In the summer, when most parents try to send their children on vacation to warmer climes, the risk of getting an intestinal infection increases significantly. It is very common to hear at a pediatric appointment a request to make a list of medications that may be useful if the child gets sick while on vacation away from home, and of course, medications for the treatment of intestinal disorders are at the top of this list.
In this article, we decided to compose a small instruction for parents with children going on vacation, as they used to say: “at the request of the workers.”
Causes
There are 2 causes of intestinal infection in people, and both of them are a consequence of the penetration of harmful microorganisms into the body. In the first case, the disease is caused by intestinal viruses. There are about 10 groups of them. The most famous and common among them are enterovirus, adenovirus and rotavirus intestinal infections. Infants are very susceptible to rotavirus, or as it is popularly called “intestinal flu”. The second causative agent of intestinal infection in young children is bacteria. Bacterial infection is much better known under the names: coli infection; dysbacteriosis; salmonellosis and others. Infection with intestinal infections occurs through the fecal-oral route, that is, through the mouth. And the mediators can be dirty hands, unwashed fruits, non-compliance with hygiene standards. You can't keep an eye on your child here. In general, children under the age of seven are most susceptible to intestinal infections. After all, children's immunity to pathogenic bacteria and viruses is very weak compared to adults. This is especially true for newborns.
Intestinal infection in children, prevention
We will not spend much time describing the routes of infection. In this case, the main route of infection is certainly the entry of the pathogen directly through the mouth into the human body, or with unwashed hands, or through contaminated food and hygiene items. Children most often become infected with rotavirus infection. This happens because until the age of 3, most children are especially susceptible to rotavirus, and in hot climates, where we all try to get to in the summer, rotavirus lives everywhere, even in refrigerators. This does not mean that you cannot contract any other intestinal infection. Diarrhea, for example, can be caused by the so-called “travelers' disease”, the cause of which is no longer a virus, but a bacterium - E. coli, which lives in the specific region you are visiting and enters the body usually with water, which is all local they drink, and nothing bad happens to them for this, since they all have a strong immunity to this stick, but you and I don’t have this immunity, so we are friends with the toilet for a couple of days.
But you can still protect yourself from traveler's illness: wash your hands before eating and drink only bottled water. But protecting yourself from rotavirus is much more difficult, since it can end up anywhere, including, unfortunately, getting directly into the food on the table.
Since you and I know that rotavirus loves children most of all, a logical question arises: is there a vaccine against it? Yes, I have. The vaccine against rotavirus is called Rotatec. If you immediately after the birth of your baby begin to plan some long trips a year or two after his birth, then of course it would be better to immediately take care of vaccinating your baby against rotavirus.
Attention! to get vaccinated against rotavirus after a year, since the instructions for the drug imply a three-time vaccination regimen in the period from 2 to 8 months. The vaccine is administered orally, it is a live vaccine, and it may have contraindications, so before getting vaccinated against rotavirus, you should consult with a pediatric immunologist.
Symptoms
The first signs of rotavirus can appear within 24 hours after infection, but more often they appear 3-5 days after the virus enters the body. The symptoms of the disease are acute and obvious: the temperature rises sharply and strongly (up to 38-390); vomiting occurs several times a day (up to 3-6); the general condition of the child is lethargic, apathetic; frequent watery diarrhea begins with a pronounced light yellow tint and an unpleasant sour odor; redness of the mucous membranes of the eyes and throat occurs. Along with the manifestations of the disease described when rotavirus occurs, in the case of enterovirus infection the following may be observed: fever, convulsions, muscle and head pain. Signs of a bacterial infection are similar to the manifestations of a viral infection - these are the same elevated temperature, but up to 37-380C, vomiting (with viral infections it is always present, and with bacterial infections - in half the cases), diarrhea (if watery yellow diarrhea is observed with viral infections, sometimes with foam, then with a bacterial infection it necessarily contains inclusions of mucus, has a greenish tint, sometimes small blood clots are found in the stool - in an advanced form.
Rotavirus in a newborn
Infants become dehydrated very quickly, so the general course of rotavirus infection is usually quite severe. The recommendations also include drinking plenty of fluids. Breastfed babies get most of their fluid from breast milk. Therefore, it is important to put your baby to the breast frequently. Mom can notice that the child himself began to ask for the breast more often during illness - this is not hunger, but the need to replenish water losses.
It is also important to put mixed-fed babies to the breast more often, and to switch formula-fed babies to a low-lactose or lactose-free formula for the period of illness and recovery. You can order this mixture with fast delivery throughout Moscow and all of Russia in our online store.
