The problem of constipation in children at an early age worries parents and pediatricians. Kids strain aimlessly, scream from pain and a swollen belly, and refuse to eat. Most often they are caused by the child's diet.
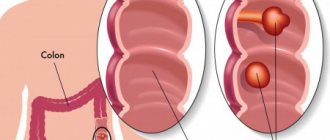
But with a constant tendency to retain stool, a suspicion of pathology of the large intestine arises. Dolichosigma in children is a disease caused by too long sigmoid colon. At the same time, the thickness of the walls remains normal, so the diameter of the lumen can only change when twisting or bending the “extra” movable loops.
Formation mechanism
Doctors believe that anomaly in the length of the sigmoid intestine is quite common in children. During examination, it is found in 25% of newborns. In most cases, the child does not feel the pathology, so it is recognized as an individual physiological deviation.
Pathological dolichosigmoid changes in the intestine are considered when disturbances occur in the formation of feces and motor function in delivering them to the anus. Up to 30% of cases are recognized as congenital anomalies in the formation of the fetal intestinal tube. The rest can occur in a child in an acquired manner due to impaired digestion, putrefactive fermentation in the sigmoid colon, its distension with gases and feces, and the formation of new loops.
Not all pediatricians agree with this interpretation. Some believe that in childhood there cannot be enough causes for an acquired disease. The pathology is present from birth, but does not immediately manifest itself. It is provoked by improper nutrition of the nursing mother and baby, and lack of sufficient child care.
Traditional medicine methods
Home recipes are used only after consultation with a doctor. Self-therapy at a severe stage of dolichosigma often leads to the death of the baby, since attempts to move feces provoke the development of intestinal obstruction. If the doctor has approved home treatment, then the following will help in the fight against constipation:
- Flax seeds. Pour 1 tbsp. l. flaxseed 100 ml of boiling water, leave for half an hour, then strain. Use the solution from the first year of life, 2.5-5 ml 1-2 times a day for 10 days.
- Hop cones. Fill with bread kvass (dark) in a ratio of 1:20. Store in the refrigerator. Stir the solution thoroughly before each use. Give a child from 2 years of age to drink in the morning and evening at a dosage of 1 ml/kg body weight. Duration of therapy – 7 days.
- Castor oil. Give a child after 1 year 0.5 teaspoon 1 time/day. You should not take castor oil in childhood for more than 2 days in a row.
The main causes
It is not yet possible to accurately indicate the cause of dolichosigma in children. Predisposing factors and conditions of the disease have been studied. These include:
- complicated pregnancy of the expectant mother;
- the impact on the fetus of infectious diseases and toxic medications suffered by a pregnant woman;
- lack of vitamins and protein products in the mother’s diet;
- exposure of the fetus to environmental conditions (gas pollution, increased radiation, poor quality of drinking water);
- unfavorable heredity.
The expectant mother should not rely on her own choice of medication
How do the symptoms appear?
Symptoms of the disease develop gradually in the child. How pronounced the manifestations are depends on the degree of elongation of the intestine and the body’s ability to compensate for peristalsis at the expense of other areas. In 2/3 of cases, children under one year old are affected. The main symptom is constipation. They appear when switching to complementary feeding or stopping breastfeeding. They are provoked by a change in the composition of feces, an increase in volume.
In 30% of children, defecation disorders occur between the ages of 3 and 6 years. Gradually, cleansing the intestines becomes a problem for the child; there is no bowel movement for 3-4 days. In addition, there are:
Why does a 3 year old child have a stomach ache?
- abdominal pain, children react sharply to palpation of the iliac region on the left and closer to the navel;
- bloating due to accumulated gases in the intestines;
- increased hardness of stool consistency, relatively large diameter of discharge;
- blood impurities due to damage to the vessels of the intestinal mucosa by the stone masses;
- smell from the child's mouth;
- signs of vitamin deficiency (brittle nails, sticky spots in the corners of the mouth);
- anemia (anemia), pale skin, blue lips.
Older children complain of increased fatigue, palpitations, refuse food and active games, and do not gain weight well. Inflammatory diseases of the stomach (gastritis) with nausea, vomiting, damage to the biliary system and pancreas are possible.
