An anal fissure is a linear or oval-shaped defect in the mucous membrane of the rectal canal. If the ulcer heals within 8 weeks, proctologists speak of an acute anal fissure. A chronic anal fissure is indicated by the presence of a sentinel tubercle at the bottom of the wound defect. Proctologists at the Yusupov Hospital know how to quickly cure an anal fissure.
Doctors at the proctology department treat acute anal fissure using the latest medications that are effective and have minimal side effects. They are used topically in the form of ointments, gels and rectal suppositories. If the pathological process enters the chronic stage, minimally invasive procedures (chemical sphincterotomy) and excision of the mucosal defect with a surgical or laser scalpel are performed. After complex treatment, most patients do not experience a relapse of the disease.
Causes
The reasons that result in anal fissures can be identified as follows:
- Strong physical activity.
- Constipation. With chronic constipation, very hard stool is constantly formed. They lead to damage to the tissues of the anus and microcracks. Straining, which is carried out by a person, increases the pressure in the rectum, which leads to tissue rupture and, as a result, the appearance of a crack.
- During childbirth, a rupture of the mucous membrane is possible, as a rule, with strong straining and the application of forceps, which are used for difficult childbirth.
- Inflammatory processes in proctitis. The strength of the tissues of the anus decreases during inflammation, and this leads to damage to them by feces.
- Poor chewing of food, poor nutrition. Sharp pieces of food that remain undigested (seeds, nuts) during bowel movements can damage tissue.
- Intestinal examinations.
- Anal sex.
- Rapid, incorrect administration of an enema.
- Wrong diet: alcohol, spicy food.
- Prolonged sitting.
There are basic signs that allow you to diagnose an internal anal fissure very quickly and easily. In general, patients experience the following symptoms:
Acute pain during bowel movements, which patients describe as a “broken glass” or “burning” sensation. Such pain begins in the anus, then begins to radiate to the anus, then to the groin and lower abdomen. This syndrome may continue for some time after the act of defecation.
Bleeding during bowel movements. They may appear as a small streak of blood in the stool. In some patients, the fissure may bleed between bowel movements.
The presence of spasm of the anal sphincter, which can also be accompanied by severe pain.
Some patients may experience such symptoms only for a while, which gives rise to the misconception that the fissure can be cured, but this phenomenon is extremely rare. If you do not follow certain treatment measures, it is difficult to achieve the desired result, and the possibility of relapse is very high. An advanced anal fissure is much more difficult to treat, so it is important to trust a qualified professional.
Make an appointment
Reasons for the development of pathology
The appearance of an anal fissure can be spontaneous or observed due to tissue trauma. The spontaneous appearance of ruptures is associated with the activity of the intestinal flora and lack of hygiene in the genital area. In case of traumatic injury, the tension of the mucous membrane is caused by tension in the internal walls of the anus. As a result of spasm caused by straining during defecation, the mucous membrane of the anus bursts and forms a wound erosion.
The formation of cracks in the anus is more typical for young people and is more common among the female population.
The disease develops for a number of reasons, which are united by one etiological factor, which is based on sphincter tension. The following reasons for the formation of anal fissures are distinguished:
- >stool disorders (constipation, dry stool, frequent bowel movements, diarrhea);
- pathologies of the digestive and hepatobiliary tract (gastritis, reflux esophagitis, gastric or duodenal ulcers, cholecystitis, cholelithiasis, Crohn's disease, etc.);
- labor activity;
- tumor processes (endometriosis, rectal cancer);
- STDs (syphilis, HIV, etc.)
- vascular diseases (obliterating atherosclerosis, varicose veins in the pelvic area, vasculitis, thrombophlebitis);
- external traumatic injury (medical manipulation during examination of the rectum, enema or use of adult toys);
- anal sex.
Chronic fissures are formed as a result of secondary inflammatory processes localized in the anorectal area.
Types and symptoms
After childbirth, an acute anal fissure may form or worsen. In the first case, the patient had no signs of anal fissure before giving birth, and the second type of anal fissure is an ulcerative defect that existed for longer than 2-3 months. The crack could have formed before pregnancy, and worsened under stress during childbirth.
