Peptic ulcer of the stomach and duodenum is a fairly common disease.
The nature of peptic ulcer disease is considered to be sufficiently studied, many medications have been developed and put into practice, which have indeed proven to be very effective. Peptic ulcer disease is now successfully treated with conservative methods. In recent decades, indications for surgical treatment (especially elective treatment) have sharply decreased. However, there are still situations where surgery cannot be avoided.
In addition to the pain and unpleasant symptoms that this disease causes the patient, in 15-25% it is accompanied by complications (bleeding, perforation or obstruction of food passage), which requires surgical measures.
All operations performed for stomach ulcers can be divided into:
- Emergency - mainly suturing a perforated ulcer and resection of the stomach in case of bleeding.
- Planned – gastric resection.
- Open method.
- Laparoscopic.
Indications for surgery for stomach ulcers
Perforation of an ulcer (the occurrence of a through defect in the wall of the stomach or duodenum).- Bleeding from an ulcer that cannot be stopped with hemostatic agents and endoscopic hemostasis.
- Cicatricial narrowing of the outlet of the stomach, making it difficult for food to pass through.
- Long-term non-healing ulcers suspicious for malignancy.
- Often recurrent (more than 3-4 times a year) ulcers (relative indication).
- Combination of an ulcer with diffuse gastric polyposis (relative indication).
The main operations that are currently performed for peptic ulcer disease are gastric resection and suturing of the perforation.
Some other types of operations (vagotomy, pyloroplasty, local excision of an ulcer, gastroenteroanastomosis without gastrectomy) are performed very rarely today, since their effectiveness is much lower than gastrectomy. Vagotomy is performed mainly for duodenal ulcers.
Causes
The reasons leading to the occurrence of ulcers on the mucous membrane of both the stomach and duodenum are:
- chronic stress,
- unhealthy diet
- smoking,
- consumption of “aggressive” drinks,
- the use of certain groups of medications (for example, painkillers from the NSAID group or hormones).
The role of the specific bacterium H.pylory in the occurrence of ulcerative defects on the mucous membrane of the stomach and duodenum is also widely discussed.
In general, the clinical picture and symptoms of duodenal ulcer are similar to those of the stomach.
Duodenal ulcers are usually located in the bulb and postbulbar region, on the anterior or posterior wall.
Types of ulcers
Based on the number of ulcerative lesions, single and multiple ulcers are distinguished. Depending on the size of the ulcerative defect:
- small ulcers (up to 0.5 cm in diameter);
- medium (0.6-1.9 cm in diameter) sizes;
- large (2.0 - 3.0 cm in diameter);
- giant (over 3.0 cm in diameter) ulcers.
Pain due to duodenal ulcer
Pain from duodenal ulcer is usually localized in the upper abdomen, can vary significantly in intensity (from moderate discomfort to sharp cutting pain), and is often associated with food intake.
Unlike stomach ulcers, duodenal ulcers are characterized by the development of “hungry” and night pain, which decrease with food intake, which can lead to weight gain (for example, this can explain nightly “trips” to the refrigerator).
Pain can radiate to the back, to the spine, which sometimes leads to incorrect interpretation and treatment, for example, for osteochondrosis.
Features of patient selection for surgical treatment of peptic ulcer
In emergency situations (perforation, bleeding), the question is about the life and death of the patient, and here there is usually no doubt about the choice of treatment.
When it comes to planned resection, the decision must be very balanced and thoughtful. If there is even the slightest opportunity to manage the patient conservatively, this opportunity should be used. The operation can get rid of the ulcer forever, but it adds other problems (quite often manifestations occur, designated as operated stomach syndrome).
The patient should be informed as much as possible about both the consequences of the operation and the consequences of not taking surgical measures.
Operations for perforation of an ulcer
A perforated stomach ulcer is an emergency condition. If the operation is delayed, it can lead to the development of peritonitis and the death of the patient.