Dolichosigma of the intestine in a child causes an imbalance in the microflora of the large intestine. It is the loss of healthy bacteria that contributes to vitamin deficiency. Children are prone to irritability, tearfulness, and often suffer from colds. A decrease in local immunity is accompanied by skin manifestations in the form of small pustules.
One of the signs of vitamin deficiency is peeling skin on the fingers
Signs of the disease
Clinical manifestations of the disease are caused by functional changes in the colon and chronic fecal intoxication. The leading manifestation of dolichosigma is persistent constipation, which can last up to 10 days in a row. Due to prolonged absence of bowel movements, a child may experience unexpected bowel movements that he cannot control. The feces come out slowly, painfully, have an unpleasant odor, and have a thick consistency.
First symptoms
The timing of the development of pathological symptoms varies. They depend on the degree of elongation of the intestine, changes in its motility and tone, and the compensatory capabilities of the body. Most often, dolichosigma develops at the age of 6-12 months. This is due to the introduction of complementary feeding or the transfer of the baby to artificial (mixed) feeding, which entails an increase in the quantity and thickening of the consistency of stool. The first symptoms of dolichosigma:
- constipation is episodic, no stool for 2-3 days;
- dilatation (stretching) of the intestine, worsening morphological changes;
- decreased reflex to defecate;
- encopresis (fecal incontinence).
In later stages
With further development of the pathological process, the frequency and duration of constipation increase. Feces in children become large in diameter, sometimes resemble a fir cone, and often have a foul odor. Damage to the rectum during the passage of dense feces causes the appearance of scarlet blood in the stool. Characteristic clinical signs at the late stage of dolichosigma in a child:
- recurrent pain in the umbilical or left iliac region;
- flatulence;
- intestinal spasm;
- formation of fecal stones;
- inflammatory processes in the intestinal wall;
- cicatricial changes in the sigmoid mesentery.
Course of the disease
The development of dolichosigma in a child goes through 3 stages. Some pediatricians call them forms. They differ in the severity of symptoms and response to treatment measures.
- I (compensation stage) - the mildest, the child’s constipation is not constant, lasts for 2-3 days, the pain is not severe, disappears after defecation. The general condition is good, the baby’s activity and development are not affected. It responds well to diet and mild laxatives.
- II (stage of subcompensation) - constipation becomes habitual, no bowel movements for more than three days. Abdominal bloating and pain appear. The child is irritable, eats poorly, and is underweight. To cleanse the intestines you have to use enemas, diets and laxatives are not enough.
- III (stage of decompensation) - the picture of the disease is pronounced, the symptoms are advanced. The child suffers from prolonged constipation, there are signs of intoxication (headaches, lethargy, nausea, vomiting), anemia and vitamin deficiency. Abdominal pain and bloating persist constantly. Attacks of partial intestinal obstruction occur. Only siphon enemas help cleanse a child’s intestines. This condition can only be effectively treated with surgery.
What methods of diagnosing dolichosigma are used in pediatric practice?
The doctor carefully performs a digital examination of the rectum. With constipation caused by dolichosigma, it turns out to be empty. Palpation of the abdomen indicates a lesion in the descending zone of the large intestine. Sometimes it is possible to feel hard fecal stones through the child's thin abdominal wall.
Diagnostic tests of blood, urine and feces in this case are not decisive. But they are necessary to identify complications, inflammation of the intestines, urinary organs, and diseases.
Therefore, it is necessary to appoint:
- blood test (leukocytosis, increased ESR, hemoglobin level, red blood cell count are important);
- stool (mucus, hidden and obvious blood, purulent impurities, leukocytes, undigested particles), checked for the presence of parasitic infection;
- in the urine there may be signs indicating the transition of inflammation from the intestines (mucus, leukocytosis, bacteria, red blood cells).
It is possible to detect sigma elongation in young children only with the help of irrigography after administration of a barium suspension with an enema. For older children, taking barium in solution followed by a series of pictures of the stomach and intestines is suitable.