Anal injuries most often occur brightly, with severe pain. Sometimes there is a latent (hidden) course of an anal ulcer. With sharp cracks, the defect has smooth edges. This helps achieve quick healing. If the patient has a chronic version of the disease, an ulcer with rounded, thickened and calloused outlines, granulations and a skin fold called the “sentinel tubercle” is formed.
Anal fissures after childbirth can be single or multiple. They are located mainly on the anterior wall of the anal canal and occur when tension occurs during pushing. Anal fissures are manifested by the following symptoms:
- sharp burning pain;
- spasm of the anal sphincter;
- the presence of a small amount of scarlet blood.
The pain occurs suddenly and is associated with the act of defecation. It can be combined with burning, distension in the anus, and pressure. Sometimes the pain radiates to the perineum, thigh, sacrum. Often, in the presence of an anal fissure after childbirth, not only the act of defecation is disrupted, but also urination. The moment of formation of an anal fissure during childbirth may be missed, since the woman already experiences severe discomfort.
If after childbirth a chronic fissure worsens and the following symptoms appear:
- Pain does not occur at the time of defecation, but after bowel movement from feces - after a few minutes or even hours (this does not apply to those cracks that existed before childbirth and deepened due to additional damage - in this case, the woman feels acute pain during bowel movements );
- Disruption of the normal anatomical structure of the sphincter due to spasm and changes that are associated with the proliferation of connective tissue in areas of defects;
- Bleeding in the form of drops or smears on toilet paper.
Proctologists speak of a chronic fissure if more than 2 months have passed since the formation of the ulcerative defect. The formation of ulcers is facilitated by constipation that occurs after childbirth, as well as infections and other provoking factors. Patients may develop complications of anal fissure:
- Profuse bleeding from the rectum leading to anemia;
- Pectenosis – replacement of the sphincter muscles with connective tissue and loss of the ability to maintain the “tension-relaxation” cycle, as a result of which feces are not excreted and coprostasis occurs;
- Paraproctitis is an infectious inflammation of the peri-rectal tissue spaces, which is manifested by weakness, fever, and throbbing pain in the rectum and perineum.
Recently, malignant degeneration of ulcers has been increasingly occurring, which occurs with long-existing and often damaged cracks. You should make an appointment with a proctologist immediately if the size of the defect increases, blood is released in the feces, or the severity of pain decreases. To identify signs of an anal fissure in a woman after childbirth, the proctologist examines the anus, digital examination of the rectum and anoscopy after preliminary anesthesia of the area of the ulcer.
The ABCs of Hemorrhoids
It can be difficult for an uninitiated user to find answers to questions when it comes to problems with the anus. Together with a surgeon, a doctor of the highest category, Sergei Dmitrievich Trukhmanov, we decided to create a material in which we collected all the terms related to this topic. For the convenience of our readers, we have compiled the article in a convenient dictionary format, where you will find the meaning of all the necessary terms. Remember that self-medication can aggravate the disease, so when the first symptoms appear, seek help from a specialist.
Anal velvet
or fimbria is a radial mucocutaneous fold that usually disappears when the anus is stretched. These are often consequences of anal thrombosis, birth injuries, and prolapse of nodes. It should be distinguished from stage 4 hypertrophy of hemorrhoidal nodes, when the internal nodes are visible from the anus.
Anal itching
occurs only as a result of exposure to unfavorable factors on the skin around the anus: worms (pinworms), ingress of mucus from the rectum (with insufficient retaining function of the anus, significant prolapse of the mucous membrane, with severe inflammation of the rectal mucosa), ingress of purulent discharge (with chronic paraproctitis) . Often occurs with profuse sweating in patients with obesity or so-called. "deep anus." However, there is the concept of “idiopathic anal itching,” when no cause can be found. This is the most unpleasant course of the disease, but I have never had such patients - I always managed to find the cause and eliminate it.
Anal tone
- state of the anal muscles at rest. With a decrease in tone, any degree of incontinence is possible: from gas to dense feces. Increased tone indicates a problem that needs to be found.
Anal polyp
- a neoplasm of the anal canal, occurring either from an enlarged anal papilla or from organized internal thrombosis. Often true polyps (glandular and villous) are also found in the anal canal, i.e. mucosal neoplasms capable of malignant degeneration. Removal of all polyps is mandatory, since they can become a substrate for the development of a cancerous tumor, and it is impossible to know their histological structure without removal.
