There are contraindications. Specialist consultation is required.
Causes General symptoms Types of hemorrhoids Symptoms Stages Diagnosis Treatment Prevention
Hemorrhoids (hemorrhoids) are varicose, deformed and inflamed blood vessels (hemorrhoidal plexuses) located in the smooth muscles of the walls of the rectum and anus. They are a normal part of the rectum and are located at the junction of small arteries that become veins. Hemorrhoidal plexuses contain smooth muscle and connective tissue and are classified by where they are located in relation to the pectineal line, the point dividing the upper 2/3 and lower 1/3 of the anus. The anatomical difference is formed due to the type of cells lining the hemorrhoidal veins and the nerves that provide sensation. It is damage to these vessels that forms the signs of hemorrhoids.
Often people go to the doctor, noting the first signs of hemorrhoids in women or men - enlarged nodes, causing itching, pain or bleeding.
In our clinics you can treat hemorrhoids in the following ways:
- Hemorrhoid ligation surgery with latex rings
- Laser removal of hemorrhoids
- Non-surgical treatment of hemorrhoids
- Desarterization of hemorrhoids (new technique)
Hemorrhoids: causes of occurrence
Although the presence of hemorrhoidal plexuses is part of the normal anatomy of the rectum, if the nodes become inflamed, increase in size, and blood stagnates in them, a disease develops - hemorrhoids. Changes occur gradually, starting from barely noticeable and reaching severe and pronounced. Symptoms of hemorrhoids occur when pressure increases in the small vessels supplying the rectum and anus, causing the veins and plexuses to swell and fill with blood. This leads to an increase in the size of the nodes, which contributes to the appearance of symptoms of external or internal hemorrhoids. Increased pressure in the veins and the development of pathology can be caused by many factors, and the causes of hemorrhoids in women or men may vary. Common risk factors include:
- Lack of fiber-rich foods in the diet, which causes hardening of the stool. Difficulty during bowel movements causes a person to strain and strain, which increases the pressure in the blood vessels of the anus.
- Prolonged sitting on the toilet, which can increase the pressure in the blood vessels of hemorrhoids.
- Obesity;
- Diarrhea – both acute and chronic.
- Colon cancer or previous rectal surgery.
For women, an additional cause of hemorrhoids that affects treatment is pregnancy. Carrying a baby is associated with swelling and enlargement of hemorrhoids, which most likely occurs due to the increased pressure of the enlarged uterus on the rectum and anus. In addition, hormonal changes during pregnancy can weaken the muscles that support the rectum and anus, which form the tone of the veins.
Causes and risk factors for developing hemorrhoids
The occurrence of hemorrhoids is associated with the structural features of the rectum in this area. There are special anatomical formations here - cavernous or cavernous bodies, which in their structure are similar to the cavernous bodies of the penis. Essentially, they are intertwining vessels that are supported by connective tissue. Their main task is to close the anal canal.
If the connective tissue cannot support the choroid plexus, the outflow of venous blood is impaired. The vessels become overfilled, expand in size and bulge outward. As a result, a hemorrhoidal node is formed.
The following factors can lead to weakening of connective tissue:
- Excess weight, especially abdominal obesity, is especially dangerous.
- Pregnancy and childbirth.
- Sexual practices associated with anal stimulation.
- Regular physical activity involving lifting weights.
- Inflammatory diseases of the pelvic organs.
- Tumors of the pelvic organs.
- Bowel movement disorders, such as chronic constipation and diarrhea.
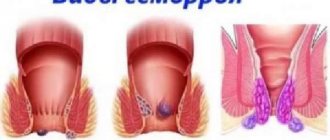
What are internal and external hemorrhoids
Internal hemorrhoids are located above the pectineal line and are covered with the same cells as those lining the rest of the intestine. External hemorrhoids occur below the line and are covered with skin-like cells.