Usually, when an ulcer is perforated, it is sutured and the abdominal cavity is sanitized, and less often, an emergency gastrectomy is performed.
Preparation for emergency surgery is minimal. The intervention itself is performed under general anesthesia. Access – upper median laparotomy. A revision (examination) of the abdominal cavity is performed, a perforation hole is located (it is usually several millimeters), and it is sutured with absorbable thread. Sometimes, for better reliability, a large oil seal is sewn to the hole.
Next, the stomach contents and effusion that have entered there are sucked out from the abdominal cavity, and the cavity is washed with antiseptics. Drainage is being improved. A tube is inserted into the stomach to suction out the contents. The wound is sutured layer by layer.
The patient is on parenteral nutrition for several days. Broad-spectrum antibiotics are mandatory.
If the course is favorable, the drainage is removed on the 3-4th day, the sutures are usually removed on the 7th day. Working capacity is restored after 1-2 months.
When peritonitis develops, repeated surgery is sometimes required.
Suturing a perforated ulcer is not a radical operation, it is only an emergency measure to save life. The ulcer may recur. In the future, it is necessary to undergo regular examinations for early detection of exacerbations and the appointment of conservative therapy.
Gastric resection
The most common operation for peptic ulcer disease is gastric resection. It can be carried out both as an emergency (for bleeding or perforation) and as a planned procedure (chronic long-term non-healing, often recurrent ulcers).
From 1/3 (for ulcers located close to the outlet) to 3/4 of the stomach is removed. If malignancy is suspected, subtotal and total resection (gastrectomy) may be prescribed.
gastrectomy
Resection of part of the stomach is preferable, rather than simply excision of the area with the ulcer, because:
- Removing only the ulcer will not solve the problem as a whole, the peptic ulcer will recur, and you will have to do a second operation.
- Local excision of the ulcer followed by suturing of the stomach wall can subsequently cause severe cicatricial deformation with impaired passage of food, which will also necessitate a repeat operation.
- The gastric resection operation is universal, it has been well studied and developed.
Preparing for surgery
To clarify the diagnosis, the patient must undergo:
- Gastroendoscopy with biopsy from the ulcer.
- X-ray contrast examination of the stomach to clarify the function of evacuation.
- Ultrasound or CT scan of the abdominal cavity to clarify the condition of neighboring organs.
In the presence of concomitant chronic diseases, consultation with relevant specialists is necessary, compensation for vital systems (cardiovascular, respiratory, blood sugar levels, etc.). In the presence of foci of chronic infection, their sanitation is necessary (teeth, tonsils, paranasal sinuses).
At least 10-14 days before surgery, the following are prescribed:
- Blood and urine tests.
- Coagulogram.
- Determination of blood group.
- ECG.
- Biochemical analysis.
- Blood testing for the presence of antibodies to chronic infectious diseases (HIV, hepatitis, syphilis).
- Examination by a therapist.
- Gynecologist examination for women.
Progress of the operation
The operation is performed under general endotracheal anesthesia.
An incision is made along the midline from the sternum to the navel. The surgeon mobilizes the stomach and ligates the vessels leading to the part to be removed. At the border of removal, the stomach is stitched either with an atraumatic suture or with a stapler. The duodenum is stitched in the same way.
Part of the stomach is cut off and removed. Next, an anastomosis is performed (most often “side to side”) between the remaining part of the stomach and the duodenum, less often – the small intestine. A drain (tube) is left in the abdominal cavity, and a tube is left in the stomach. The wound is sutured.
You cannot eat or drink for several days after the operation (intravenous infusion of solutions and liquids is being established). The drainage is usually removed on the 3rd day. The stitches are removed on 7-8 days.
Painkillers and antibacterial drugs are prescribed. You can get up in a day.
Diagnostics
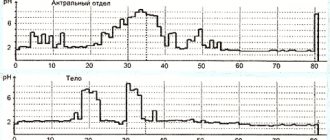
In the general blood test, leukocytosis is observed, a neutrophilic shift of the leukocyte formula to the left.