Anal incontinence
- this is incontinence of gases or feces, most often the result of a decrease in the tone of the muscles of the anus and a weakening of their volitional efforts. Congenital and acquired forms of the disease are possible (including after operations, childbirth and injuries).
Anococcygeus pain syndrome
or coccydynia or acute anal pain syndrome. The leading symptom is pain in the perineum of varying intensity. The cause of severe pain can be a tumor, internal hemorrhoidal thrombosis, anal fissure, paraproctitis, trauma to the coccyx, and neuroma of the coccygeal plexus. In women, pain in the sacrum and coccyx area with irradiation to the anus can be caused by disease of the uterus and appendages, endometriosis.
Anorectal reflex
- when the rectum is filled with contents, the internal sphincter relaxes, and the urge to defecate appears. Retention is possible only by tension of the external sphincter.
Pain in the anus
- possible only in 5 cases: anal fissure, anal thrombosis, prolapse and strangulation of hemorrhoids, paraproctitis and tumor of the anal canal.
Knots falling out
— sliding of hemorrhoids from their places due to the destruction of the ligamentous apparatus of the submucosal layer. Manifested by a sensation of foreign bodies outside the anus. At first it adjusts on its own (and the sensations disappear); at a later stage, assistance is required (finger, hand, cold, forced position). It is one of the symptoms of hemorrhoidal disease. Treatment is suture ligation with lifting (desarterization), Longo operation, radical hemorrhoidectomy.
Rectal prolapse
- turning the rectum out through the anus, first when straining, and then even just in a vertical position. It should be distinguished from anal prolapse, as the last stage of hemorrhoidal disease.
Haemorrhoids
or more correctly -
hemorrhoidal disease
. The most typical symptom complex: blood, prolapse of nodes, pain, itching. It is possible to have both a combination of symptoms and their appearance separately.
Hemorrhoidal bleeding
. In contrast, blood discharge during bowel movements in small quantities (from 1-2 milliliters to 1-2 tablespoons), and not affecting health, can cause the development of anemia, loss of consciousness, fainting, etc. A single release of blood can reach 100 – 200 milliliters. It should be distinguished from rectal bleeding that occurs with diverticulosis, polyps, tumors, and ulcerative colitis. Diagnosis and treatment of all types of bleeding - only in specialized institutions.
Hemorrhoidal thrombosis
can be external or internal. Painful “bumps” appear, usually bluish in color. This is a consequence of a rupture of one of the vessels of the hemorrhoidal plexus with hemorrhage into the surrounding tissue. Treatment is either surgical - removal of thrombotic masses, or conservative - thrombolytic and anti-inflammatory, phlebotonic and analgesic therapy. After surgical treatment, there are no traces of thrombosis, but there is pain until the wounds heal completely. After conservative treatment, dense, enlarged nodules may remain, which can become a source of problems in the future, but the treatment itself occurs with less pain. The duration of treatment depends on the size of the thrombosis, the duration of the thrombosis, and the age of the patient: from 2-5 days to 3-4 weeks.
Hidradenitis suppurativa perianalis
- a severe disease of the perianal sweat glands. The patient undergoes many surgical interventions, often resulting in disability.
Diarrhea
or simply diarrhea. May signal a serious bowel problem in the same way as constipation. Very often, thinning and frequent stools occur in people with tumors and large colon polyps. The body does this to prevent intestinal obstruction.
Defecation
- a complex reflex act of removing feces through the anus. In everyday life it is called a “chair”.
Dysbacteriosis
- a change in the state of the intestinal microflora, which can be caused by various reasons. According to the majority of surgeons and coloproctologists, there is no need for separate diagnosis and treatment. Treatment occurs within the framework of the identified pathology, since a healthy colon independently regulates the colonization of its bacterial flora (which takes an active part in digestion).
Constipation
- defecation with a stool consistency denser than thick porridge. The less often the bowel movements, the more pronounced the constipation and the more severe its consequences for the anus.
Infrared (IR) photocoagulation
- an outpatient method of influencing bleeding hemorrhoids and the so-called “daughter accumulations of cavernous tissue” of the anal canal. Has limited use, not radical.
