to the spinal cord and brain. There are also difficulties in diagnosing the disease due to the erased symptoms and the absence of pronounced meningeal syndrome (signs of irritation of the meninges).
Attachment of a secondary infection. Inflamed organs and tissues are very sensitive to other infections. They penetrate most quickly through ulcers and cracks with bleeding. When a secondary infection is added, ulcerative necrotizing stomatitis or Vincent's tonsillitis, syphilitic seizure, syphilitic dysphonia (impaired vocal function), etc. may occur.
Candidal sepsis is the introduction of a fungal infection into the general bloodstream. A serious condition in which candida penetrates into all organs and tissues. Signs of intoxication of the body: nausea, vomiting, abdominal pain, tachycardia and body hyperthermia develop (increase in temperature above 38 ° C), multiple organ failure occurs (disruption of several functional systems of the body), and the activity of the central nervous system (CNS) is disrupted. In this condition, treatment is carried out only in intensive care units, since if assistance and special therapy are not provided in a timely manner, the outcome can be fatal [2].
Complication
With timely treatment, candidiasis does not cause any particular harm to health. But the symptoms of candidiasis can cause a lot of discomfort. Long-term, it can lead to damage to other organs, most often the urethra, bladder and kidneys. In particularly severe cases, the progressive disease can affect the reproductive organs, leading to infertility in both men and women. But candidiasis poses the greatest danger to pregnant women, because... the risk of fetal damage is very high.
An integrated approach to the treatment of patients with candidiasis of the digestive tract
Candida fungi are opportunistic microorganisms that normally populate the digestive tract, participate in the process of fermentation, food digestion, etc. This phenomenon, called colonization, is clinically asymptomatic. A study of adult healthy volunteers showed that Candida albicans was present in their oropharyngeal zone in 20–30%, in the small intestine – in 50–54%, in the large intestine – in 55–70%, in feces – in 65–70% of cases .
So, with physiological well-being, there is a certain balance between macro- and microorganisms, in which, on the one hand, factors of the body’s resistance to microscopic fungi play a role, on the other, factors of the pathogenicity of fungi. The body's resistance depends on belonging to risk groups and the competence of its immune system. For protection, macrophage and neutrophil phagocytosis is also important, preventing the dissemination of fungal, especially candidiasis, infection.
According to most researchers, the asymptomatic presence of fungi in the gastrointestinal tract (GIT) can cease when they acquire pathogenic properties, and the patient’s immune system fails.
The most common mycoses of the digestive tract are esophageal candidiasis and intestinal candidiasis, which occur both in immunocompetent and (much more often) in immunosuppressed individuals. Primary mycoses of the stomach, including candidiasis, are rarely diagnosed, which is associated with the physiological acidic environment of the stomach, where fungal cells die.
Risk factors for the development of candidiasis of the esophagus and intestines are:
1. Gastrointestinal diseases:
- diseases of the mucous membranes of the oral cavity;
- gastroesophageal reflux disease;
- stomach contamination with Helicobacter pylori;
- atrophic gastritis, gastric hypoacidity, achalasia, bulbitis;
- erosive and ulcerative diseases of the esophagus and intestines;
- mixed intestinal infection, dysbiosis;
- diverticulosis, polyposis;
- enterocolitis, Crohn's disease, irritable bowel syndrome, etc.
2. Other diseases:
- oncological;
- hematological;
- endocrinological;
- allergic;
- AIDS and HIV infection.
3. Injury to the gastrointestinal mucosa:
- esophagogastric tube;
- burns of the esophagus;
- surgical interventions.
4. Taking medications:
- antibiotics;
- cytostatics;
- hormones and other chemotherapy drugs.
Malnutrition, fasting, alcoholism, smoking, drug addiction contribute to the development of candidiasis. Risk factors also include old age, when the immune system ages, numerous somatic diseases occur, the amplitude of longitudinal contractions of the esophagus and the strength of sphincter contractions decrease, absorption processes are disrupted, etc.
