A case of gastric cancer detected by ultrasound examination
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Introduction
Gastric cancer occupies one of the first places among malignant tumors of other localizations and in almost half of the cases is detected at late incurable stages [1]. Clinical manifestations of stomach cancer are not always specific. The generally accepted methods for diagnosing this disease are X-ray and endoscopic. However, in recent years, work has appeared indicating the possibility of using other methods, in particular, ultrasound examination of the stomach, including for the detection of stomach cancer [2-6].
Observation
A 62-year-old patient was followed by an endocrinologist for 6 years for a mild form of diabetes mellitus. She had no complaints, was treated as an outpatient, and periodically took Diabeton. Over the course of several months, she began to notice general weakness, then pain in the epigastrium, right hypochondrium, bitterness in the mouth, belching, gradually worsened her appetite, and the patient lost about 3 kg in weight. On examination: average height, high nutrition, normal skin color, no swelling, subcutaneous lymph nodes are not palpable. The tongue is covered with a white coating. Heart sounds are moderately muffled and rhythmic. Pulse 72 beats/min. Blood pressure 110/70 mm Hg. Art. Blood tests showed sugar levels within normal limits, and urine tests showed no sugar. The abdomen is swollen, enlarged in volume, painful on palpation in the epigastrium and right hypochondrium. The liver and spleen are not palpable.
It was decided to begin examining the patient with an ultrasound (fasting) of the abdominal cavity, including examination of the liver, gallbladder and pancreas. Ultrasound signs of chronic cholecystitis, fatty infiltration of the liver, and chronic pancreatitis were noted.
Not satisfied with the results, the endocrinologist sent the patient for a repeat ultrasound of the abdominal cavity, as well as an examination of the spleen and kidneys, during which signs of chronic cholecystitis, diffuse changes in the liver, pancreas with signs of fatty infiltration were also noted. No changes were detected in the spleen and kidneys. However, free fluid was found in the abdominal cavity, which forced us to expand the scope of the ultrasound.
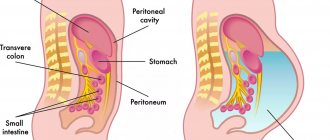
When examining the area of the projection of the stomach, a symptom of lesion of a hollow organ (HOA) was revealed, indicating thickening of the walls of the stomach (mainly the posterior one) and narrowing of its cavity in the area of the outlet section and body (Fig. 1). The maximum outer diameter of the affected segment of the stomach was 54.7; the maximum wall thickness is 28 and the length along the organ is 82 mm. During color Doppler examination, chaotically located small vessels of irregular shape were visible in the area of the thickened wall. After filling with fluid, the altered gastric wall was visible as a hypoechoic, irregular, rigid stripe. The layering of the wall is not pronounced, the outer contours of the stomach are uneven, unclear, in the body area along the posterior wall and along the lesser curvature are not visible, merging with the anterior surface of the pancreas. The stomach cavity in this place is narrowed, deformed, peristalsis was not traced. Given the intimate connection of the stomach to the pancreas, against the background of a fluid-filled stomach, the pancreas was studied in more detail. In the parenchyma of the gland, three hypoechoic, heterogeneous structures with uneven contours were identified, sizes: in the head area 6x9, body area 25x29 and tail area 19x23 mm. It was concluded that there were ultrasound signs of a gastric neoplasm with metastases and invasion into the pancreas; ascites and gastroscopy with biopsy is recommended.
Rice. 1.
Ultrasound of the stomach (fasting examination).
Echogram A.
Longitudinal section in the epigastrium to the left of the midline. Liver. Cross section of the stomach (symptom of damage to a hollow organ). A significant thickening of the walls of the stomach is visible, mainly the posterior one (the wall is uneven, indistinct, merges with the anterior surface of the pancreas).
Echogram B.
Oblique section in the epigastrium. Image of circularly thickened walls of the stomach in the place of their greatest thickening (damage to a hollow organ).
1 - thickened walls, 2 - narrowed stomach cavity.
During gastroscopy: little secretion was found in the stomach cavity, the folds were smoothed and swollen; The mucosa is pale brown in the body area, along the lesser curvature - lumpy, rigid, in places with an ulcerative necrotic coating. A biopsy was taken. The conclusion of the morphological study of the gastric biopsy was signet ring cell carcinoma. The patient was sent to the oncology clinic.
conclusions
- Complaints of patients with stomach cancer can be masked by manifestations of other diseases, in particular diabetes mellitus, chronic cholecystitis, chronic pancreatitis.