Bowel examination
. This or an X-ray examination - irrigoscopy, passage of barium through the intestines; or endoscopic: sigmoidoscopy, sigmoidoscopy, fibrocolonoscopy. The latter is used for preventive purposes once every 3 years in people over 45-50 years old to identify and remove polyps and for diagnostic purposes for all diseases of the anus and rectum. For other methods there are separate, strictly limited indications.
Foreign bodies of the rectum
- objects inserted into the anus by a person for any purpose, indigestible swallowed objects, so-called. fecal stones must be removed in a specialized hospital.
Latex ligation of hemorrhoids
- used to reduce the size of nodes and stop bleeding from them in a non-surgical way. A widely used method of temporarily improving the condition of patients. It is not radical, serious complications are possible (although very rare), so I personally do not use it.
Lifting
mucosa with suture ligation and radical surgery has proven itself well. In most cases, it allows you not to excise excess mucosa.
Operation Longo
— hardware circular resection of the mucous membrane of the lower ampullary part of the rectum with the intersection of the branches of the arteries feeding the hemorrhoids. An excellent method for the treatment of internal hemorrhoids with prolapse, but without an external component. I used it widely, but now I rely more on my own hands, performing suture ligation with a liftig. Recurrences of prolapse of nodes and mucous membrane of the anal canal are due to the tenderness of the postoperative scar and persistence of constipation. Recently, publications have appeared about serious complications including death, so its use has begun to be limited throughout the world.
Paraproctitis
- can be acute and chronic. Acute paraproctitis is ulcers around the anus of varying size and location. You should not trust the treatment of such ulcers to NOT proctologists. The outcome is possible in chronic paraproctitis, anal incontinence or pararectal fistula.
Perianal condylomas
- often a viral disease that develops with certain changes in immunity. Treatment is usually surgical with mandatory correction of immunity.
Radical operation
for hemorrhoids according to Milligan and Morgan. In the West it is considered the “gold standard” for advanced stages. In my opinion, it can be used at any stage if the main goal is to guarantee against relapse. The use of modern suture materials and rectal anesthetics helps reduce pain, and a cosmetic effect appears with transverse suturing of mucocutaneous wounds.
Rectocelle
- thinning of the rectovaginal septum of varying degrees, most often of postpartum origin. Both proctologists and gynecologists treat. It is possible to install mesh implants.
Sclerotherapy
for hemorrhoidal disease is a controversial topic. Domestic specialists inject sclerosant into the node, causing thrombosis. Western proctologists inject the drug under the mucous membrane above the node in order to fix the mucous membrane in place as a result of aseptic inflammation. I don’t see the point in either one if the specialist knows the suture ligation technique.
Strictures
rectum and anal canal. They develop after injuries, operations, purulent diseases. A common cause is chronic anal fissure. Treatment is either bougienage or surgery.
Anal fissure
- this is the name of any superficial damage to the mucous membrane of the anal canal. When the traumatic factor is eliminated, it heals independently with adequate treatment.
Chronic anal fissure
is a complication of chronic hemorrhoids with prolapse of nodes, therefore it does not heal without surgery.
Suture ligation
or disarterization of nodes or dearterization of them. It can be performed at any stage of the disease, but often radical surgery is a better choice. Absolutely indicated for isolated internal hemorrhoids. And no special anesthesia is required after the operation, and the long-term results are encouraging. But if it is necessary to eliminate the external component, its main advantage - low postoperative pain - is lost.
"Bumps"
near the anus, as patients often say, these are most often thrombosed external nodes or internal ones that have fallen out. It is not recommended to treat without examination by a proctologist.
Epithelial coccygeal tract
or pilonedal sinus or coccygeal cyst or sacrococcygeal suppuration - a congenital anomaly associated with incomplete reduction of the former tail muscles. Treatment is only surgical, preferably in a specialized hospital.
Diagnostics
Proctologists make the diagnosis of anal fissure based on the following criteria:
- characteristic complaints;
- anamnesis data;
- results of clinical and instrumental examination.
Patients who have an anal fissure complain of pain in the anus during and after defecation, bleeding during bowel movements in the form of streaks in the stool and marks on toilet paper. When collecting anamnesis (information about the development of the disease and previous treatment), doctors identify factors that may be the cause of an anal fissure in a given patient:
- insufficient dietary fiber intake;
- carbohydrate-rich, fatty, spicy foods;
- constipation or diarrhea;
- difficult childbirth;
- cycling, weight lifting.