Clinically, candidiasis of the digestive tract is divided into:
- oropharyngeal candidiasis (pseudomembranous, atrophic, erythromatous, rhomboid glossitis, angular cheilitis);
- candidal esophagitis (erosive and without erosion);
- gastric candidiasis (erosive-fibrinous and secondary to peptic ulcer);
- intestinal candidiasis (pseudomembranous, collagenous, lymphocytic);
- candidal proctosigmoiditis;
- perianal candidiasis;
- secretory diarrhea associated with candidiasis.
Candidal esophagitis in general hospitals occurs in 1.3–2.8% of patients, in transplant departments - up to 4%, with disseminated carcinomatosis - from 2.8 to 6.7%. This disease often occurs without subjective complaints and is detected incidentally in population studies in 1–7% of cases. Sometimes patients note pain and discomfort when passing solid and liquid food, dysphagia, and hypersalivation. According to the depth of the lesion, 4 types are endoscopically distinguished: from mild edema, hyperemia, single white plaques <1 mm in diameter to massive inflammation, deformation and bleeding of the mucosa, ulceration, even perforation.
Gastric candidiasis, as a rule, develops secondary to peptic ulcer and gastroesophageal reflux disease. Achlorhydria, in turn, promotes the colonization of fungi on the mucous membrane with subsequent invasion, especially in defect areas (ulcers, erosion), which slows down repair (healing), pain syndrome appears, and sometimes bleeding of the ulcer.
Candidiasis of the intestine usually manifests itself as abdominal discomfort, diarrhea, bloating, pain and other symptoms. The study of intestinal microbiocenosis makes it possible to specify amorphous “enterocolitis”, namely: to differentiate pseudomembranous colitis caused by Clostridium difficile, an acute process in the intestine caused by rotoviruses and Escherichia coli, Crohn’s disease, irritable bowel syndrome from candidiasis or dysbiosis with a predominant candidal component.
In most cases, fungal infections of the gastrointestinal tract are accompanied by changes in microbiocenosis and a decrease in the body's colonization resistance. To treat gastrointestinal candidiasis, a wide variety of antimycotics, both systemic and local, are used. Also, one of the goals of therapy is to create conditions for the growth and functioning of normal microflora.
In modern scientific literature, drugs for the correction of dysbiosis are divided into 3 main groups: probiotics - contain viable microorganisms; prebiotics – contain microflora growth stimulants; synbiotics – contain live microorganisms and prebiotics. There are probiotic complexes, which are a combination of the above components, as well as sorbents, vitamins and microelements. There are a lot of means for correcting intestinal microflora disorders, and new options and varieties are constantly appearing.
A further development of traditional probiotics are natural metabiotics. The terms "metabiotics", "metabolic probiotics", "postbiotics", "biological drugs" or "pharmacobiotics" are used to refer to small molecules that are structural components of probiotic (symbiotic) microorganisms and/or their metabolites, and/or signaling molecules with a specific (known) chemical structure that are capable of influencing the microbiome and/or metabolic and signaling pathways in humans. One of the representatives of metabiotics is Baktistatin.
The Baktistatin complex includes natural components that complement each other: sorbent, probiotic, prebiotic. One of the advantages of the Baktistatin complex is the absence of live bacteria foreign to the human gastrointestinal tract, the long-term presence of which in large quantities is undesirable. Instead of living bacteria, the Baktistatin complex includes products of their vital activity - active metabolites. Therefore, Baktistatin begins to work immediately, and its action is aimed at restoring one’s own normal microflora, which is unique to each person.
We conducted a study to evaluate the effectiveness and safety of the probiotic complex Baktistatin in treatment regimens for patients with candidal esophagitis and enterocolitis.
The study assessed the effectiveness and safety of 2 treatment regimens for esophageal and intestinal candidiasis in 2 groups: Group 1 – control, in which patients received etiotropic antifungal therapy; 2nd – the main group of patients in whom the Bactistatin complex is included in the above-mentioned therapy regimen.
