Duration
15 minutes
The duration of the study itself is from 1 to 10 minutes.
After this, a decryption is carried out, and the person is immediately given the photographs. The patient is scheduled for 30 minutes. Soreness
No pain
The study is non-invasive and painless.
Preparation
Preparation required
Follow a diet 2-3 days before the test.
12 hours before the x-ray you need to stop eating solid food, and 2 hours before the examination you need to cleanse your intestines (about the same as when preparing for gastroscopy). Rehabilitation
Not required
After the study, patients feel well.
Work ability
Saved
After X-rays, patients feel well and their ability to work is not impaired.
Sports activities
No restrictions
The study is non-invasive, no restrictions.
Abdominal X-ray is a non-invasive, painless examination method. The procedure is performed without the use of a contrast agent and is 100% safe! X-ray allows you to see the overall picture of the condition of the abdominal organs.
If you are worried about bloating, pain, constipation, nausea, consult a specialist. Perhaps the cause will be determined using an x-ray.
In addition to radiography, there is also such a study as fluoroscopy. Fluoroscopy is a real-time study of organs, which allows you to evaluate their functioning over time. The main difference between radiography and fluoroscopy is that such observation is not carried out; one-time photographs are taken. However, in some cases, when the radiologist sees clear images with brightening, contrast is not needed.
Our patients can undergo contrast X-rays of the abdominal organs and radiography. It is determined individually what kind of research needs to be carried out.
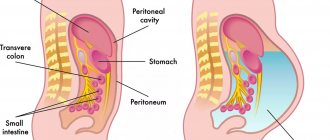
Traditional abdominal examination includes transillumination and serial plain radiography. Due to the anatomical features of the digestive system, it is impossible to recognize the disease only from photographs taken in standard projections.
The duration of the study itself is from 1 to 10 minutes. After this, a decryption is carried out, and the person is immediately given the photographs. The radiologist writes a description for the doctor who referred the patient for an x-ray.
A survey X-ray of the abdominal cavity allows you to determine what is causing the patient’s poor health: excess gases, fluid in the abdominal cavity (bleeding), foreign objects. In the images, the doctor can see damage that has arisen for various reasons: inflammation, injury, etc.
Introduction
With the widespread implementation of colorectal cancer screening, colonoscopy is becoming one of the frequently performed endoscopic procedures. Colon perforation is one of the most serious complications of both diagnostic (DC) and therapeutic colonoscopy (LC). The frequency of this event varies from 0.016 to 0.8% in DC and from 0.02 to 8% in LC [1]. Previously, the vast majority of perforations required surgical treatment, but recently endoscopic methods for closing perforations using various types of clips have been successfully introduced into practice [2, 3]. Despite a number of reports on successful endoscopic closure of colon wall defects made at conferences at various levels, the real situation with perforations during colonoscopies in routine clinical practice in Russia remains unknown.
The purpose of the study is to analyze the causes, methods and results of treatment of colon perforation in DC and LC.
Causes
Causes of rupture or perforation:
- Inflammation of the middle ear (otitis media). A middle ear infection often causes fluid to accumulate in the middle ear. The pressure of this fluid can cause perforation.
- Barotrauma. Barotrauma is stress on the eardrum when the air pressure in the middle ear and the air pressure outside are out of balance. If the pressure is severe, the tympanic membrane may rupture. Barotrauma is most often caused by changes in air pressure associated with air travel. Other events that can cause sudden changes in pressure—and possibly rupture of the membrane—include scuba diving and a direct blow to the ear, such as a car airbag.
- Loud noises or explosions (acoustic trauma). A loud sound, such as an explosion or gunshot, or a blast—essentially an overwhelming sound wave—can cause the membrane to rupture.
- Foreign objects. Small objects such as a cotton swab or hairpin can puncture or rupture the tympanic membrane.
- Severe head injury. Severe trauma, such as a skull fracture, can dislocate or damage the structures of the middle and inner ear, including the eardrum.