A different x-ray picture allows you to distinguish dolichosigma from similar diseases
Ultrasound allows you to examine the intestine clogged with dense feces. Computed tomography in childhood is impossible because it requires the patient to be in a calm, immobile state. If differential diagnosis is necessary, colonoscopy is performed under short anesthesia with a thin pediatric probe. Administration through the rectum makes it possible to examine the large intestine and assess damage to the mucosa
The child is prepared for the examination with cleansing enemas and laxatives.
Constipation in children: modern approaches and treatment tactics
Choosing an effective treatment for chronic constipation in children is a major challenge for pediatricians. The incidence of this pathology in children under one year of age is 17.6% (1), and at older ages it is 10–25% [2]. Features of the development of the large intestine in children explain many of the clinical symptoms of impaired motility, leading to the development of chronic constipation.
The growth of the large intestine in the prenatal period lags behind the growth of the small intestine, and in the newborn the ratio between the length of the small and large intestines is 5.6:1. Up to three years, both parts of the intestine grow equally rapidly, but in subsequent periods the large intestine shows a faster growth rate, and the ratio between the two parts of the intestine becomes equal to 4.6: 1. In newborns, the cecum is located high, the ascending colon is shorter than the descending colon, the sigmoid colon is long and forms kinks. The structure of the wall of the colon is characterized by weak development of muscle bands, swellings and omental appendages.
The colon in newborns and children under one year of age is usually horseshoe-shaped, its bends are weakly expressed. The transverse colon has a short mesentery and is inactive. In the first 1.5 years of a child’s life, the mesentery lengthens 3–4 times. Already in early childhood, differences in the length and position of the transverse colon are observed. It can be located transversely, go in an oblique upward direction and sag in the form of the letter V. The dependence of the position of the transverse colon on the shape of the abdomen and the lower aperture of the chest has been noted. With a wide aperture, the intestine is most often located horizontally; with a narrow aperture, it sags to a greater or lesser extent.
The sigmoid colon in newborns has a long mesentery; its loops can be located in different areas of the abdomen. In the first years of life, the intestine is located high. After 5 years, it descends more and more into the pelvic cavity. The mesentery in the postnatal period is relatively shortened, and the intestine becomes more fixed.
The rectum of newborns is relatively long, its bends are weakly expressed, and the walls are thin. The intestine occupies almost the entire pelvic cavity. During the first year, the rectal ampulla is formed. The severity of the ampulla varies individually (in adults, there are two main forms of the rectum: ampullary, with a well-developed ampulla, and cylindrical, without a pronounced ampulla). In the circumference of the rectum there is connective tissue that plays a role in fixing the organ. In early childhood, it is poorly developed, which creates the preconditions for rectal prolapse with increased intra-abdominal pressure, abdominal tension with severe coughing, straining, etc.
Disorders of the act of defecation in young children, with incomplete fixation of parts of the colon, contribute to the formation of pathological mobility and kinks of the colon, which leads to a slowdown in the passage of intestinal contents.
The cause of disruption of the movement of feces through the colon can also be such developmental anomalies as colon hyperplasia (syn.: congenital gigantism of the colon) - expansion and lengthening of the colon. There are several options:
a) dolichosigma - congenital elongation of the sigmoid colon without elements of its expansion. The intestine, as a rule, forms 2–3 or more additional loops; b) megadolichosigma (syn.: dolichomegasigma) - elongation of the sigmoid colon with expansion, reaching 10–20 cm in children, and thickening of the wall; c) dolichocolon - elongation of the large intestine due to excessive growth in length of the transverse colon, descending and sigmoid colons without its expansion; d) megadolichocolon - elongation is accompanied by a uniform expansion of the intestinal lumen, hypertrophy of its wall and the absence of haustra.
During the first visit to a newborn, a pediatrician should examine the anal area and evaluate the anorectal index (ARI) in order to exclude ectopia of the anus. ARI is the quotient of the distance between the vagina or scrotum and the anus (cm) divided by the distance between the vagina or scrotum and the coccyx (cm). Normally, in girls the ARI is 0.45 ± 0.08, in boys - 0.54 ± 0.07 [3], with anterior displacement (ectopia) of the anus, the ARI decreases - in girls <0.34, and in boys < 0.46 [4].