Plain x-ray of the abdomen reveals free gas in the abdominal cavity (pneumoperitoneum). In the absence of pneumoperitoneum on a plain radiograph of the abdomen, after it has been emptied, 500–700 ml of air is injected into the stomach using a probe, which partially passes through the perforation into the free abdominal cavity and is found under the diaphragm.
Also, a perforated ulcer is detected using gastroscopy.
Laparoscopic surgery for gastric ulcers
Laparoscopic surgery is increasingly replacing open surgical interventions. Using this technique, it is now possible to perform literally any operation, including gastric ulcer surgery (suturing a perforation of the stomach wall, as well as gastric resection).
Laparoscopic surgery is performed using special equipment, not through a large incision in the abdominal wall, but through several small punctures (for inserting a laparoscope and trocars for accessing instruments).
In this case, the stages of the operation are the same as with open access. Laparoscopy also requires general anesthesia. Stitching of the walls of the stomach and duodenum during resection is carried out either with a regular suture (which lengthens the operation) or with stitching devices (like a stapler), which is more expensive. After cutting off part of the stomach, it is removed. To do this, one of the punctures in the abdominal wall expands to 3-4 cm.
The advantages of such operations are obvious:
- Less traumatic.
- No large incisions – no post-operative pain.
- Less risk of suppuration.
- Blood loss is several times less (coagulators are used to stop bleeding from crossed vessels).
- Cosmetic effect - no scars.
- You can get up a few hours after the operation; there is a minimum period of hospital stay.
- Short rehabilitation period.
- Less risk of postoperative adhesions and hernias.
- The ability to repeatedly enlarge the surgical field with a laparoscope allows you to perform the operation as delicately as possible, as well as examine the condition of neighboring organs.
The main difficulties associated with laparoscopic operations:
- Laparoscopic surgery takes longer than usual.
- Expensive equipment and consumables are used, which increases the cost of the operation.
- A highly qualified surgeon and sufficient experience are required.
- Sometimes during the operation it is possible to switch to open access.
- Not all peptic ulcer conditions can be operated on using this technique (for example, laparoscopic surgery will not be prescribed for large perforation sizes, as well as for the development of peritonitis)
The danger of a perforated ulcer and how to treat it.
The incidence of perforated ulcers in the Republic of Belarus is almost twice as high as in Europe.
What is the reason for this? Mainly due to poor motivation of the patients themselves for treatment. About 60% of patients diagnosed with peptic ulcer and perforated ulcer do not follow doctors’ recommendations for treatment both at the “therapeutic stage” and after the perforation episode.
Patients often come to the operating table and find out that they are suffering from a peptic ulcer only at the moment of perforation of the ulcer. Perforated ulcers often develop in young and middle-aged people, with males predominating among patients. Recently, perforated ulcers have increasingly begun to develop in women (the peak incidence occurs in the age group of 50-60 years).
Why exactly these categories of people turned out to be so vulnerable? Young men are generally less likely to see a doctor. Consequently, they do not receive adequate drug therapy for peptic ulcer disease, which would help avoid complications such as bleeding, penetration, and perforation of the ulcer. Aggressive advertising of over-the-counter medications “against heartburn and stomach discomfort” plays a negative role in this. As a rule, these are inexpensive, but far from the most effective drugs needed for the treatment of peptic ulcers. As a result, a significant proportion of young men with peptic ulcer disease do not see a doctor until the ulcer perforates. Regarding the reasons for the increase in the number of women suffering from perforated ulcers, there is a connection with the transition of a woman from one hormonal status to another.
Once perforation of the gastric ulcer is confirmed, urgent surgical treatment is required, otherwise the prognosis is poor.
Causes of perforated ulcers: non-compliance with the prescribed diet, constant stress, mental and nervous strain, physical activity incommensurate with capabilities, malfunctions of the immune system.