- The ultrasound method can be used to detect stomach cancer and clarify the extent of the process.
- It is advisable to include the stomach in the mandatory list of organs during an ultrasound examination of the abdominal cavity.
Literature
- Malignant neoplasms in Russia: statistics, scientific achievements, problems / V.I. Chissov, V.V. Starinsky and others // Kazan. honey. magazine. 2000. N 4. S. 241248.
- Lemeshko Z.A., Pimanov S.I. Ultrasound examination of the stomach: Clinical guide to ultrasound diagnostics; Ed. V.V.Mitkova. M.: Vidar, 1997. T. 4. P. 939.
- Lemeshko Z.A., Turok T.P., Panina N.I. Detection of gastric pathology using the ultrasound method in an outpatient setting // Proc. report 3rd Congress of the Russian Association of Ultrasound Diagnostics in Medicine. M., 1999. October 25-28. Topic 3. P.96.
- Ultrasound diagnosis of stomach cancer / L.M. Portnoy, T.B. Legostaeva, N.V. Yaurova, L.E. Gaganov // Ross. oncol. magazine. 1999. N 4. S. 22-29.
- Tukhbatullin M.G. Possibilities of ultrasound examination of the stomach // Kazan. medical journal 1996. N 3. S. 218-219.
- Fujino Y., Nagata Y., Ogino K., Watahiki H. Evaluation of endoscopic ultrasonography as an indicator for surgical treatment of gastric cancer // J. GastroenterolHepatol. 1999.Vol. 14(6). P.540-546.
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Treatment and prognosis
Surgical intervention is currently used as the main treatment method for patients with localized and locally advanced forms of GIST. For unresectable tumors, the presence of metastases, or recurrent GIST, treatment consists of prescribing tyrosine kinase inhibitors (imatinib) [17, 19]. According to various data, from 10% to 30% of GISTs have malignant potential. GISTs are usually classified according to the risk of malignancy: very low, low, moderate, high. The main prognostic factors for GIST, according to current international consensus, are the mitotic index (the number of mitoses in an area of 5 mm2 of tumor at 400 magnification), tumor size and location. Moreover, the risk of GIST metastasis increases depending on the size of the primary tumor, regardless of the mitotic index. It is also necessary to note the importance of the marker of proliferative activity Ki-67, the level of expression of which significantly increases with increasing risk of GIST aggressiveness, which is used to assess the degree of malignancy and prognosis. It is generally accepted that gastric GISTs, all other characteristics being equal, have a more favorable prognosis [18, 20, 21].
Determination of mutation types in different KIT
and PDGFR-α is also an important prognostic marker that allows us to judge both the clinical course of the disease and the expected response of the tumor to therapy with tyrosine kinase inhibitors [22].
According to a meta-analysis by L. Yan et al. [23] (20 studies, 3780 patients), progression-free survival of GIST was significantly worse in patients with KIT
than in patients with
KIT
(odds ratio [OR] 3.60, 95% confidence interval [CI ] 2.17–5.98, z=4.96, p<0.00001, heterogeneity
I
2=0%).
KIT
mutations were significantly more common in patients with larger (≥5 cm) GIST (OR 1.51, 95% CI 1.05–2.17, z=2.22, p=0.03, heterogeneity
I2
=0 %, p=0.97), as well as in patients with a higher (≥5/50 HPFs) mitotic index (OR 1.76, 95% CI 1.05–2.95, z=2.15, p= 0.03, heterogeneity
I
2 = 57%, p = 0.03).
Symptoms
Gastric atrophy has main signs and symptoms that are almost the same in all patients.
Among them:
- nausea;
- aching pain with an uncertain location, which noticeably intensifies after eating;
- copious amounts of saliva;
- frequent belching with a bitter, rotten taste;
- bloating and rumbling in the stomach;
- feeling of heaviness in the stomach;
- an unpleasant white coating on the tongue;
- stool instability, in which constipation is replaced by diarrhea;
- dystrophic syndrome;
- clinic of iron and vitamin D-, B12-, C-deficiency anemia - dizziness, fatigue, shortness of breath, weakness, brittle hair and nails, bleeding gums, pale skin, decreased visual acuity, seizures and pustular skin lesions.