Outer
Externally it manifests itself as hemorrhoids outside the anus. They are located near the sphincter. The nodes become inflamed and enlarge due to stagnation of blood in the pelvic area. If a blood clot appears in the external node, swelling forms, causing pain to the person. The patient feels a voluminous lump on sensitive thin skin. This development of the disease is typical with an incorrect diet, stagnation of blood in the rectum, low physical activity, and heavy physical exertion. When the skin that covers the node becomes thinner, a blood clot comes out, followed by bleeding.
Interior
With this form, hemorrhoids are almost invisible. They are located inside the anal canal, in the place where it passes into the rectum, under the mucous membrane. The nodes appear due to the protrusion of blood vessels and are usually painless. However, even in this case, hemorrhoidal thrombosis may occur. At an early stage, the disease can be recognized by a small amount of blood discharge after bowel movements.
Pathogenesis
Proctological disease develops when the arteriovenous cavernous plexuses increase and form during intrauterine development. Outwardly they resemble the corpora cavernosa of the genital organs. The plexuses are located above the dentate line or on the mucous membrane in the lower rectum. They are also localized under the dentate line, in the subcutaneous tissue in the anal canal. The plexuses are connected to each other using anastomosis.
The corpora cavernosa in the anus fill with blood and are responsible for sealing the closed sphincter. Previously, proctologists believed that chronic hemorrhoids develop due to varicose veins in the affected area. Today, there are a number of factors that influence the impaired functioning of internal organs. These include an increased amount of blood in the corpora cavernosa, as arterial inflow accelerates. Venous outflow slows down. Thrombosis forms, which leads to anemia, and the vascular wall of the anus becomes inflamed.
The superior rectal artery becomes wider than in healthy people. The number and density of blood vessels in the anal area increases. Muscles and veins weaken, become thinner, and worn out. Hemorrhoids enlarge and prolapse from the rectum. When defecating, the patient strains, thereby putting pressure on the exit of feces. Nodes move in the wrong direction.
How to determine external and internal hemorrhoids
Normal hemorrhoidal tissue is not visible because it must first swell and become inflamed or form a clot to cause symptoms. Swollen external hemorrhoids or internal prolapsed hemorrhoids outside the anus may be seen, but internal hemorrhoids are not visible because the nodes remain inside the anus. A thrombosed hemorrhoid will appear as a lump on the edge of the anus protruding from the anus and will be dark bluish in color due to the clot contained within the swollen blood vessel. A nonthrombosed hemorrhoid will appear as a lump of skin. Often several swollen hemorrhoids appear at the same time.
Symptoms of hemorrhoids in men and women
Acute hemorrhoids or exacerbation of a chronic process are the most common cause of complaints from the rectum and anus. Most common symptoms:
- painless bleeding from the anal area, blood stains on linen, toilet paper;
- anal itching;
- pain, discomfort in the anal area;
- swelling and the sensation of a lump or foreign body in the anus are associated with inflammation and exacerbation of chronic hemorrhoids.
Inflammation of internal hemorrhoids has special symptoms, for example, it can cause swelling. This in itself does not cause pain because there are no pain fibers attached to the veins above the pectineal line. Hard stool can damage the thinned mucous membrane of the node, causing painless bleeding. However, swollen hemorrhoids can also cause the muscles surrounding the rectum and anus to spasm, causing pain, especially if they prolapse through the anus. You can feel a lump along the edge of the anus. Internal hemorrhoids can also thrombose (clot), causing severe pain.
Inflamed hemorrhoids can produce mucus, which can cause inflammation of the skin around the anus, causing burning and anal itching. However, there may be other causes of itching, including yeast and other skin infections.
External hemorrhoids behave differently because the nodes are covered with “regular skin”, which contains pain receptors. Thrombosis of external hemorrhoids occurs when the underlying vein inside the hemorrhoid becomes blocked, causing severe pain due to the rapid stretching of the skin covering the hemorrhoid. You may feel a hard, painful lump in your anus. External hemorrhoids can also result in excess skin tags that can be felt at the edge of the anus and can cause difficulty cleaning the skin after bowel movements, leading to secondary skin infections.