The proctologist examines the patient on a gynecological chair, in a supine position, with the legs brought as far as possible to the stomach or in the knee-elbow position. Examination of somatically severe patients is carried out in the lateral position. During an external examination of the anus and perineum, the doctor pays attention to the shape of the anus, its gaping, the presence of deformations and scar changes, and the condition of the skin.
During the examination, proctologists determine the presence of a sentinel tubercle. In order to clearly examine the lower edge of the anoderm defect, assess its location, shape and size, the doctor separates the edges of the anus. In the presence of an anal fissure, the proctologist sees a linear or ellipsoidal defect (erosion or ulcer) with smooth edges, which does not extend beyond the anatomical boundaries of the anal mucosa
Using digital examination, doctors determine the presence of anoderm defects, the tonic state of the anal sphincter and the strength of volitional contractions. In the presence of an anal fissure, the sphincter tone is increased. After pain relief, proctologists perform anoscopy, sigmoidoscopy, and colonoscopy. The pressure in the rectal lumen is assessed using profilometry. This research method provides recording of pressure in different planes along the entire length of the anal canal. Using a computer program, a graph of the distribution of pressure values is constructed and the maximum average pressure values and the asymmetry coefficient are calculated. The processing program allows analysis of pressure data at any level of the cross-section of the anal canal.
If the disease lasts no more than 2 months, there are no scar changes in the area of the bottom and edges of the anal fissure, proctologists make a diagnosis of “acute anal fissure”. An anal fissure is considered chronic if one of the following criteria occurs:
- More than 2 months have passed since the first episode of pain;
- the sentinel tubercle and cicatricial edges of the ulcer are determined;
- fibers of the internal sphincter are present at the bottom of the defect;
- there is a fibrous polyp of the anal canal.
After examining the patient, proctologists at the Yusupov Hospital make a differential diagnosis of anal fissure with other diseases of the rectum, which manifest themselves with similar syndromes: hemorrhoids, ulcerative colitis, polyps, cancer.
Make an appointment
Clinical symptoms
Anal erosions are accompanied by severe pain, which manifests itself in the form of spastic pains. The pain intensifies when the sphincter tenses during the passage of feces, or when urine and intimate hygiene products come into contact with the wound surface. When collecting anamnesis, a number of other symptoms are of clinical significance:
- traces of blood in bowel movements, on toilet paper or underwear;
- constant itching and burning in the anus;
- conscious avoidance of bowel movements;
With constant pain, patients need mechanical and medicinal laxatives.
Conservative therapy
An acute anal fissure causes sharp pain during bowel movements and after defecation. To heal an acute anal fissure, proctologists prescribe medications that relieve painful spasm of the anal sphincter. The most effective in this regard are rectal suppositories with nitroglycerin, but they often cause headaches in patients.
Conservative treatment of acute anal fissure consists of the following measures:
- oil microenemas that facilitate bowel movements;
- taking medications that provide soft stools that do not require straining;
- sitz baths with furatsilin, chamomile infusion after each bowel movement;
- ointment applications to the anus or insertion of suppositories into the anus, which have an analgesic, anti-inflammatory and wound-healing effect.
Often the cause of anal fissure is prolonged diarrhea. To combat it, doctors prescribe adsorbents, coatings and enzyme preparations. For chronic anal fissure, therapy is supplemented with medications that relax the sphincter around the anus. This therapy is effective in 50-60% of patients. Proctologists at the Yusupov Hospital do not carry out conservative measures in the presence of a fibrous polyp with a diameter of more than 1 cm or protruding into the anus, as well as in cases of persistent changes in the internal sphincter that prevent its relaxation.
If there is a defect in the mucous membrane of the anal canal, proctologists at the Yusupov Hospital carry out local conservative therapy with ointments and suppositories that contain painkillers, stimulating epithelialization and antimicrobial agents.
The effect of suppositories for anal fissures is as follows:
- Healing the resulting defect in the mucous membrane of the anal canal;
- Restoring the integrity of damaged tissues;
- Anti-inflammatory, antibacterial;
- Pain reliever;
- Decongestant.