Examination of the anal area should be a mandatory part of a general medical examination. It is well known from practice that many developmental defects manifest themselves some time after the birth of a child, so even experienced doctors may not see them during an examination in the maternity hospital. Below we will look at malformations of the rectum and anorectal region, which may be accompanied by constipation.
Rectal atresia - occurs in 2.5–6.6 children per 10,000 births. Currently, mutations in the Sonic hedgehog (Shh), Gli2 and Gli3, and Ephrin-b2 lacz/Lacz genes have been discovered in animals, causing anomalies in the development of the rectum [5].
The clinical picture of the fistulaless form of atresia of the anus or rectum of various localization and extent is manifested mainly by symptoms of low intestinal obstruction. Lack of meconium passage, anxiety, refusal to eat and vomiting are the most characteristic symptoms that appear 1-2 days after the birth of the child.
Often rectal atresia is combined with fistulas in the genitourinary system or on the skin of the perineum. Clinical manifestations depend on the diameter and extent of the fistula. With high atresia, fistulas of narrow diameter predominate. Normal bowel movement through them is difficult, as a result of which symptoms of intestinal obstruction appear earlier. Fistulas that open onto the skin of the perineum in girls are often short and wide, ensuring normal bowel movements for a long time, which allows choosing the optimal timing for surgical treatment (at the age of 1.5–2 years). Until this age, it is necessary to ensure regular bowel movements with the help of a laxative diet, cleansing enemas, and bougienage of the fistula.
Congenital narrowings of the rectum and anus can be located in various parts of the rectum, including the anus. They can also be holes of different diameters. Clinical manifestations depend mainly on the degree of narrowing and can be characterized by various symptoms (from constipation to intestinal obstruction). The location and degree of narrowing of the rectum is determined by rectoscopy or proctography. With a small degree of narrowing, conservative treatment methods are used (laxative diet, bougienage, etc.). If conservative measures are ineffective, surgical treatment is performed.
Duplication of the rectum is an abnormal accessory formation that can take the form of a diverticulum, as well as a round or oblong cystic formation located intramural or adjacent to the rectum. Large doubling sizes can cause compression of the rectum with the appearance of symptoms of low intestinal obstruction. The main methods for diagnosing this defect are radiological and endoscopic methods. Treatment is surgical.
Ectopia of the anus is a displacement of the normally formed anus to a greater or lesser distance from its usual location. In this case, minor displacements have no clinical significance and may even remain unnoticed for a long time due to the absence of functional disorders. In case of functional disorders (fecal incontinence) in the case of ectopia of the anus, a differential diagnosis should be made with rectal atresia in combination with a fistula. Special studies (sphincter myography, etc.) are performed in the hospital [6, 7].
Sacrococcygeal teratoma (embryocytoma) - consists of the rudiments of various organs and immature tissues of the embryonic type, which causes rapid tumor growth. Upon examination, a painless spherical tumor is detected in the sacrococcygeal region, of heterogeneous consistency with cystic fluctuating areas and dense nodes. The teratoma can reach large sizes and hang down, pulling the anus, which causes constipation and difficulty urinating.
Constipation from an early age is the main symptom of Currarino syndrome , a rare hereditary syndrome of anorectal, sacral and presacral anomalies. The full form of the syndrome includes a combination of anorectal stenosis, presacral formation and sacral bone defect; in 80% it is diagnosed in the first 10 years of life [8].
Hirschsprung's disease is a developmental anomaly of the intramural nervous system of the colon, the incidence is 1:5000 children. The main clinical symptoms: from an early age, absence of independent stool, stool loss, absence of feces in the rectum during digital examination; after a cleansing enema, fecal fragments of small diameter are detected. As a rule, by 3 months of life, Hirschsprung's disease is diagnosed in 40% of children, by one year - in 61%, and by 4 years - in 82% [9].
Anomalies of intestinal development are the causes of constipation in 5% of children [9]. Practice shows that chronic constipation in these cases develops gradually, becomes more severe as the child grows, and reflects decompensation of intestinal function.
Regardless of whether an anomaly in the development of the colon is diagnosed or the doctor only assumes its presence, it is necessary to carry out all therapeutic measures aimed at simultaneously normalizing intestinal motility and restoring the impaired act of defecation.