Material and methods
To assess the incidence, methods and results of treatment of colon perforation caused by colonoscopy, a multicenter (9 medical institutions) retrospective study was conducted. All participants were sent identical table layouts for entering data characterizing the perforation and the method of its elimination; in addition, doctors were asked to comment in free form on the cause of the event. We analyzed the gender, age of the patients, the type of intervention during which the perforation developed, its location, size (mm), time of occurrence (immediate/delayed) and diagnosis, method and result of correction, as well as the length of service of the doctor who performed the intervention. Perforation was understood as visible through damage to the organ wall and/or target symptom, and/or free gas in the abdominal cavity with the clinical picture of perforation of a hollow organ. Perforation in DC was defined as an event that occurred during colonoscopy without any intervention, excluding forceps biopsy.
Perforation that occurred immediately or within 3 hours after colonoscopy was considered immediate, and perforation that occurred more than 3 hours after the procedure was considered delayed. The location of the perforation was assessed according to anatomical landmarks.
Exclusion criteria from the study were localization of perforation in the rectum or intentional perforation (full-thickness removal), or pain without visible perforation and/or target sign, and/or free gas in the abdominal cavity, or lack of basic data on the case.
Participants reported 56 cases of perforation, and the final analysis included 50 cases (DC 11 of 14, LC 39 of 42) in 50 patients (38 women, 12 men). The time period for which data was provided ranged from 1.5 to 11 years.
Statistical processing was carried out using Microsoft Excel spreadsheets, using Fisher's exact test and one-way analysis of variance (one-way Anova), the level of statistical significance was considered p<0.05.
What happens if you leave the problem without a solution?
Tooth perforation is a fairly serious problem leading to various dental problems. If a cavity forms in the root canal, root apex or tooth walls, immediate treatment is required. Lack of therapy can lead to the following consequences:
- the development of a granuloma - a cavity filled with pus, which can grow, gradually affecting nearby tissues;
- if left untreated, granuloma can develop into a cyst;
- if the tooth structure is severely damaged, root fracture may occur, which is difficult to detect without x-rays;
- development of inflammatory processes with severe painful symptoms that complicate chewing food;
- Aggravated tissue inflammation can affect speech, causing speech defects.
The perforation options don't end there. Various inflammatory and destructive processes can develop, which lead not only to dental diseases, but also to their loss.
results
The average age of patients who had colon perforation was 62.9±11.9 years. The majority (76%) of patients were female; the rates of female and male patients in the groups of perforations that occurred with DC and LC did not differ statistically significantly. Data on the frequency of perforations over a long period of time are presented by only two clinics (Irkutsk Diagnostic). It amounted to 10 (0.009%) cases per 111,102 studies in DC and 5 (0.03%) per 15,612 studies in LC.
Perforation with DC occurred more often in older people than with LC (72.4±6.1 compared with 60.1±11.8 years p=0.001). The average size of the perforation hole was larger in DC than in LC (21.6 ± 13.3 and 8.6 ± 10.1 mm, respectively, p = 0.001). Direct perforation occurred in 45 cases, and 44 of them were diagnosed within 0-3 hours after the study. Delayed perforation occurred in 5 (100%) cases after LC.
The cause of the majority of perforations - 21 (64%) cases - in the LC group was removal of formations using the EMR method (endoscopic mucosal resection; endoscopic resection of the mucosa); the ESD method (endoscopic submucosal dissection; endoscopic dissection in the submucosal layer) caused LC in 11 cases. In addition, perforations occurred during polypectomy - 2 and balloon dilatation/stenting - 5. Perforation in the rectosigmoid region occurred in 12 cases (of which with DC - in 7 cases), in the left half of the colon - in 19 (DC - 4, more 2 cases were excluded from the final analysis due to the lack of complete data), in the right half - in 19 (DC - 0, one case of cecal barotrauma was not included in the study due to incomplete data). Perforation in the left half of the colon, including the rectosigmoid region, occurred more often in DC than in LC (p<0.00001).