Diagnostics
Bacteriological cultures of stool and, in some cases, vomit. This is the leading diagnostic method. Determines which microbe is causing the intestinal infection. To analyze the stool, a smear is taken from the child’s anus (it is also called a “VD smear” or “intestinal group smear”). The resulting material is sown on special nutrient media. After a few days (usually 5-7 days), colonies of bacteria grow, which can be examined under a microscope and tested using various methods. Unfortunately, it is not always possible to detect the pathogen. Blood tests to determine the increase in antibody titer to any pathogen. Determine the reaction of the immune system to a suspected infection. If there is an increase in antibodies to a specific pathogen, then we can say with confidence that the person is sick (or has been sick). This method is rarely used in practice. Express diagnostics: enzyme-linked immunosorbent assay (ELISA) and other laboratory tests. They are mainly used in hospital settings. Scatological analysis of stool. In it you can see the degree of digestion of food, blood, mucus and protozoa (amoeba and lamblia).
Diagnosis of rotavirus infection
Rotavirus infection is diagnosed by the presence of typical signs of the disease: fever, vomiting and diarrhea.
It is important to know that you can get sick from rotavirus infection in an atypical form. In this case, the disease progresses more easily. Only 1-2 signs may be expressed or not expressed at all. In this case, the person releases the virus and is infectious.
There are various stool tests that can detect the virus. However, treatment must begin immediately when the first symptoms appear, without waiting for test results.
Treatment
The biggest mistake parents make is the desire to stop seemingly unwanted manifestations of the disease. But in the first hours this is strictly forbidden, because vomiting and diarrhea are a protective reaction of the body, which is trying to cleanse itself of toxins. Stopping cleaning will lead to even greater intoxication. It is important to constantly replenish the loss of fluid and mineral salts (potassium, sodium, calcium). You should ensure that your child drinks plenty of fluids. It is necessary to drink with special solutions. No juices or dairy! For acute intestinal infections, a saline solution is used: 1 teaspoon of table salt, 4 teaspoons of sugar and 1.5 teaspoons of baking soda per liter of water. You need to give your child 2-3 teaspoons of water every 3-5 minutes. If a child vomits, then it is necessary to drink in small portions so as not to provoke repeated attacks. It is best to give the child a warm drink (at body temperature): in this case, the absorption of liquid from the intestinal walls into the blood will occur as quickly as possible, which is now extremely important. Feeding a child who has an intestinal infection is extremely undesirable and one might even say that it is impossible. Hunger is the second cure in such a situation. The gastrointestinal tract is now affected, it has no time to digest food. When the child feels better and he still demands to eat (only in this case!), stick to the diet: light rice soup, oatmeal or rice porridge, low-fat cottage cheese or kefir, mashed potatoes with water. You can also make a puree from baked apples, steamed carrots, pumpkin, zucchini, grated apples and bananas. It is forbidden to give your child foods that cause gas or contain coarse fiber. And no sweets, fatty, spicy, salty or smoked foods. Portions should be small: it is better to feed the child often, but in fractions. Monitor your child's hygiene very carefully. Be especially careful about hand washing after using the toilet and before eating. Only a doctor can judge the advisability of prescribing antibiotics and other medications. Therefore, you should not self-medicate.
This is new material, but Tiger Cub once wrote on this topic - “Rotavirus infection.
(Please note that the information contained in an earlier article may not be entirely current.) Now we invite you to familiarize yourself with the modern view of this problem.The article was prepared by a team of pediatricians at the Tiger Cub Children's Clinic
What is rotavirus and what are its symptoms? How dangerous is rotavirus infection and how to help a sick child, how effective is vaccination against this virus?
About the disease.
Rotavirus infection is one of the types of acute intestinal infection. It is caused by a special type of virus - rotavirus, popularly this disease is often called “stomach flu”.
From the first lines we are clear - rotavirus has nothing to do with the influenza virus and any specific strains of it. Any flu can multiply and exist only on the mucous membranes of the respiratory tract. With rotavirus, everything is different; it “lives” in the small intestine, and therefore calling it the flu as a whole is not very correct.
For the first time, rotavirus (under a microscope resembling a wheel, and therefore called “rota” - wheel (lat.)) was discovered almost half a century ago by Australian researchers. According to existing medical statistics, 98% of children under the age of 3 have already had this disease at least once. It is transmitted the virus is transmitted through contact - fecal-oral, this is popularly called “dirty hands disease”.
A baby can become infected from a sick person through toys, door handles, dishes, and household items. The virus is extremely contagious. Although specific immunity to rotavirus is developed, it is almost irrelevant, since this virus has a lot of strains and varieties - science already knows at least 9 of them, and mutations are still ongoing.