In the vast majority of cases, the cause of chronic constipation is intentional or subconscious retention of stool (this statement does not apply only to children in the first months of life).
The development of chronic constipation is preceded by an episode of acute stool retention. Due to various reasons, feces become denser and decrease in volume, their evacuation from the rectum is reduced and is accompanied by great effort. Irritation of the anus, often accompanied by an anal fissure, causes painful bowel movements. If measures have not been taken to eliminate constipation, the child begins to consciously hold back feces, since defecation is associated with pain. Feces accumulate in the rectum, which leads to stretching of the rectal ampulla, the formation of a functional megarectum, incoordination of the pelvic floor muscles and, as a result, persistent disruption of the act of defecation.
The child cries during the act of defecation, rests his feet or body, squeezes his buttocks, and makes great efforts to free himself from feces. A bright blush may cover the child's face, so often great efforts during the act of defecation are misinterpreted by parents.
The etiology of acute constipation may vary depending on the age and developmental period of the child.
Conservative treatment
At any stage of the disease, treatment begins with therapeutic methods. Only in the absence of results is the question of indications for surgical intervention decided.
Dietary recommendations
The nature of nutrition is important in therapy. To do this, parents need to remember some rules. It is good for your baby to drink a lot of water, preferably slightly acidified with lemon juice. The liquid allows you to soften the stool. Any carbonated drinks or kvass are strictly prohibited. They help stool stick together into lumps.
Mineral waters with released gas and in a warm state work well. It is necessary to choose those that contain sulfate salts. The doctor will tell you how much water to drink for a particular patient. Feeding is done in small portions, at least six times a day. It is necessary to prepare dishes only boiled, steamed. Anything that is crusty, fried, spicy, or smoked is prohibited.
Avoid foods that make it difficult for food to pass through the intestines:
- cereals (rice, semolina, millet);
- flour products (pasta, fresh baked goods, cakes, cookies);
- meat dishes and animal fats (strengthen fermentation processes, “get stuck” in the intestines, and are poorly digested);
- sweets (sweets, chocolate);
- strong tea, cocoa, coffee.
You can feed your baby:
- boiled fish and soups made from it;
- cottage cheese;
- kefir, yogurt;
- boiled buckwheat porridge;
- vegetable dishes (vegetarian soup, solyanka, salads);
- Vegetable oils (olive, sunflower, linseed) are used for dressing.
The addition of bran is recommended. Vegetables and fruits that contain a lot of fiber are healthy. It helps loosen stools (boiled carrots and beets, pumpkin, apples, plums, prunes, dried apricots, apricots). They are used in salads, juices, baked in the oven for an afternoon snack, or prepared as a decoction or compote. For sweets, you can use a little honey and marmalade (contains pectin). It is not recommended to add to the diet: bananas, pears, grapes.
Drug treatment
Due to the disruption of the production of its own vitamins in the intestines, the child is shown vitamin complexes, including vitamins C, A, E, group B, D. They will help prevent the development of anemia and decreased immunity.
The doctor determines whether the little patient needs antispasmodics, because the pain is caused not by spasm, but by stretching and atony. Uncontrolled use of No-shpa and Drotaverine only worsens the situation. It is very important to restore the intestinal flora, so repeated courses of probiotics such as Bifidumbacterin, Lactobacterin, and dairy products with intestinal bacteria are prescribed.
Laxatives are prescribed by the doctor in minimal doses if diet does not help
The following are used in the treatment of children: Duphalac, Mucofalk, Duspatalin, Festal. The drugs have the ability to increase the tone of the intestinal wall, thin the stool, and enhance muscle motility.
Physiotherapy methods
Effective for physiotherapeutic treatment:
- electrical stimulation of the intestine;
- laser exposure;
- acupuncture;
- electrophoresis with tonic substances.
A very cautious attitude has developed towards colon hydrotherapy (intestinal lavage with mineral waters and herbal decoctions). They try not to prescribe it even to adult patients due to the large number of complications.
Enemas
The administration of water or saline solution with an enema has a local irritant effect on the rectum. The urge to defecate is reflexively caused. The volume of water for an enema is determined by the age of the child. The baby is placed on his right side, the buttock is raised and an enema tip lubricated with Vaseline is inserted.