In both groups of patients, selective decontamination with modern effective antifungal drugs of targeted action was carried out for 7–14 days. Patients in the main group additionally received Baktistatin, 2 capsules 2 times a day for 20 days.
To study clinical, endoscopic and laboratory indicators over time during the treatment of patients with candidal esophagitis and enterocolitis, a special questionnaire was developed, including a physical examination, gastroscopy, colonoscopy, and bacteriological examination of stool.
The results of comparing the scores of clinical symptoms showed that while taking the Baktistatin complex, manifestations of candidiasis of the esophagus and intestines went away faster. Thus, before treatment, the overall score for the severity of symptoms of candidal esophagitis was 355; after treatment, this figure decreased to 123 in the control group and to 60 in patients of the main group taking Bactistatin (Fig. 1). With regard to candidal enterocolitis, before treatment the total symptom severity score was 645, after treatment - 317 in the control group and 120 in the main group (Fig. 2).
In addition, the use of the Baktistatin complex in the treatment of gastrointestinal candidiasis significantly influenced the restoration of colon microbiocenosis due to an increase in the number of bifidobacteria and lactobacilli and a decrease in the number of enterobacteria, non-fermenting bacteria and fungi.
The data obtained indicate that the use of the metabiotic Baktistatin allows one to avoid the side effects of systemic antimycotics on the intestinal microflora and improve the condition of the esophagus and intestines in a short time due to a more pronounced reduction in the severity of the disease.
Thus, the use of the Baktistatin complex in treatment regimens for fungal infections of the gastrointestinal tract helps to quickly create conditions for the growth and functioning of normal microflora and reduce the side effects of systemic antimycotics.
How is the disease diagnosed?
Visual methods for diagnosing candidiasis. Upon examination, inflammation of areas of the skin is revealed, limited to a border of exfoliating, macerated epidermis, and a whitish coating on the mucous membranes.
Laboratory diagnostics. Contrary to popular belief, the main method for diagnosing candidiasis is still microscopy of a smear from the affected areas of the mucosa. PCR (DNA diagnostics), which has become popular recently, is usually poorly suited for diagnosing candidiasis.
Laboratory diagnosis of the disease includes:
- microscopy of discharge smear
- cultural diagnostics (seeding)
- enzyme immunoassay (ELISA)
- polymerase chain reaction (PCR).
What promotes the proliferation of Candida fungus in the intestines?
To avoid the development of intestinal candidiasis, you need to know what factors cause the disease. Only in this way can you partially avoid the risk of contracting such an unpleasant disease. The intestinal mucosa is affected by:
- when the endocrine system malfunctions, for example, with diabetes mellitus, adrenal tumors;
- for various diseases and pathologies of the gastrointestinal tract;
- in case of immunodeficiency caused by pregnancy, stress, nervous strain, depression, etc.
- physiological and psycho-emotional factors;
- when the patient has tumors;
- when there is a disturbance in the hematopoietic process;
- if there is HIV infection in the body;
- for autoimmune and allergic diseases requiring treatment with glucocorticosteroid drugs.
In addition to the main factors causing the development of intestinal candidiasis, you can get sick even if you fail to self-medicate simple infectious diseases with unknown drugs. For example, many people believe that by taking an antibiotic a couple of times you can very quickly recover from a particular disease. But at the same time, they forget that an antibiotic is not a solution to all problems; sometimes for recovery, it is enough to take a regular, safer pill.
Overuse of antibiotics disrupts the normal intestinal microflora and contributes to the development of intestinal candidiasis.
In addition, the disease can develop from excessive alcohol consumption, lack of protein in the daily diet, or irregular nutrition. In order to avoid this disease, you need to eat right, and the food should be nutritious and rich in healthy vitamins and microelements.