Classification of hemorrhoids
Depending on the location of hemorrhoids, the following types of hemorrhoids are distinguished:
- Internal - nodes are located in the lumen of the rectum. During external examination they are not visible; they are detected during digital rectal examination and instrumental examination (rectoscopic examination, sigmoidoscopy). But if the nodes are large or the ligamentous apparatus is weakened, they can fall out of the anal canal when straining, for example, during defecation. In this case, they can be injured, bleed or pinched.
- External - the nodes are localized below the dentate line of the anal canal and can be detected by visual examination. They should not be confused with prolapsed internal hemorrhoids; in particular, the external nodes are covered with skin, and the internal ones with mucous membrane. A frequent complication of this type of hemorrhoids is thrombosis, which is accompanied by a clear clinical picture in the form of severe pain.
- Combined - the patient has nodes above and below the dentate line.
According to the type of course, acute and chronic hemorrhoids are distinguished, but many clinicians consider acute hemorrhoids to be a clinical manifestation of a previously undiagnosed disease.
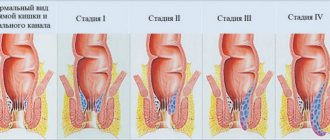
Stages of hemorrhoids
Hemorrhoids can be acute (when the disease develops rapidly and is accompanied by severe pain and discomfort) and chronic. In the second case, a mild pain syndrome is observed, the disease develops over a long period of time with periods of exacerbation (bleeding, prolapse and pinched nodes occur).
First stage
Mild discomfort is felt, and short-term bleeding is typical, which occurs after any overexertion - hard work, defecation. Inflammation is detected only during examination. At this stage, conservative treatment, sclerotherapy, and photocoagulation are recommended.
Second stage
It is characterized by periodic prolapse of inflamed hemorrhoids, while bleeding may be absent. The dropped nodes are set on their own without much effort. Conservative treatment, sclerotherapy, photocoagulation, ligation, or a combination of these techniques is recommended.
Third stage
Dystrophic changes occur in the sphincter, it weakens, as a result of which prolapsed hemorrhoids can only be set manually. The course of the disease is accompanied by severe itching, frequent and heavy bleeding. Ligation, surgical treatment, and a combination of techniques are recommended.
Fourth stage
Hemorrhoids are in a constantly prolapsed state along with the rectal mucosa. It is impossible to set them. It may be accompanied by bleeding or occur without it. Inflammation can affect nearby tissues. Surgery to remove hemorrhoids is indicated.
External hemorrhoids
As we already know, with external hemorrhoids, hemorrhoids form below the dentate line of the anal canal. In this case, the nodes are visible to the naked eye, or the patient can feel them on their own - they look like lumps and are often painful on palpation. The first sign of pathology is usually pain. It can occur on its own, without provoking factors, but is more often associated with defecation, prolonged sitting or standing, and physical activity associated with heavy lifting. In common stages, pain is provoked by sneezing, coughing, and running.
Bleeding occurs less frequently than with internal hemorrhoids, and does not appear as blood in the stool, but as stains on linen or toilet paper. If the nodes are large, a feeling of a foreign body appears.
Diagnosis of hemorrhoids: determining the cause and symptoms in men and women
Common symptoms of hemorrhoids include itching, pain, rectal fullness or hardness, and bleeding. Diagnosis is made based on a history and physical examination. The history may indicate associated symptoms, including constipation, problems with bowel movements, and straining to go to the toilet. Your doctor will ask more questions to look for other causes of rectal bleeding, including tumors, inflammatory bowel disease, and gastrointestinal bleeding.