In DC, colonic diverticulosis and severe adhesions are cited as the main causes of patient-related perforation; and excessive force during endoscopy, as a physician-related reason. Characteristics of colon perforation and treatment results are shown in the table .
Characteristics of colon perforations during colonoscopy and methods of their treatment
| Index | Perforation during colonoscopy, n=50 | p | |
| diagnostic colonoscopy, n=11 | therapeutic colonoscopy, n=39 | ||
| Average perforation hole size, mm | 21,6±13,3 | 8,6±10,1 | 0,001 |
| Localization | — | — | <0,00001 |
| Left half of the colon, n (of which the rectosigmoid section) | 11 (7) | 20 (5) | — |
| Right half of the colon, n | — | 19 | — |
| Time of occurrence | — | — | N.S. |
| Direct | 11 | 34 | — |
| Deferred | — | 5 | — |
| Method of treatment | — | — | 0,0003 |
| Clipping, n (of which successful) | 1 (0) | 28 (27) | — |
| Surgical | 10 | 11 | — |
Note. NS - not statistically significant.
Clips passed through the endoscope channel to close the perforation were used in 29 cases (58% of all and 69.4% of direct perforations). The number of clips used was reported in 23 cases - on average 5.9±2.2 (4-11) pieces. The application of clips turned out to be ineffective in 2 (6.9%) cases, and therefore a second stage of surgical treatment with the formation of a stoma was required. A typical case of endoscopic treatment of perforation is presented in the figure .
Perforation of the colon during mucosal resection.
a — epithelial formation in the form of a superficially spreading tumor; b — after submucosal lifting, the formation is captured by a loop; c — wound after removal of a formation with a perforation hole; d — the wound is sutured with clips.
Surgical treatment was chosen in 21 cases (DC - 10, LC - 11), including 100% of delayed perforations, in 8 (38.1%) cases - with the formation of a stoma. There were no deaths. Delayed perforation (p=0.0096) and perforation with DC (p=0.0003) are statistically significantly associated with the risk of surgical intervention. On average, the size of the defect in patients who required surgical treatment was larger than the size of the perforation repaired with clips (16.2 ± 15.8 and 8.03 ± 6.7 mm, respectively, p = 0.015). Physician experience (more or less than 10 years) did not have a statistically significant effect on the likelihood of endoscopic treatment of colon perforation.
Contraindications for carrying out
X-ray is a safe examination that has no absolute contraindications and allows you to quickly obtain clear images of internal organs. However, radiation diagnostics is contraindicated for pregnant women and children under 15 years of age.
Our studies are carried out using the latest generation Italray Clinodigit Compact digital X-ray machine. High-definition pictures are obtained in literally 10-15 minutes. Digital detectors are 5 times more sensitive than photographic film.
Discussion
Perforation is one of the complications of DC and LC. The frequency of its occurrence in our study (DC - 0.009% and LC - 0.03%) was lower than according to the literature (from 0.016 to 0.8% for DC and from 0.02 to 8% for LC [1]) , however, it should be noted that these results are presented only by two institutions that are centers of expertise in performing colonoscopy.
If we consider all the presented cases of perforation in DC (14 observations), it can be noted that the vast majority of them were localized in the rectosigmoid region (50%) and sigmoid colon (43%), only in one case in the right half of the colon (cecum) , which corresponds to the literature data on a higher risk of perforation with DC in the left half of the colon [4–6].
Perforation in DC in this study occurred in elderly people (mean age 72.4±6.1 years), and female patients predominated (90.1%). Diverticular disease and severe adhesions were identified as the main causes of this event. When conducting multifactor analysis, B. Bielawska et al. also noted that older age and female gender are risk factors for perforation during colonoscopy [7]. According to other researchers, risk factors for perforation included age over 75, female gender, diverticular disease and a history of abdominal surgery [8].
LC perforations in this study occurred during EMR, ESD, stenting, and balloon dilatation. The European Society of Gastrointestinal Endoscopy (ESGE) and the International Association of Emergency Surgery classify colonoscopy as a procedure with an increased risk of colon perforation [1, 9].