Treatment of candidiasis
Treatment of candidiasis is aimed at eliminating factors that contribute to the occurrence of candidiasis. If the skin is affected, local treatment is carried out using an open method using antifungal ointments.
The attending physician prescribes systemic and local medications for this disease. Local agents are not absorbed into the blood - they act only on the mucous membrane affected by the Candida fungus. They stop the reproduction and growth of fungi, relieve discomfort and restore affected tissue.
CANDIDIASIS OF THE ESOPHAGUS
Candidiasis is an infectious disease of the mucous membranes, skin and internal organs caused by yeast-like fungi of the genus Candida. Esophageal candidiasis (OC), which is a manifestation of visceral candidiasis, occupies a prominent place among infectious lesions of the esophagus. In recent years, there has been a tendency to increase the frequency of CP, especially in patients with impaired immunity. The growth of candidiasis infection is largely due to an increase in the number of patients with HIV infection, advances in transplantation and immunosuppressive therapy, and the uncontrolled use of antibiotics. KP occurs in 0.7-1.5% of gastroenterological patients [5, 6].
The problem with severe fungal infections caused by opportunistic pathogens is that they are difficult to treat and can be fatal. The mortality rate for invasive candidal infections has been found to be 34% [16].
Etiopathogenesis. Candida species are the most common esophageal pathogen, most notably Candida albicans, with occasional occurrences of C. tropicalis, C. parapsilosis, C. glabrata, C. lusitania, and C. krusei. These microorganisms are normal components of the oral flora and their growth is inhibited by bacterial commensals. Infection with fungi such as Candida, which are widespread in the environment, occurs through endogenous or exogenous routes. Endogenous infection is associated with the activation of saprophytic fungi; exogenous infection can occur through direct contact with carriers of infection or from the environment. If the host's body is not weakened, many fungi do not exhibit their pathogenic properties. Research in recent years has shown that the source of fungal dissemination is the intestines, and candidiasis of the oral cavity, genitals, and esophagus is a manifestation of systemic candidiasis. The likelihood of developing systemic damage depends both on the properties of the microorganism itself (their number, virulence, genetic and species heterogeneity of the population), and on the state of the macroorganism, especially its immune system, nutritional status and abdominal blood flow [3, 17].
Favorable conditions for the development of the infectious process are created by various violations of the physiological, anatomical and immunological mechanisms of the body's defense. Factors that provoke the occurrence of esophageal candidiasis include the use of antibiotics, inhaled or injected corticosteroids, antacid therapy or a hypochlorhydric state, diabetes mellitus, alcoholism, the consequences of intoxication, malnutrition, old age, impaired motility of the esophagus or esophageal obstruction, organ and bone marrow transplantation , enteral and especially parenteral nutrition, etc. A weakened immune system can lead to candidiasis infection. In diabetes mellitus, elevated blood glucose levels promote fungal growth because hyperglycemia impairs granulocyte function. Hypofunction of the parathyroid glands and adrenal glands leads to disruption of calcium-phosphorus metabolism, which causes hidden spasmophilia of the esophagus, thereby reducing its local protective capabilities [9]. Impaired nutritional status due to a lack of protein in the body and low calorie food affects the state of the immune system and creates the preconditions for the development of candidiasis [3]. Risk factors for candidiasis include a decrease in the acidity of gastric juice (pH 7.4 is optimal for the growth of Candida fungi, and when the pH shifts to 4.5, fungal growth is completely inhibited) [3, 4, 7].
The pathological manifestations of KP are varied. At first, the affected areas of the esophagus have the appearance of individual whitish or yellowish lesions raised above the mucous membrane. Later, these lesions can merge, forming dense plaques with the introduction of the fungus into the submucosa or pseudomembranous deposits with the penetration of the fungus into the muscular layer and blood vessels [9]. Films that form on the esophageal mucosa in especially severe cases can almost completely close the lumen of the esophagus. Plaque consists of desquamated epithelial cells that mix with fungi, inflammatory cells and bacteria. Microscopic examination reveals uniformly colored yeast-like cells and filaments of mycelium of Candida fungi [9]. True ulceration is observed infrequently and in most cases is observed in immunosuppressed patients with granulocytopenia [29]. Sometimes necrosis of the esophageal wall occurs and phlegmonous inflammation of the esophagus and mediastinum develops, which can become one of the causes of death of the patient [1].