To confirm the diagnosis, determine the cause of hemorrhoids and select treatment, an examination is performed. It involves a rectal examination, in which a finger is used to feel for abnormal lumps or masses. A rectal examination may be delayed if pain or swelling is severe. Additionally, hemorrhoids and constipation may be associated with anal fissures in the skin surrounding the anus. The associated pain and spasm makes rectal examination very painful. If the doctor is concerned that symptoms, especially rectal bleeding, cannot be explained by hemorrhoids, an anoscopy may be considered. This is a procedure in which a lighted tube is inserted to view the anus. If there is concern that bleeding is coming from other areas of the colon, a sigmoidoscopy or colonoscopy may be performed. These procedures are usually performed by a gastroenterologist or surgeon.
Depending on the situation, blood tests may be ordered. If there was heavy bleeding, you need to check your hemoglobin or red blood cell levels. If the patient is taking blood thinners, a coagulation test is necessary.
Diagnostics
For diagnosis, the patient visits a proctologist. The private proctology clinic uses modern treatment methods and new equipment. The proctologist receives information about the patient’s medical history, studies the medical history and data from diagnostic studies. Digital examination, anoscopy and sigmoidoscopy are performed. An examination of the rectum is carried out on a gynecological chair. The patient bends his knees. A medical specialist examines external and internal hemorrhoids, examines the condition of soft tissues, feces and mucous secretions.
Anoscopy allows you to determine the location, size and condition of internal hemorrhoids. For a rectal examination, the patient should push to ensure that the information is more accurate. If there is a suspicion of damage to parts of the large intestine, irrigoscopy and colonoscopy are prescribed. During the examination, the doctor excludes or confirms the presence of concomitant diseases of the esophagus, rectum, and anus. First of all, the presence of malignant neoplasms should be excluded.
Methods for treating internal and external hemorrhoids
When hemorrhoids occur or worsen, it is important to choose the right treatment methods. It can be conservative, minimally invasive and surgical.
“SM-Clinic” provides services for prompt diagnosis and effective treatment of hemorrhoids in clinics in St. Petersburg. Both non-surgical and surgical treatment are used, including laser surgery for hemorrhoid removal. The disease can have several stages, which determines the type of treatment.
Non-surgical treatment of hemorrhoids
Conservative therapy
Allows you to reduce the frequency, duration and severity of exacerbations. It involves taking general medications (normalize blood flow, increase venous tone, etc.) and using local remedies (suppositories, ointments, gels to eliminate inflammation, pain, itching, prevent thrombosis, etc.).
Ligation with latex rings
One of the most modern and popular low-traumatic methods of treating internal hemorrhoids. Through an anoscope, a latex ring is applied to the stem of the hemorrhoidal node, which leads to compression of the tissues and disruption of blood circulation in them. After 1-2 weeks, the node is rejected.
Sclerotherapy
During the procedure, with the help of special drugs (sclerosants) that are introduced into the node, the inner lining of the venous wall is affected, which leads to its damage and subsequent gluing. As a result, the pathologically deformed vein no longer participates in the blood circulation process and dies. The technique is effective only for small hemorrhoids; the risk of relapse cannot be excluded.
Infrared photocoagulation
This technique involves temperature exposure to the node. The coagulator is applied to the node at 3-5 points. As a result, a burn of 2-3 mm appears. The morbidity of this method is extremely low, and patients become able to work on the same day or within 24 hours. The damaged node disappears after some time.
Surgical techniques
Surgical removal (hemorrhoidectomy)
Surgery is resorted to in the third and fourth stages of the disease. The surgical method involves excision of the hemorrhoidal node along with part of the mucous membrane and is indicated for chronic hemorrhoids of stages 3 and 4, severe bleeding, frequent relapses and thrombosis of the nodes. Surgery takes little time, and patients recover quickly. The method is considered one of the most effective, where the number of relapses is reduced to an absolute minimum.