The solution should not differ in temperature from the body. Too hot or cold is painful for the child. After administration, you need to squeeze your buttocks and sit or carry the baby in your arms for 10–15 minutes. Then plant it in a pot.
Massage
The only contraindication to massage is the presence of blood in the stool and an unclear source of bleeding. Breasts need daily massage of the back and abdomen to strengthen the muscles. In the position on the stomach, spiral movements are made with two fingers along the spinal area from the lower back to the tailbone. Thus, it is possible to stimulate the urge to defecate.
The abdomen is massaged in a clockwise circular motion. The massage needs to be enjoyable for the child. Shouting and sudden pressure should not be allowed. The procedure is always started by stroking and rubbing the skin. Then begin soft, slow pressing movements. In reverse order, finish by tapping the phalanges of the fingers. The entire procedure takes 20 minutes.
It is recommended to massage daily in the morning before feeding.
Physiotherapy
Indicated for older children. It is better to take your child to group classes at the clinic. Here they look at each other and learn the exercises faster. To stimulate bowel function:
- run;
- jumping in place;
- movements that strengthen the abdominal muscles;
- spinning a hoop.
Jumping rope promotes intestinal motility
Folk remedies
Recommendations of traditional medicine help in complex conservative effects. The possibility of use should be discussed with your pediatrician, since there may be contraindications at different ages.
Among herbal remedies it is proposed to use:
- celandine syrup - the same amount of celandine herb and sugar, after mixing, is tied in a gauze knot and placed in whey to infuse for 2 weeks;
- vegetable oil (preferably flaxseed or sunflower) - given a teaspoon before meals, it is necessary to provide for preliminary sterilization by boiling in a bottle in a water bath;
- the combination of buckthorn and prunes in a decoction improves the taste, and is useful for children as a compote after lunch;
- A water infusion (1:30) is prepared from flax seeds for an hour, filtered and drunk on an empty stomach, you can grind it in a coffee grinder and give the child ½ teaspoon in powder form;
- Wheat sprouts should be added to salads and porridge;
- Cabbage juice is prepared fresh; treatment is recommended for 2 weeks.
Treatment
Treatment of dolichosigma is a very complex process and includes two main directions: therapeutic (conservative) treatment and surgery.
First, conservative methods are used (medicines, massage, diet, physical therapy, etc.). Surgery is performed solely as a last resort.
Traditional medicine methods are often added to traditional means of therapy, but they complement and do not cancel the above methods of treatment.
Conservative treatment
Diet
To achieve effectiveness from treatment, the digestion process should be carried out. There are certain rules for choosing products and their consumption:
- The child should drink up to 3 liters of fluid per day. Kvass and carbonated drinks should be avoided, as such liquids cause constipation. They help strengthen and compact stool in the intestines. Water with lemon has a beneficial effect on the functioning of the gastrointestinal tract. Lemon oxidizes the environment, as a result of which feces liquefy and easily exit the body.
- Cereals: wheat, rice, buckwheat, semolina - should be removed from the diet.
- The consumption of flour products (pasta, confectionery, baked goods) has a negative effect on the healing process. Therefore, they should be removed from the diet.
- Meat and animal fats are contraindicated.
- Instead of forbidden strong tea and coffee, it is recommended to give your child at least 200 ml of low-fat kefir daily.
- It is allowed to give the child chocolate. But its consumption is not recommended to be combined with other foods, and it is also forbidden to eat it less than an hour before or after a meal. If you eat chocolate at the same time as other foods, constipation will occur, which will further worsen the child’s condition.
- You should not give your child solid food; all hard foods must be thoroughly steamed.
- The child should be fed in small portions 4 to 5 times a day.
Drug treatment
When the diet does not produce results, it is necessary to give the child pharmaceutical drugs. Before taking them, you should first consult with a specialist, as complications may arise, and an overdose will lead to the development of side effects: intestinal irritation and increased intestinal motility.
Laxatives
These drugs give results at the initial stage of pathology development. They are effective at the early stage of dolichosigma development. The appointment is carried out in strict accordance with medical indications and the age of the child.
Glycelax
The glycerin-based drug is available in the form of suppositories for rectal administration. It has a beneficial effect on intestinal motility and softens fecal matter. Can be used from birth. The best time to use is in the morning.