Due to the presence of oil in the composition of suppositories for the treatment of anal fissure, when they are used, the stool becomes soft and the walls of the ulcer are not injured. Due to their ease of use, good absorption and quick action, suppositories are most often prescribed for healing anal fissures. When using rectal suppositories for anal fissures, the active substance is practically not absorbed into the blood, does not enter the systemic circulation and does not cause an allergic reaction.
Choosing an anal fissure treatment method
A
anal fissure is a spontaneously occurring linear or ellipsoidal defect (ulcer) of the mucous membrane of the anal canal. The incidence of anal fissure (according to patient visits) ranges from 11 to 15% among all diseases of the colon and is 20–23 cases per 1000 adults. Young and middle-aged women are more often affected.
Etiology and pathogenesis
The causes of anal fissure are numerous. Among them, the most likely are considered: vascular disorders, changes in the perianal epithelium (parakeratosis), neuromuscular changes and injury to the anal sphincter. The most common cause of acute fissures is defects in the mucous membrane of the anal canal, which develop during the passage of hard feces. The posterior wall of the anal canal has anatomical prerequisites for the formation of cracks: the deeper distal parts of the anal sinuses (crypts) are located here, and the tendon endings of the anal sphincter muscles also converge. In women, the weak point of the anal canal is its anterior part, where the vulva, vagina and fibrous center of the perineum seem to converge. Therefore, fissures in the anterior part of the anal canal occur mainly in women. Cracks on the side walls of the anal canal are relatively rare.
The fissure is often combined with hemorrhoids. The medial walls of internal hemorrhoids are essentially the walls of the anus. They are located in the area of the anorectal line, which is most susceptible to injury during defecation. In addition, circulatory disorders (blood stagnation, thrombosis) in this area, especially in the posterior and anterior parts of the anal canal, may be accompanied by the formation of linear ulcers, similar in nature to varicose ulcers, which explains the chronic course of many anal fissures with hemorrhoids. Chronic inflammation of this area can gradually lead to fibrosis and loss of elasticity of the mucous membrane of the anal canal, and subsequently to ruptures with the formation of acute and chronic fissures.
The formation of anal fissures can also be caused by neurogenic disorders with prolonged spasm of the internal, and especially external, anal sphincters. Thus, anal fissure is a polyetiological disease, which must be taken into account in the process of its treatment
.
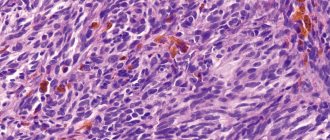
Pathological anatomy
The area of the mucous membrane in these areas, exposed to the highly virulent rectal flora, becomes scarified, and then thickens, deepens, and thus a real crack is formed - a longitudinal defect of the mucous membrane with clear edges and a bottom. At the bottom of such a crack-ulcer, due to constant nonspecific inflammation, the nervous structure of the affected area of the wall of the anal canal changes pathologically: the nerve endings lose their sheath and become exposed, which leads to severe pain. The upper pole of the defect remains within the dentate line, i.e., it does not extend to the rectal mucosa. In the chronic course, the edges of such an ulcer become compacted and thickened, especially in the distal part of the fissure, where a polypoid connective tissue thickening is formed - a “sentinel tubercle”, and in the proximal part, i.e. at the level of the dentate line itself, a hyperplastic anal papilla is sometimes determined. Anal papillae are normally thickened distal parts of the valves of the anal columns and have no relation to true polyps of the anal canal. This was clearly shown by V.A. Amineva (1972), but still many surgeons in such cases diagnose an anal polyp, which leads not so much to incorrect actions by the doctor, but to misinformation of patients that is unjustified from the standpoint of deontology.
The length of the crack usually does not exceed 1 cm. Microscopy reveals a defect in the multilayered epithelium with thickening in the area of the edges of the ulcer. The bottom of the ulcer is usually clean, represented by mature granulation or sclerotic connective tissue. Sometimes the scar in the area of the bottom of the crack extends to a depth of 2–5 mm with the inclusion of small nerves and muscle bundles. In some cases, the inflammation is mild or completely absent, but in other cases the inflammation is significant and is sometimes accompanied by the occurrence of a fistula.