With a perforated ulcer, severe weakness and intense pain in the abdominal area, chills, nausea occur almost instantly, vomiting often occurs, and dry mouth appears. The condition worsens, which is expressed by paleness of the skin. Against this background, the heart rate increases and then decreases. Subsequently, a drop in pressure is observed, which often provokes loss of consciousness. The initial period of ulcer perforation can last from 3 to 6 hours. During the latent period, which can last up to 12 hours, the patient’s condition stabilizes somewhat. Blood pressure and heartbeat are normalized, and the skin tone improves. But at the same time, dry mouth and shallow breathing remain. Painful sensations subside and become less intense. The danger at this point is that, as their condition improves, patients may refuse to undergo surgery. This increases the risk of serious complications, including death.
It is important to remember that if perforation of a stomach ulcer is confirmed, you cannot hesitate, you should immediately agree to the operation.
If surgical intervention is not performed, then purulent peritonitis develops. Unbearable pain returns, constant nausea and severe vomiting occur, abdominal bloating and fever occur. In this case, the likelihood of a positive prognosis is significantly reduced.
Since signs of perforation of an ulcer are always obvious, if they appear, you should urgently call an ambulance . Emergency care for a perforated ulcer at home is to ensure complete rest. It is advisable to persuade the person to go to bed and it is better not to do anything until the ambulance specialists arrive. To minimize pain, you can try to take the most comfortable position. As a rule, the pain is slightly reduced if you lie on your side and press your legs to your stomach. It is advisable to try to convince the person not to change position too often. It is strictly forbidden to consume any food or water. This is due to the fact that food and liquid immediately enters the abdominal cavity. Before the ambulance arrives, you should regularly monitor your pulse and blood pressure, and also observe the person’s appearance. A drop in blood pressure, increased heart rate, and pale skin are symptoms of an approaching painful shock.
Diagnostics. A general blood test, radiography of the abdominal organs, ultrasound of the abdominal cavity, and an endoscopic examination are urgently performed to determine the exact location of the defect and assess the degree of damage.
Treatment . It is impossible to cure a perforated stomach ulcer using any conservative methods. Surgical treatment is the only way to eliminate a perforated gastric ulcer . There are three main approaches: suturing the ulcer, excision of the ulcer, and gastric resection. In most patients, the perforation is closed by suturing the defect. Excision of a perforated gastric ulcer is performed only in every tenth patient. Indications for gastric resection arise in the case of a complicated course of a peptic ulcer (callous and penetrating ulcers, multiple ulcers, stenosis of the gastric outlet), suspicion of a malignant process, repeated perforation of a gastric ulcer, or a large size of the perforation. In approximately 10% of patients, minimally invasive – laparoscopic surgical techniques are used. The use of laparoscopic operations can significantly reduce the incidence of postoperative complications.
Surgery is only the initial stage of treating a perforated ulcer. A positive prognosis after surgical treatment depends entirely on proper rehabilitation.
Diet. Its goal is to reduce the load on the digestive organ and restore its motility. Only by following a strict diet for at least six months can a relapse be prevented. On days 2-3 after surgery, you are allowed to drink small amounts of mineral water, weak tea or sweet fruit jelly. On the 4th-5th day, ground boiled cereal soups, as well as rosehip decoction, are introduced into the diet. Fish soufflé and steamed cutlets made from dietary meats are allowed in small quantities. On day 10, a small amount of mashed potatoes is included in the diet. From now on, boiled pumpkin and soft carrots should be gradually introduced into the menu. Salt should be avoided.
Dairy products can be introduced into the diet after 2 weeks, but it is necessary to monitor the body’s reaction. If you feel well, you can regularly take low-fat cottage cheese and natural yogurt. Bread should first appear in the diet no earlier than in a month.
During the postoperative period, it is recommended to eat up to 6-7 times a day, but in very small portions. Dishes in the diet should be puree or semi-liquid. Food should be steamed or boiled.