Thickness standards
Despite a person’s age and gender, the thickness of the stomach wall is constant. If its size is 50-60 mm over the area of the entire digestive organ, then the compaction indicators are normal. If this figure increases in at least one of the areas, you should look for the causes of the pathology. The thickness of the organ wall does not vary according to various indicators, and an increase in its density above 0.6 cm indicates an abnormal compaction. If the thickening area is more than 3 cm long and the wall changes its relief, this indicates limited thickening. The organ is deformed, the volume decreases, thickening is present virtually throughout the stomach - this is a common compaction.
Fibrogastroduodenoscopy
This type of endoscopic examination is another one of the most popular. It allows the doctor to visually examine the walls of the stomach and identify possible pathologies. To carry out the procedure, a special device is used - a gastroscope. It consists of a tube with a diameter of 8-11 mm and a length of approximately 100 cm. The front tip is movable and can rotate 180 degrees. There is also a light and camera for easy inspection.
The probe is used not only for visual diagnosis, but also for biopsy. Microscopic forceps are inserted through the probe to help remove the material.
This procedure is performed if there is a suspicion that the thickening of the walls is associated with cancer. The advantage of fibrogastroduodenoscopy is that it is targeted, and only the area of interest to the specialist can be affected. The removed sample is sent for diagnostics, during which the exact cause of the pathology is determined.
Anatomy
The stomach in the human body is the primary organ of the digestive system. It is located between the esophagus and the small intestine, or rather the duodenum.
The organ consists of several parts:
- The cardinal section is the uppermost part. Here the transition from the esophagus to the stomach itself takes place.
- The more convex part is the arch or bottom.
- The continuation of the vault is the body of the stomach. It is divided into greater and lesser curvature.
- The final part is the antrum. Here the organ narrows, takes the form of a tube and passes into the duodenum.
Digestion processes take place in any part of the organ, therefore atrophy can form in different parts.
The wall of an organ consists of several layers or membranes. The most superficial is serous, the thickest, serving as a frame and protection for the organ from aggressive influences.
This is followed by the muscle layer, consisting of a number of muscle fibers involved in the processes of digestion and peristalsis
The submucosa serves as a transition to the innermost and most important wall - the mucosa
In the gastric mucosa there are a number of cells that synthesize and secrete various substances; parietal cells produce hydrochloric acid, which is involved in the chemical processing of the bolus.
Endocrine cells secrete the hormone gastrin, which is necessary for normal digestion. Additional elements synthesize mucus; it is a protective component of the mucous membrane from its own hydrochloric acid.
When there is little mucus, damaging self-digestion processes are launched. Chief cells produce the enzyme pepsin.
The gastric mucosa has a number of functions:
- Digestive: produces substances that facilitate all digestive processes.
- Secretory: participates in the release of secretory active compounds.
- Hematopoietic: produces vitamins and blood clotting factors.
Ultrasound diagnosis of thickening of the stomach walls
Wall thickening can also be detected using x-rays, but ultrasound has several advantages.
The examination allows you to study the organ in different projections, it is safe and does not have a harmful effect on the body. During the examination, the Doctor can see changes in each layer. On ultrasound, the wall looks like a thin line consisting of three layers - hyperechoic inside and hypoechoic on the sides. The mucous membrane has folds that smooth out when the sensor is pressed. Normally, movements (peristalsis) can also be observed.
An increase in thickness occurs due to any of the layers. Thus, with interstitial tumors, changes in the size of the submucosal or muscular layer in a certain area are often detected. An increase in the mucous layer occurs during inflammatory processes and hypertrophy. Also, benign (polyps) and malignant (adenocarcinoma) neoplasms often form in this layer. Doppler examination allows one to differentiate malignant neoplasms, which can detect increased blood flow in this area.
Thickening as a symptom of stomach inflammation
With the modern rhythm of life, constant stress and poor nutrition, a large part of the population suffers from digestive disorders.
In addition to the above factors, this disease is also affected by:
- frequent drinking;
- drug use;
- infection;
- taking painkillers from the group of non-steroidal anti-inflammatory drugs (NSAIDs);
- autoimmune infection.
In the latter case, inflammation often occurs against the background of other autoimmune diseases, for example, type I diabetes.
Inflammation is manifested by severe nausea, vomiting, aching pain and heaviness after eating. When these symptoms appear, immediate diagnosis and treatment are required. In the absence of therapy, the disease can provoke a number of complications, one of which is an increase in the walls of the organ, which increases the risk of cancer.