There is a morphological classification, according to which all cases of KP are divided into three groups depending on the severity of the process, that is, depending on the depth of damage to its wall: 1st group - individual whitish plaques with the introduction of pseudomycelium of the fungus between the epithelial cells; 2nd group - membranous plaques merging with each other and forming vast fields, while filaments of pseudomycelium grow not only the mucosa, but also the submucosa; Group 3 - pseudomembranous overlays, combined with deep changes, in which the threads of the fungus penetrate deeply into the thickness of the muscle tissue [10].
Clinical manifestations and complications. Symptoms of the disease are practically absent in 25-30% of patients suffering from KP, especially in immunocompetent individuals. However, most patients present with complaints related to damage to the gastrointestinal tract. The most typical clinical manifestations of KP are dysphagia and, somewhat less commonly, odynophagia. The severity of esophageal symptoms ranges from moderate difficulty swallowing to severe pain, resulting in the inability to eat and the development of secondary dehydration. In severe odynophagia, there may be other causes or co-infection, especially in patients with AIDS. Much less frequently, patients may complain of chest pain not associated with swallowing, heartburn, nausea, sometimes vomiting with the release of films (pseudomembranes), decreased appetite and weight, and the appearance of loose stools with mucus (see figure) [4, 9, 29].
| Symptoms of candidal esophagitis (RS Orlando, 1996) |
Physical examination may be helpful in KP. Approximately two thirds of patients with
AIDS and esophageal candidiasis have candidal stomatitis. KP is observed in patients with chronic mucocutaneous candidiasis, which is a severe form of candidal infection and is more often observed with dysfunction of the adrenal glands and parathyroid glands [29].
Complications of esophageal candidiasis are rare. Esophageal bleeding can be observed in severe cases of the disease, accompanied by the formation of erosions, ulcers, and be associated with coagulopathy; perforation may develop. Secondary obstruction of the lumen by mycetoma has been described. Necrosis rarely occurs with the development of phlegmonous inflammation of the esophagus and mediastinum [1]. In severe cases, specific esophagitis can be complicated by the development of candidiasis sepsis [6].
Diagnostics. Suspicion of esophageal candidiasis should arise in any patient if there are risk factors for the development of esophageal infection and complaints of dysphagia and odynophagia. The presence of candidal stomatitis confirms this diagnosis, but in its absence, damage to the esophagus is also not excluded.
Barium x-ray of the esophagus is usually used for initial evaluation before endoscopy. However, in the early stages of candidal esophagitis, X-ray examination of the esophagus does not have much diagnostic value, since it reflects only nonspecific changes common to all esophagitis [2]. Classic radiographic signs of acute esophagitis caused by Candida spp. are linear or irregular filling defects with clear edges. In severe cases of candidal esophagitis, fusion of lesions occurs, which is why large filling defects sometimes form clusters in the form of bunches of grapes [2]. In this case, the esophagus acquires a “shaggy” (“hairy”) appearance, simulating ulceration [25]. The presence of large, well-circumscribed ulcers is not a sign of candidal esophagitis. Impaired motility and narrowing of the lumen of the esophagus due to pseudomembranes may occur. It should be remembered that a normal barium radiograph of the esophagus does not exclude esophageal candidiasis. Due to severe odynophagia, the patient will not be able to drink barium, which makes X-rays of the esophagus difficult [29].
The double contrast radiological method is considered more informative for the diagnosis of candidal esophagitis, the effectiveness of which reaches 70% [26].