All varieties of this virus are quite resistant to low temperatures, exposure to sunlight and air. Rotavirus survives for quite a long time in spring and sea water.
The incubation period is the time that passes after the virus enters the body until the acute stage of the disease begins. This period of time varies for different children.
The virus accumulates and replicates, usually within 3-7 days. The disease itself lasts about 2-3 days, and the body takes at least another 5 days to recover after recovery.
A child is contagious all the time from the moment of infection until the end of the recovery period. Even if the baby already feels well, viable microparticles of the virus still continue to be released in the stool. It is for this reason that we strongly do not recommend sending him to kindergarten or school immediately after the child feels better. This is very likely to lead to mass infection in the children's group.
The likelihood of infection with rotavirus does not in any way depend on the cleanliness of the family. Even if a mother washes and vacuums the entire house several times a day, if she forces her child to wash his hands with soap every hour, carefully monitors the quality of every product that ends up on the table, and does not allow him to drink water of dubious origin - all this hardly reduces the risk of getting sick. rotavirus.
The virus most often attacks children aged 6 months to 2 years. In general, children from birth to 5 years of age are at risk. In a newborn, this disease occurs somewhat less frequently, since the first six months after birth the child is favorably influenced by the mother’s “innate” immunity, which usually lasts for a maximum of six months. Then the baby becomes more vulnerable.
The World Health Organization provides the following figures: every year on our planet, about 25 million children become infected with rotavirus. Most recover fairly quickly and on their own. 2 million children end up in hospitals, which leads to the death of about 500 thousand children annually, but not from the rotavirus infection itself, but from the severe complications that occur during its course.
Symptoms.
The following main symptoms can be identified: • Diarrhea. • Vomiting • Abdominal pain. • Increased flatulence. • Increased body temperature. • Lethargy, pale skin. • Lack of appetite.
According to our statistics, the vast majority of cases of unexplained diarrhea in children under three years of age are a manifestation of rotavirus infection. In other words, if a child ate everything he usually ate and has no signs of food poisoning, then stool upset in 99% of cases indicates an attack by this particular type of virus.
Rotavirus is tropic (has a special affinity) for pancreatic cells. At the height of the disease, its function is impaired. At first, the stool becomes oily (poorly washed off), has a smooth shiny surface and a clayey consistency. Then transient lactase intolerance develops (the intestinal villi are affected), and the stool becomes increasingly watery. An imperative urge to defecate is characteristic.
It seems that everything that “enters” the child immediately “comes out” without stopping. For this reason, it is quite simple to distinguish rotavirus infection from poisoning (a disorder caused by bacteria) - the main clue for parents should be the consistency of the stool. Pasty diarrhea often occurs with food poisoning. Diarrhea “with water” is a viral diarrhea, and, as a rule, there are no other options.
With viral diarrhea, stool has a grayish color and a very strong, unpleasant odor. By 2-3 days, the contents of the pot acquire a clayey consistency and a yellowish-gray color. The sour smell persists.
Rotavirus infection is characterized by a sudden acute onset - with fever and vomiting. Sometimes vomit may have a specific odor of acetone; a child’s breath may smell similarly. At the next stage, enteritis and gastroenteritis, diarrhea develops (up to 10-12 trips to the toilet per day). Minor respiratory symptoms may appear - runny nose, sore throat, pain when swallowing, cough.
About treatment.
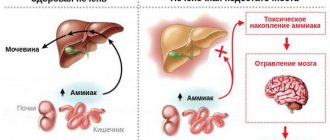
Diarrhea due to rotavirus infection usually goes away within 2-3 days, but poses a rather serious danger of dehydration. Almost all deaths that occurred with this disease became possible precisely because of critical loss of fluid and severe dehydration. The younger the child, the faster he develops dehydration, the more dangerous the rotavirus is for him. The infection is most severe in infants.
A serious complication caused by rotavirus in severe dehydration is pneumonia. Many cases of dehydration are complicated by serious disorders of the nervous system. Rotavirus and dehydration are especially dangerous for underweight children.
The main thing that parents should learn to do is not even to determine the origin of the baby’s diarrhea, but to be able to quickly assess whether the child has signs of dehydration. We strongly recommend that you consult a doctor in any case of diarrhea in a young child. But you can’t just sit still and do nothing; you have to watch carefully.
If a baby's tongue becomes dry, he begins to cry without tears, does not pee for more than 6 hours and practically does not sweat - this is a good reason to urgently call an ambulance. If the baby begins to lose consciousness, his eyes “sink”, his facial features “sharpen”, and he develops a high temperature - these are extremely dangerous symptoms, they indicate severe dehydration. Doctors' help is required immediately.