Bisacodyl
The drug in the form of rectal suppositories is allowed to be administered to children from two years of age. The medicine has an irritating effect on the intestinal walls, thereby normalizing its motility.
Guttalax
Allowed for children over 4 years old. Produced in the form of tablets and drops. The laxative effect of the drug is based on several mechanisms of action; as a result, the time interval between bowel movements decreases, the stool softens and leaves the body without difficulty.
Probiotics
An imbalance in flora often accompanies constipation. The quantitative and species composition of microflora changes. This has a negative effect on the condition, possibly worsening constipation, which leads to even greater inflammation. An imbalance leads to the growth of pathogenic flora. The free space in the intestines is occupied by a fungus, resulting in the development of candidiasis. Inflammatory and infectious processes move to other organs. Often intestinal dysbiosis is accompanied by an imbalance of the microflora of the genitourinary and respiratory systems. Long-term disruption reduces immunity, and the development of autoimmune pathologies is possible.
To normalize microbiocenosis, it is necessary to take probiotics. The appointment is carried out in strict accordance with the regimen prescribed by the doctor. Treatment should be completed only after consultation with specialists. Recommended products: bifidum, lactobacterin, yoghurt with bacterial starters.
Vitamins
Due to dietary restrictions, the child may lack vitamins and elements, as a result of which the immune system will be weakened. Vitamins B6, B12, C and E are very important for a child’s body.
They help improve food processing and facilitate the process of natural bowel movement.
Enema
An enema is performed only when diet and laxatives have failed to relieve constipation. For enema, pure water, herbal decoctions, and saline solutions are used. Excessive use of an enema entails a decrease in defecation reflexes, possibly the disappearance of the urge to empty the bowel or the development of fecal incontinence. Also, the result of long-term use of an enema is irritation of the intestinal walls, and this leads to the development of irritable bowel syndrome, colitis.
Massage and physical therapy
Massage and exercise are carried out to relieve constipation. A well-done massage stimulates the motor activity of the intestine and promotes the movement of fecal matter throughout the organ. A daily fifteen-minute exercise session will lead to gradual tightening of muscles, normalization of digestion, and quick elimination of problems with stool.
Surgery
The main indication for surgery is the failure of conservative treatment. It is performed subject to the progression of the disease, prolonged absence of stool, and increasing symptoms of intoxication. Many additional loops, bends and twists of the intestine are another mandatory indication. The main method is excision of part of the sigmoid colon.
Surgery
Indications are the child’s lack of results from the diet, medications, massage, addiction to enemas, and pronounced signs of intoxication. The operation is performed under general anesthesia. The surgeon cuts off unnecessary loops of the sigmoid colon and stitches the lower and upper ends.
If obstruction is suspected, the child is operated on according to vital indications. The doctor should examine the entire intestine for tissue viability. Twisting of moving loops can compress and disrupt the nutrition of the intestinal wall, leading to necrosis. Then, in addition to the sigmoid area, other sections have to be removed.
What complications does untreated dolichosigma lead to?
If you are not careful about the signs of illness, the child may experience:
- retardation in physical development, exhaustion;
- anemia;
- pustular rashes on the skin;
- fecal stones that can cause intestinal obstruction;
- chronic poisoning by wastes - fecal intoxication.
A frivolous attitude towards the course of pregnancy, constipation of the newborn baby, and lack of proper attentive care on the part of adults contribute to the development of dolichosigma in the child and serious consequences. Treatment in an advanced stage, refusal of timely examination lead to the need for surgical treatment. The earlier a child’s disease is detected, the greater the guarantee of its complete cure.
Diagnostics
When examining a child with dolichosigma, the doctor notes a lack of body weight, pale skin, and retarded physical development. Palpation of the abdomen reveals intestinal loops filled with feces. Rectal examination reveals an empty rectum. Instrumental diagnostic methods:
- irrigography;
- MSCT (multilayer computed tomography) of the intestine;
- electromyography;
- barium passage radiography;
- sphincterometry;
- rectosigmoidoscopy;
- Ultrasound of the abdominal cavity;
- Ultrasonography of the large intestine.