The prognosis depends on various factors. The main factors are age, the presence of concomitant pathologies, the patient’s condition, and the duration of the disease.
Of course, a perforated ulcer is a very serious complication that quite often takes you by surprise. But you should never despair, because modern treatment methods allow you to fully recover after a complex operation. To do this, you need to show willpower, follow all the doctor’s recommendations and a strict diet throughout a long period of rehabilitation.
Surgeon 1 x/o
Nikolaeva O.S.
After operation
For 1-2 days after surgery, food and liquid intake is excluded. Usually on the second day you can drink a glass of water, on the third day - about 300 ml of liquid food (fruit drinks, broths, rosehip decoction, raw egg, slightly sweetened jelly). Gradually, the diet expands to semi-liquid (slimy porridges, soups, vegetable purees), and then to thick boiled food without seasonings with a minimum salt content (steamed meatballs, fish, cereal porridges, low-fat dairy products, stewed or baked vegetables).
Any canned food, smoked meats, seasonings, roughage, hot dishes, alcohol, baked goods, carbonated drinks are prohibited. The volume of food per meal should not exceed 150-200 ml.
A strict restrictive diet with 5-6 meals a day is recommended for 1-1.5 months.
During open operations, it is recommended to limit heavy physical activity and wear a postoperative bandage for 1.5–2 months. After laparoscopic operations this period is shorter.
Causes of perforated stomach ulcer
People suffering from chronic peptic ulcer disease, as well as those who have suffered an acute form of the disease, are at risk of developing a perforation defect.
Perforation can be initiated by:
- Inflammation that occurs around the main focus of mucosal damage;
- Overeating (the stomach cannot cope with a large amount of food);
- Increased acidity of gastric juice (leads to an aggressive environment);
- Excessive consumption of foods seasoned with spices and alcohol;
- Sudden physical exertion;
Modern research indicates that the causative agent of peptic ulcer disease is the bacterium Helicobacter pylori (which has initially aggressive strains). Almost 50% of all humanity is infected with it. But contamination is not the only cause of peptic ulcer disease. Any violation of the body’s protective functions activates the pathogenic influence of microorganisms.
Factors that increase the risk of peptic ulcer disease:
- Suppressed immune system;
- Impaired quality or duration of sleep, night shift work;
- Prolonged stress;
- Taking certain medications. Long-term treatment with non-steroidal anti-inflammatory drugs (including aspirin) is not allowed; even short-term anticoagulants (warfarin, heparin), corticosteroids (prednisolone), and some chemotherapy drugs can have a pathogenic effect;
- Smoking (has an indirect effect on increasing the content of hydrochloric acid and disrupting microcirculation in the mucous membranes);
- Excessive alcohol consumption (leads to direct damage to the mucous membranes);
- Violation of food intake and nutritional quality. Too low or high temperature of food, foods with high fat content, smoked foods, etc., dry food unnecessarily load the stomach and provoke the occurrence of diseases;
- Hereditary factors;
- The presence of other pathologies of the gastrointestinal tract (for example, gastritis);
Complications after surgery
Early complications
- Bleeding.
- Suppuration of the wound.
- Peritonitis.
- Failure of seams.
- Thrombophlebitis.
- Pulmonary embolism.
- Paralytic intestinal obstruction.
Late complications
- Recurrence of ulcers. An ulcer can occur both in the remaining part of the stomach and (more often) in the area of the anastomosis.
- Dumping syndrome. This is a symptom complex of autonomic reactions in response to the rapid entry of undigested food into the small intestine after gastric resection. Manifested by severe weakness, palpitations, sweating, dizziness after eating.
- Adductor loop syndrome. It manifests itself as bursting pain in the right hypochondrium after eating, bloating, nausea and vomiting with bile.
- Iron deficiency and B-12 deficiency anemia.