According to the data obtained, the size of the perforation hole was statistically significantly larger in the DC group than in the LC group (21.6 ± 13.3 mm compared to 8.6 ± 10.1 mm), which practically coincides with the results published by D. Yang and al. (19.3±12.8 and 5.8±2.9 mm, respectively) [10].
The vast majority of perforations in this work were diagnosed within 3 hours, while according to the literature, only 68% of perforations are detected on the day of the procedure [11], and the average delay time for diagnosing this event is 0.36 days after DC and 1.5 days after LK [4].
An attempt at endoscopic closure of perforation was made in 70% of cases of its occurrence with direct LC and 9% with DC, which is lower than according to a number of foreign authors (82-84% with LC and 31-60% with DC) [2, 12 , 13].
However, according to the results of a systematic review published in 2022, including 19 studies (744 cases of colon perforation), endoscopic clipping was used in only 15% of cases [14]. ESGE recommends using endoscope clips to close small perforations (up to 20 mm) and over-the-scope clips (OTSC) to close larger perforations [9]. In this study, only the first type of clip was used, which reflects both the small average size of the perforation hole and the high cost and low availability of OTSC type clips.
The need for surgical treatment after an attempt at endoscopic clipping occurs, according to the literature, in 14.7% of cases [15], which is 2 times higher than according to our data. This fact, combined with a lower proportion of attempts at endoscopic closure of the perforation, can be explained by a more conservative choice between the indications for endoscopic and surgical treatment by the physicians participating in the study.
Delayed perforation and perforation during diagnostic endoscopy are associated with the need for surgical treatment, which is consistent with literature data [2, 9].
A stoma is created in approximately 30% of patients who require surgical treatment for perforation. In the literature, the incidence of ostomy varies widely, reaching 59.7% [16].
Complications
The eardrum has two main functions:
- Auditory. When sound waves strike, the eardrum vibrates—the first step by which structures in the middle and inner ear translate sound waves into nerve impulses.
- Protective. The eardrum also has a barrier function, protecting the middle ear from water, bacteria, and other foreign substances.
Complications may occur as the membrane heals or if it fails to heal.
Possible complications:
- Hearing loss. Typically, hearing loss is temporary, lasting only until the tear or hole heals. The size and location of the tear can affect the degree of hearing loss.
- Inflammation of the middle ear (otitis media). A perforated eardrum allows bacteria to enter the ear. If a perforated eardrum does not heal or repair itself, you may be vulnerable to ongoing (chronic) infections that can cause permanent hearing loss.
- Middle ear formations (cholesteatoma). Cholesteatoma is a growth in the middle ear consisting of skin cells and other substances. All accumulated impurities and dead skin cells in the ear canals usually come out with earwax. If the membrane is ruptured, skin cells can pass into the middle ear and form a cholesteatoma. Cholesteatoma provides a favorable environment for bacteria and contains proteins that can damage the ossicles of the middle ear.
Reviews of doctors providing the service – Tooth perforation
I would like to express my gratitude to the dentist Elena Nikolaevna Kiseleva and her assistant Svetlana - they are real specialists and at the same time sensitive, not burnt out by years of practice.
Thanks to them, I have been coming back here for many years. Thanks to the management for such doctors! Read full review Svetlana Nikolaevna
13.08.2021
I am very grateful to Evgeniy Borisovich Antiukhin for removing my three eights. Especially considering that the lower tooth was not the simplest (it was located in an embrace with a nerve). The removal took place in 2 stages, one tooth under local anesthesia, two under general anesthesia. I had no idea that wisdom teeth could be... Read full review
Sofia
28.12.2020
Signs of tooth perforation
The appearance of a pathological hole during dental treatment is indicated by the appearance of pain symptoms of a very intense nature. If the doctor touches the probe to a fresh wound, the patient has a specific feeling as if it is resting on the gum with a pointed end. Symptoms of old tooth perforations:
- pain when biting;
- a fistula in the gum that closes and opens again;
- swelling of the transitional fold (during exacerbation of periodontitis).