If dehydration begins, a child who cannot drink enough fluids to restore balance in the body needs intravenous water. This is what the inpatient treatment will be based on.
If there are no signs of dehydration, parents can easily cope with rotavirus intestinal infection on their own. And here the main therapy will be to prevent the onset of dehydration. For this, the child needs to be given water. The more often the better. The drink should not be cold or hot, but only at room temperature, since this is the liquid that is absorbed most quickly in the small intestine. If the baby refuses to drink in sips, he needs to be fed with a teaspoon more often, but he must drink. For rotavirus infection, we recommend taking special medications that should be in the medicine cabinet of every family with children - oral rehydration products (for example, Regidron, Humana Electrolyte). If there is no such medicine, it is not possible to buy it, then we recommend using a recipe approved by the World Health Organization: take 2 tablespoons of sugar, a spoonful of salt and a spoonful of soda per liter of water. The parents’ task is to give their child this saline solution at any cost. If this does not work, it is better to immediately call an ambulance.
First aid.
In general, the algorithm for reasonable parental actions in case of childhood diarrhea should always look like this: • Drink plenty of warm drinks. Frequent and fractional. Plain water and saline solution. If a child pees every 3 hours, it means he is consuming enough fluid to prevent dehydration. If you can’t get someone to drink even with a disposable syringe without a needle, call an ambulance. • Place a small child on his side so that in the event of an attack of vomiting he does not choke on the vomit. • Antipyretics - only if the temperature is above 38.5. • Monitor the child's condition and prevent dehydration. At the first symptoms of dehydration, call an ambulance. • Do not feed. If he really asks, give liquid porridge or puree in small quantities.
Before the doctor arrives, leave a diaper with stool or keep a sample of the contents of the potty to show the doctor. This way, the doctor will be able to diagnose the disease faster, and the likelihood of an error will be reduced (rotavirus, for example, is very similar to cholera in its initial stages).
It's a big mistake to give your child antibiotics. The disease is of viral origin, and antibacterial drugs are completely powerless against viruses. Treating a child with viral diarrhea with them is a real parental crime, since it not only does not bring benefit, but also increases the likelihood of complications.
Another mistake that can cost parents dearly is the unauthorized prescription of antidiarrheal drugs (for example, Enterofuril). With rotavirus, viral particles (more precisely, their microparticles) are released in the stool. Therefore, stopping diarrhea means prolonging the disease, leaving viral particles in the small intestine, where they will continue to destroy beneficial cells for some time. There is no need to fight diarrhea; it is a defense mechanism of the body.
Another misconception is the effectiveness of antiviral drugs for intestinal infections. Although some doctors continue to prescribe antiviral drugs for rotavirus infection, we strongly do not recommend taking them for an intestinal infection. Of course, whether or not to take the above tablets or syrups is up to you. But you should know that there are no antiviral drugs in nature with clinically proven effectiveness. Moreover, the effectiveness of these drugs against a specific pathogen, rotavirus, has not been proven. It is also worth abandoning homeopathic remedies (Anaferon, Oscillococinum). With them, with their effectiveness and proven action, everything is even worse (yes, this is possible), and the purchase of such drugs will only be an extra burden on the family budget and can cause additional stress for the baby.
Vaccination.
Many countries have already included vaccination against rotavirus intestinal infection in their mandatory National Vaccination Schedules. In Russia there is no such mandatory practice yet. Vaccination against rotavirus, according to Western experts, helps reduce morbidity by 80% and reduces the risk of death by 45%. That is, infection remains possible, but the course of the disease will be milder.
In the children's clinic "TIGER" the RotaTek vaccine is used to prevent rotavirus infection. The vaccine is taken orally (as drops in the mouth). RotaTek contains small quantities of live rotavirus artificially weakened in laboratory conditions. In most cases, the vaccine does not cause allergic reactions or side effects, it is quite easily tolerated even by the smallest patients.
The recommended vaccination period is from 1.5 months to six months. It is not advisable for older children to be vaccinated. A total of 3 doses of the vaccine are administered. Standard recommended RotaTek vaccination schedule: 2 - 3 - 4.5 months.
Naturally, vaccination will not be given to a child who is currently ill; vaccination against rotavirus is also contraindicated for children with congenital malformations of the gastrointestinal tract. As before any vaccination, before vaccination with RotaTek you need to see a pediatrician with test results (clinical blood test and general urine test). No special preparation is required for rotavirus vaccination.
Advice for parents.
During the acute phase of the disease, you should not feed the child unless he asks for food himself.