A cytology brush and balloon catheter are used to quickly diagnose esophageal infections without endoscopy. These instruments can be easily inserted through the nasal passages or the mouth through a protective probe that prevents contamination. The material obtained from the protected brush or balloon catheter after it is removed from the esophagus is evaluated cytologically and culturally. The technique using protected brushes has a sensitivity of 88% and a specificity of almost 100% [26].
The cytological method involves staining impression smears or swab sediment from a cytological brush in search of active forms of Candida - budding yeast cells, pseudomycelium and mycelium. The cultural method involves placing the test material on Sabouraud's glucose-enriched medium or other media, in order to then judge the etiology of the infectious process in the esophagus by the nature of the colonies formed.
Endoscopic examination of the esophagus is the most sensitive and specific method for diagnosing esophageal candidiasis. The endoscopic picture of KP is most often characterized by the presence of easily removable fibrinous loose overlays of white or yellow color, under which easily wounded and/or edematous mucosa is found. Catarrhal and erosive-ulcerative esophagitis are less common [19]. Candida spp. rarely causes true ulceration. The presence of an ulcer in candidal esophagitis is often a sign of an additional pathological process in the esophagus [29]. There are various endoscopic classifications of esophageal candidiasis (Tables 1 and 2).
During endoscopy, affected areas of the mucosa may be subjected to brush biopsy for cytological examination or biopsy for histological diagnosis. When ulcers are identified endoscopically, repeated biopsies help rule out the presence of coexisting pathological processes. Cytological examination of brush biopsy material has a higher sensitivity level than histological examination of biopsy specimens for mild superficial candidiasis because microorganisms may be washed off the tissue surface during processing of the biopsy material [19]. In rare cases, positive cytology in the presence of negative histology indicates colonization rather than infection. For more severe candidiasis of the esophagus, the greatest diagnostic value is histological examination of mucosal biopsies using special staining for neutral mucopolysaccharides according to Schiff PAS (CHIK reaction) or according to Gomori with silver hexamethylenetetramine. Only histological examination demonstrates invasion of the mycelium or pseudomycelium of the fungus deep into the tissue of the esophagus.
Skin testing and serological tests are not very informative for diagnosing esophageal candidiasis.
Treatment. There are many oral and intravenous medications that are used to treat candidiasis esophagitis. Despite the relatively wide choice of drugs, the treatment of KP is an urgent problem, since some drugs are not effective enough, others have serious side effects; In addition, there is currently an increase in resistance to antifungal drugs.
When treating KP, oral therapy should initially be prescribed; intravenous administration is used only in case of refractory disease or if there are contraindications to oral use of medications. Patients with moderate severity of the disease and minimal immunocompromise require a short course of therapy using systemically absorbed drugs such as oral azole. Immunocompromised transplant patients and AIDS patients with KP are best treated with longer courses of azole. In patients with granulocytopenia, when there is a significant risk of dissemination of Candida infection, the use of intravenous systemic drugs (azoles, amphotericin B) is justified [29].
The arsenal of modern antifungal agents is quite wide. Antifungal drugs of several groups are used to treat esophageal candidiasis. The most effective drugs are from the azole group. Non-absorbable azoles (clotrimazole, miconazole) are used orally; however, systemic drugs from this group (ketoconazole, fluconazole and itraconazole) are more effective. These drugs, like others in the azole group, alter fungal cell membrane permeability through cytochrome P450 (CYP)-dependent interference with ergosterol biosynthesis, resulting in fungal cell damage and death. New triazoles (itraconazole and fluconazole) have higher affinity similarity than imidazoles (miconazole and ketoconazole) for fungal CYP enzymes [14]. Although other drugs, such as miconazole, clotrimazole, and nystatin, can be used to treat candidal stomatitis, as well as to prevent esophageal lesions, these drugs are less effective as the main group of drugs for the treatment of KP [24].
Clotrimazole and miconazole are imidazole drugs. Clotrimazole tablets and miconazole for oral use are currently available. However, they are not absorbed from the gastrointestinal tract. These drugs can be used for mild candidiasis of the esophagus in people without immunodeficiency.