Laser removal of hemorrhoids
The idea is to cauterize the vessels with a laser beam. This is a modern, painless, low-traumatic and effective way to treat hemorrhoids at any stage. The operation itself takes only 15 minutes, is performed under local anesthesia and does not require the patient to stay in the hospital for a long time.
Dearterization of hemorrhoids (HAL-RAR method)
This is a minimally invasive operation aimed at ligating the vessels, so that blood stops flowing to them. As a result, the nodes stop bleeding, are deprived of nutrition and disappear. The technique is highly effective (up to 95%), painless and does not require long recovery.
Treatment tactics depend on the stage of the disease, the severity of clinical manifestations and diagnostic results. At the first and second stages of hemorrhoids, conservative treatment and minimally invasive methods are recommended - sclerotherapy, photocoagulation, ligation or a combination of these methods. In the third and fourth stages, surgery is required in most cases.
Treatment of chronic hemorrhoids
The main and auxiliary directions of therapy are determined only by the attending physician after a detailed diagnosis of the problem. The main indicator of the intensity of therapy is the degree of the disease and the severity of characteristic symptoms. Elimination of symptoms must be comprehensive and consistent. In the initial stages of the disorder, the main emphasis is on relieving pain and inflammation. In case of complications, the main goal of therapy is to exclude the very cause of the disease.
As part of conservative therapy, doctors recommend:
- Taking medications with analgesic and anti-inflammatory effects. Thrombolytics and venotonics, which have a restorative effect on blood vessels, local antiseptic and hemostatic suppositories, ointments that quickly relieve symptoms and promote the healing of anal fissures, have proven themselves well.
- Following a strict diet - the list of permitted foods includes green vegetables, berries, lettuce, lean meat and fish. Freshly squeezed vegetable juices, prunes, beets and pumpkin are good for digestion. Do not forget about the drinking regime - at least 2 liters of water per day.
- Physiotherapeutic procedures, strict hygiene.
In cases where chronic hemorrhoids are widespread and cause maximum discomfort to the patient, doctors recommend minimally invasive procedures or surgical removal of the nodes. The safest and least traumatic manipulations are considered to be sclerotherapy of nodes, infrared and laser coagulation, ligation with latex rings or classic hemorrhoidectomy.
How to get rid of hemorrhoids at different stages
Hemorrhoids will recur after conservative treatment in approximately 50% of cases, while the recurrence rate after surgery is only 5%. The goal is to control hemorrhoid inflammation through diet and hydration so that surgery is not required. In this regard, hemorrhoids are a lifelong condition that needs to be managed.
Hemorrhoids of 2 and 3 degrees are initially treated conservatively or using minimally invasive methods. These include injections into the hemorrhoidal vein to sclerosize or harden it, using rubber bands to cut off the blood supply and cause the hemorrhoidal tissue to shrink, or other procedures that cause the lining to shrink and die.
Danger of disease
Lack of timely treatment can become a source of various complications. Further progression of the pathological process leads to:
- To anemia - the condition is provoked by prolonged and abundant loss of blood from damaged tissues.
- Inflammatory processes - the anomaly affects nearby areas, provokes the formation of purulent sacs in them - abscesses. Pathology has dangerous consequences and requires long-term therapy.
- Cracks in the area of the anus - they are a source of pain and create favorable conditions for the subsequent penetration and active functioning of infectious agents. The result of soft tissue damage is an abscess (purulent inflammation, with elevated temperature, pain), the treatment of which consists of surgical intervention.
- Itching – disrupts the patient’s psycho-emotional state due to a constant feeling of discomfort. Mechanical damage to the skin when scratching leads to the addition of secondary infections and becomes a source of the formation of local tumors.
- Sphincter insufficiency is diagnosed more often in older people, resulting in incontinence of feces and gases.
To avoid the development of the consequences of hemorrhoids, a timely visit to a proctologist, a complete examination and subsequent therapy are necessary.
Why are hemorrhoids dangerous?