- Intestinal dyspepsia syndrome (bloating, rumbling in the abdomen, frequent loose stools or constipation).
- Development of secondary pancreatitis.
- Adhesive disease.
- Postoperative hernias.
3. Symptoms and diagnosis
In the clinic of a perforated ulcer, there are three stages, the names of which speak for themselves:
- abdominal shock;
- imaginary well-being;
- purulent diffuse peritonitis.
Each of these phases takes, on average, about six hours.
The most characteristic symptom of the initial stage is a sharp and very intense pain, often radiating to neighboring areas or the back. It is this type of pain syndrome that the well-known expression “dagger pain” refers to, and it, like a real sudden stab in the stomach, is accompanied by a powerful psycho-emotional shock. In most cases, the patient takes a forced fetal or other similar position, tries not to move (or rather, cannot), breathes shallowly and often, his eyes “sink,” his face acquires an earthy-pale hue and a characteristic motionless, suffering-panic expression. Bradycardia and a decrease in blood pressure, caused by a reflex reaction to damage to intra-abdominal tissues and receptors by the gushing acid of the gastric juice, are also quite typical.
Subsequently, the color of the facial skin, breathing, heart rate and blood pressure are somewhat normalized. At this stage, as a rule, precious time is lost: often the patient has to literally beg consent for a life-saving operation. Subjective improvement is not without reason called “imaginary well-being” - in fact, this is already a fatal risk, since in the next phase (repeated vomiting, dehydration, sharp worsening of the general condition, tachycardia and tachypnea, significant bloating) to provide assistance, even the most urgent and qualified, in many cases it is already too late.
An experienced doctor confidently assumes the diagnosis even with an external examination, palpation and percussion: there are a number of fairly informative criteria regarding muscle status, zones and nature of pain, etc.
However, much depends on the specific location of the perforation and the dynamics of symptoms. In some cases, the situation develops according to an atypical scenario; in particular, the clinical picture may resemble symptoms of acute appendicitis, myocardial infarction, pulmonary pathology - in other words, differentiation and clarification are required. In addition to the physical examination, laboratory tests, an X-ray examination (usually with a contrast agent, the detection of which outside the stomach and duodenum is one hundred percent proof of perforation), and urgent fibrogastroduodenoscopy are prescribed. In some diagnostically difficult cases, laparoscopic examination is used.
About our clinic Chistye Prudy metro station Medintercom page!
Prevention of complications
The occurrence of early complications depends mainly on the quality of the operation performed and the skill of the surgeon. On the part of the patient, all that is required is strict adherence to the recommended diet, physical activity, etc.
To prevent late complications and make your life as easy as possible after surgery, you should follow the following recommendations:
- Be regularly examined by a gastroenterologist.
- Compliance with a fractional diet regimen for 6-8 months until the body adapts to new digestive conditions.
- Taking enzyme preparations in courses or “on demand”.
- Taking dietary supplements with iron and vitamins.
- Limiting heavy lifting for 2 months to prevent hernia.
According to reviews from patients who have undergone gastrectomy, the most difficult thing after surgery is to give up your eating habits and adapt to a new diet. But this must be done. Adaptation of the body to digestion in conditions of a shortened stomach lasts from 6 to 8 months, in some patients – up to a year.
Usually there is discomfort after eating and weight loss. It is very important to survive this period without any complications. After some time, the body adapts to the new condition, the symptoms of the operated stomach become less pronounced, and weight is restored. A person lives a normal, full life without part of the stomach.
Providing assistance with a strangulated hernia
Urgent Care:
- emergency hospitalization in the surgical department, transportation on a stretcher;
- it is strictly forbidden to reduce the hernia, use analgesics, baths, or heat;
- Hospitalization is also indicated if by the time of examination the strangulated hernia has been reduced;
- patients with an irreducible hernia and pain syndrome should also be hospitalized in a hospital for emergency reasons.
previous article
Vitamin D and children's health
next article
Main differential indicators in children
Up