Ketoconazole (nizoral, oronazole) is an imidazole derivative and, when taken daily in a dose of 200 to 400 mg, gives a good effect in the treatment of esophageal candidiasis. In AIDS patients who usually require higher doses of ketoconazole, the daily dose can be increased, if nausea does not occur, to the maximum (800 mg). Ketoconazole penetrates well into various organs and tissues, but poorly through the blood-brain barrier. The drug is well absorbed from the gastrointestinal tract, but requires an acidic environment for optimal absorption. With gastric hypochlorhydria and the use of antacids, its bioavailability decreases. To improve absorption, ketoconazole should be taken 2 hours before taking antiulcer medications. Approximately 10-25% of AIDS patients experience decreased gastric acid secretion. Ketoconazole can cause a temporary blockade of the synthesis of testosterone and cortisol [6, 8, 29].
Itraconazole (Sporanox) belongs to the group of triazoles, like ketoconazole, and is prescribed at a dose of 200 mg per day. Further increases in the dose lengthen the half-life of the drug and increase its effectiveness. The absorption of intraconazole decreases when the pH of gastric juice decreases [23]. Ketoconazole and itraconazole are metabolized in the liver and excreted in the bile. The half-lives of these two drugs are 7 to 10 hours and 24 to 42 hours, respectively [14]. No dose adjustment is required in patients with renal failure.
Fluconazole (Diflucan, Diflazon, Forkan, Flucostat - domestic fluconazole) is a water-soluble triazole and is prescribed at a dose of 100 mg per day. Fluconazole is a drug whose absorption is independent of gastric pH and is significantly more effective in the treatment of esophageal candidiasis in AIDS than ketoconazole (200 mg daily) [21]. Fluconazole is available for oral and intravenous use. It is minimally metabolized and excreted unchanged in the urine. Fluconazole has a high tissue tropism and does not affect the synthesis of androgens and penetrates well through the blood-brain barrier. Unlike ketoconazole and intraconazole, it is highly soluble in water and minimally protein bound. The drug has a long half-life (approximately 30 hours, unless renal function is impaired and the presence of food or hypochlorhydria does not alter absorption), allowing it to be taken once daily. It has been shown that the administration of fluconazole improves immune parameters in the T- and B-systems [18]. Both fluconazole and itraconazole can be taken orally as solutions. These forms may be more effective than tablets because they enhance the local effect and improve absorption.
Adverse effects of ketoconazole, fluconazole and itraconazole are primarily dose dependent and include nausea, hepatotoxicity, decreased steroid production and cyclosporine metabolism [14]. In rare cases, ketoconazole can cause fatal hepatitis [12]. A slight increase in aminotransferases is a common side effect of all three drugs, but this should not be used as an excuse to discontinue them. The effect on steroidogenesis is most pronounced with ketoconazole. Reversible inhibition of gonadal and adrenal steroid synthesis by ketoconazole may occur when the dose exceeds 400 mg per day [27]. At recommended doses, fluconazole and itraconazole do not affect steroidogenesis. As a result of their effects on hepatic microsomal enzymes, all three azoles inhibit the metabolism of cyclosporine, which leads to an increase in the level of cyclosporine in the blood; this effect is most pronounced with ketoconazole [14].