The most common complications of hemorrhoids are inflammation, thrombosis or bleeding. It is important to remember that rectal bleeding or blood in the stool is always abnormal, and although it can be caused by a relatively benign cause (such as hemorrhoids), other, more serious causes can be life-threatening. These include bleeding from ulcers, diverticulitis, inflammatory bowel disease and tumors. This is especially important if a person is taking blood thinners.
Causes
Proctologists identify a number of reasons that provoke the development of hemorrhoids. These include genetic predisposition. In this group of the population, increased intra-abdominal pressure and impaired functioning of the esophagus are observed in utero. Experts call a sedentary lifestyle one of the main reasons. An unbalanced diet, disrupted daily routine and lack of normal sleep lead to a deterioration in metabolism, which provokes an increase in hemorrhoidal cones. Heavy physical activity and gastrointestinal disorders are among the factors that influence the appearance of chronic hemorrhoids.
More often, the disease is diagnosed in people who often strain during bowel movements, and in those who suffer from multiple bowel movements. Feces come out of the rectum several times at intervals of several minutes. Accelerating bowel movements by pushing leads to the formation of anal fissures and scars. In women, hemorrhoids develop during pregnancy, as the uterus puts pressure on the internal organs. The abdominal organs are especially affected by intra-abdominal pressure.
Prevention of hemorrhoids
Prevention is the most effective treatment. Diet and adequate fluid intake are very important to maintain normal bowel movements. Symptoms of hemorrhoids can occur with the passage of hard stools and constipation, as well as with diarrhea and frequent bowel movements. People with constipation may need a high-fiber diet, adequate fluids, and stool softeners. Those who have excessively frequent bowel movements may need antidiarrheal medications and dietary adjustments. These preventive measures reduce the strain required to have a bowel movement, thereby reducing the pressure in the blood vessels to prevent swelling.
The SM-Clinic Surgery Center provides services for prompt diagnosis and effective treatment of hemorrhoids using non-surgical methods and surgical techniques. Our patients recover within 24 hours in a comfortable hospital setting and quickly return to their normal lifestyle. Other treatment methods are also used, depending on the stage and type of disease. Advanced equipment is used for diagnostics, ensuring accuracy and speed of obtaining results.
Therapy methods
The specialists of the proctology department of the Global Clinic have at their disposal several methods of treating the disease at all stages of its course. The following treatment options are used at Global Clinic:
- infrared photocoagulation (cauterization of the hemorrhoid). Used to treat stage 1 hemorrhoids;
- sclerotherapy (the venous tangle is treated with a special solution for its destruction). Used to treat stage 1-2 hemorrhoids;
- latex ligation (latex rings are placed on the base of the vascular formation). Used to treat stage 1-2 hemorrhoids;
- radio wave therapy (using radio waves). Shows its effectiveness at all stages of disease progression;
- laser vaporization with desarterization of formation - effective at stages 2-3 and less often at stages 4;
- at stage 4, hemorrhoidectomy in various modifications.
Prices
Price (RUB)In installments* (RUB)Consultation with a surgeon on the operation (SPECIAL)0—Online doctor’s opinion on the operation (SPECIAL)0—Hemorrhoidectomy Cat. I. complexity from 35000—Non-surgical removal of hemorrhoids, category I. complexity from 3550—Coagulation of a hemorrhoid using radio wave surgery from 6400—Thrombosis of hemorrhoids (1 ligation) from 300—Thrombectomy from an external hemorrhoid from 4800—Removal of a thrombosed hemorrhoid I cat. complexity from 8500—Removal of a thrombosed hemorrhoid, category II. complexityfrom 11000—Removal of a thrombosed hemorrhoid, category III. complexityfrom 14500—See full list
Hide
* You can read more about the conditions here - Treatment on credit or in installments
The cost is preliminary. The exact cost of the operation can only be determined by a surgeon during a free consultation.