You should adhere to a strict diet not only during treatment, but also for some time after recovery: completely exclude from the menu whole milk and dairy products, sweet fruits, baked goods, meat, as well as fatty and fried foods. It is healthy to eat porridge with water, vegetable soups, white bread crackers, and oven-baked apples. Feeding should be frequent and in small portions. Very young children with rotavirus infection are not denied breast milk, no dietary restrictions are imposed, but they are ensured that they drink plenty of fluids. Breast milk itself contains antiviral components provided by nature, which will help the baby in the recovery process.
Occasionally, when rotavirus infection is severe, an infant may develop intolerance or partial intolerance to breast milk due to enzyme deficiency. In this case, you should reduce the number of breastfeedings and temporarily add lactose-free infant formula to the baby’s diet (until complete recovery).
A child sick with rotavirus should not necessarily be put to bed. If he has a high temperature, then bed rest is necessary. In all other cases, he should lead a normal lifestyle - play, walk.
Of course, you should stay away from the yard playground so as not to spread the rotavirus to other children, but a walk in an uncrowded park or square will be beneficial.
The most effective prevention of rotavirus is vaccination. Only then comes hygiene - you must wash your hands, of course with soap, thoroughly wash vegetables and fruits, and monitor the quality of the water your child drinks.
But once again, in fairness, we note that no hygienic tricks can guarantee a low probability of infection. Therefore, both in developed and civilized countries and in third world countries, the incidence of rotavirus is at an equally high level. If you are going to travel to the sea with a small child, we strongly recommend the rotavirus vaccine. Recently, this intestinal infection has become quite widespread at resorts, where children become infected with water. Every year, Rospotrebnadzor specialists “signal” about the unfavorable situation due to this disease on the Black Sea coast of the Caucasus, in Crimea and on the coasts of Bulgaria.
Prognosis and prevention
Timely detection of the first signs of intestinal infection in a child and properly selected treatment can ensure a complete recovery. Usually immunity to such diseases is unstable. With the development of a severe form of the disease, complications may appear, including acute renal or heart failure, pulmonary edema and other dangerous conditions. For this reason, parents are advised not to select medications for treatment themselves, but to immediately consult a doctor.
To prevent bacterial and viral intestinal infections, the following sanitary and hygienic standards must be observed:
- teach your child the rules of personal hygiene from an early age;
- properly store and heat process food;
- Parents should always wash their hands after washing and swaddling the baby;
- Make sure that the water you drink is clean (filtration and boiling will help);
- disinfection of toys and utensils in kindergartens, which can be sources of infection;
- When breastfeeding, the mother should shower daily and change her underwear regularly to keep the mammary glands clean;
- If a child eats from bottles and sucks on a pacifier, then they also need to be regularly treated with specially designed products. This way, viruses and bacteria that cause acute intestinal infections will not penetrate the gastrointestinal tract through the objects used.
The remaining children in the family or in the child care facility where the sick child was located should be examined, and their well-being should be monitored for at least 7 days.
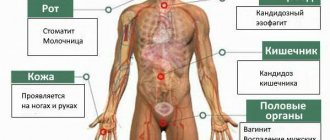
What organs are affected by intestinal infections?
In children and adults, intestinal infections can affect various organs of the digestive system:
- Stomach - when its mucous membrane becomes inflamed, gastritis develops. It is accompanied by nausea, vomiting and pain in the area above the navel.
- Stomach and small intestine - gastroenteritis develops, which is characterized by loose, watery stools containing undigested food debris. Patients complain of pain around the navel.
- Stomach, small and large intestines - gastroenterocolitis develops. In this case, the patient feels pain not only in the abdomen, but also during bowel movements. The stool is loose, frequent, sometimes mixed with blood.
- Small intestine - when the mucous membrane of this section of the gastrointestinal tract becomes inflamed, enteritis develops. This infectious disease is not characterized by nausea, vomiting and abdominal pain. The stool is frequent and watery.
- Large intestine - when this part of the digestive system is damaged, colitis develops. The disease is characterized by pain localized in the lower abdomen. Acute diarrhea develops, sometimes mixed with blood and mucus.
- Large and small intestines - inflammation of the mucous membrane, which causes severe abdominal pain, loose stools, and a frequent urge to empty the bowel.
Classification
In medicine, acute intestinal infections are divided depending on the type of pathogen that caused them. Therefore, there are two large groups of diseases - bacterial and viral. In turn, each group has subgroups:
- Viral – this includes rotavirus infection, adenovirus (intestinal flu) and enterovirus infection.
- Bacterial - This includes dysentery (shigellosis) and botulism, which occurs due to the consumption of home-canned foods.