Another main group of antifungal agents is polyene antibiotics, represented by amphotericin and nystatin. These drugs irreversibly bind to sterols in fungal cell membranes, thereby altering the permeability properties of the membrane, disrupting its barrier function and causing cell death. Nystatin (anticandin, mycostatin, fungicidin) is practically not absorbed from the gastrointestinal tract. It is used to treat candidal stomatitis, but is less effective in cases of esophageal candidiasis. In addition, the effectiveness, safety and ease of use of azole derivatives make it possible to consider nystatin as a second-line therapy. Amphotericin B (amphostat, fungizone) is the only polyene antibiotic for parenteral administration. It is not absorbed in the gastrointestinal tract, is used intravenously, penetrates well into various organs and tissues, and is excreted from the body by the kidneys. The half-life is 24-48 hours, but with systematic use it can increase to 15 days due to accumulation in tissues [8]. Although amphotericin B is the most effective drug used to treat systemic mycoses, its use in the treatment of KP is limited due to serious side effects. Side effects of amphotericin include neurotoxicity, hematoxicity, nephrotoxicity, local irritation (phlebitis), allergic reactions, dyspeptic disorders, fever, etc. [8]. The most adverse side effect resulting from long-term use of amphotericin is nephrotoxicity, which is usually reversible. This medication is now available as an oral solution and lozenges. In patients with KP who are refractory to treatment with fluconazole or other azoles, low doses of intravenous amphotericin B (10 to 20 mg daily) may be effective. The total dose of the drug for the treatment of esophageal candidiasis ranges from 100 to 200 mg [29].
Flucytosine is a drug with a narrow spectrum of antifungal activity that works by interfering with RNA translation. It is incorporated into fungal cells, where it is converted into 5-fluorouracil and inhibits thymidylate synthetase. This oral drug, which is given at a dose of 50 to 150 mg/kg per day every 6 hours, can be used in combination with amphotericin B, but it should not be used as monotherapy because fungi quickly become resistant to it. In addition, flucytosine monotherapy appears to be only moderately effective [12].
The newest class of antifungal drugs are candins, which interfere with the synthesis of the fungal wall. They are effective against most Candida species, including C. krusei. The first studies showed that capsofungin, which represents this group of drugs, was as effective in KP as amphotericin B [16].
When treating patients with KP, one should take into account the presence of resistance, which has now increased significantly due to the widespread use of azoles. If resistance develops, it is often useful to increase the azole dose. If this is not enough, switch to another drug from this group or use an oral solution of itraconazole [13], which must be prescribed in higher doses due to frequently observed cross-resistance. When a high dose (i.e. 400 mg daily) of fluconazole is not enough, switch to intravenous amphotericin B, and the result is achieved in 90% of cases. Resistance to amphotericin is rare [29].
In table 3 presents the treatment of candidal esophagitis depending on the function of lymphocytes and granulocytes.
In the treatment of candidal esophagitis in patients with AIDS, the first-line drugs are ketoconazole and fluconazole, with fluconazole being preferred. Due to better tolerability, it is primarily indicated for patients at an advanced stage of the disease who have many comorbidities. If swallowing is impaired, parenteral forms of fluconazole can be used. If first-line drugs are ineffective, drugs from the reserve group (amphotericin B, itraconazole), which are more toxic and/or more expensive, are used. Etiotropic therapy of esophageal candidiasis, in addition to the main course of treatment, requires maintenance treatment, which can be lifelong (Table 4) [4].
Treatment of candidiasis against the background of severe immunodeficiency and leukopenia is a difficult task. Along with antifungal therapy, it is important to restore the pool of neutrophil leukocytes and their functional activity, since neutrophil leukocytes are one of the main links in the defense mechanism against Candida spp. It is proposed as an additional agent in the treatment of candidal infection against the background of neutropenia to use granulocyte colony-stimulating factor, which reduces the deficiency of myeloperoxidase in neutrophil leukocytes and enhances their oxygen-dependent anti-candidal activity [7]. A good effect has been obtained from the endoscopic administration of granulocyte concentrate and high-intensity pulsed laser radiation to patients with KP, which improves immune functions [5].
Thus, to achieve success in patients with severe fungal infections, including candidiasis, an integrated approach to diagnosis and treatment is advisable. Increased survival will be facilitated by prompt diagnosis followed by the selection of effective specific antifungal therapy and therapeutic measures aimed at increasing the number of granulocytes and stimulating phagocytosis [16].
For questions about literature, please contact the editor