Clinical picture
The clinical picture of an anal fissure consists of a triad: pain in the anus, spasm of the anal sphincter, bleeding from the anus
. This is so typical and so clearly revealed during the first interview of the patient that in typical cases the diagnosis is clear even before the examination. If the fissure is combined with hemorrhoids, then prolapse of nodes and more profuse rectal bleeding are usually added to the complaints. Pain that intensifies during defecation causes spasm of the muscular structures of the anal sphincter, and spasm only intensifies the pain. Bleeding from the anal canal is relatively small, occurs during or immediately after defecation and is explained by injury to the walls of the fissure by dense feces (especially with constipation).
For sharp cracks
the pain is usually severe, but relatively short-lived - only during bowel movements and for 15–20 minutes after it.
Sphincter spasm is usually pronounced, and bleeding is minimal. In case of an acute fissure, only a painful area on the wall of the anal canal (most often on the posterior) is usually detected, and seals, raised edges of the fissure, and a “guard tubercle” at its distal edge may not be detected. With a chronic fissure,
the pain is longer lasting and intensifies not only after stool, but also with prolonged forced positioning. Patients develop a symptom such as “fear of stools.” Patients increasingly begin to resort to various laxatives, enemas, become irritable, and experience insomnia.
Complications
Anal fissure is most often caused by severe pain caused by spasm of the anal sphincter, bleeding from the walls of the anal fissure, as well as acute paraproctitis, which develops as a result of infection through a defect in the mucous membrane into the perirectal tissue.
Diagnostics
During an external examination of the anus, after identifying the area of pain, the patient’s buttocks should be carefully spread apart (preferably in a position on a gynecological chair rather than in a knee-elbow position). In almost all cases, it is possible to see the distal part of the fissure by eye - a red longitudinal or triangular ulcer extending deep into the anal canal. These non-invasive manipulations must necessarily precede a digital examination, which may fail due to severe pain. In such cases, you cannot force the digital examination of the anal canal.
During a digital examination of patients with chronic fissures, it is possible to clearly determine not only its exact location, but also the condition of the edges (dense, raised). Pay attention to the presence or absence of purulent discharge (differentiation from an incomplete internal fistula of the rectum) and, very important, determine the degree of sphincter spasm. It is a digital examination before sphincterometry that can give an experienced doctor information about the presence of a spasm: the sphincter, with increased tone, tightly covers the finger, which becomes difficult to move, and manipulation becomes very painful. In this case, the condition of the walls of the anal canal, the presence and consistency of the anal papillae, and the tension of the distal portions of the levator ani muscles are determined.
Instrumental diagnostic methods (anoscopy, rigid sigmoidoscopy) in cases of severe pain and sphincter spasm should not be performed without anesthesia. Sigmoidoscopy to a height of 20–25 cm can be performed either after the fissure has healed, or after surgery, before the patient is discharged from the hospital. You should not specifically perform sphincterometry in case of an acute fissure, although it is necessary to determine the functional state of the anal sphincters.
The most typical clinical signs of anal sphincter spasm are the presence of prolonged intense pain that occurs after defecation, difficulty in defecation and a sharp increase in the anal reflex. With an anal fissure, the main changes in the function of the obturator apparatus of the rectum are reduced to a spasm of the internal sphincter. At the same time, no spasm is observed from the external sphincter.
Differential diagnosis
anal fissure is relatively simple. It is necessary to differentiate the fissure primarily from incomplete internal fistulas of the rectum. With an incomplete fistula, as a rule, sphincter spasm is not observed, the pain is much less, and purulent discharge from the anus comes to the fore. Upon digital examination, a clear depression is identified at the bottom of the low-painful ulcer - the fistula cavity.
When diagnosing an anal fissure, you need to be sure that it is an ordinary, “banal” fissure, and not a manifestation of syphilis (gumma), rectal tuberculosis, rare parasitic (actinomycosis) or another disease, for example, anal fissure in Crohn's disease. What helps here is mainly a careful collection of anamnesis, because according to the clinical picture, a “usual” anal fissure can occur in different ways and it can be very difficult to distinguish it from a specific lesion only with the help of digital examination or anoscopy (rectoscopy). It is also necessary to remember about possible anal manifestations of AIDS.
Treatment
Treatment of patients with anal fissure should begin with conservative measures. Treatment of acute (or recurrent chronic) fissure begins with normalization of stool. In many cases (especially with acute postpartum fissure), only regulating the transit of intestinal contents through the colon, changing its consistency during constipation, or curing chronic diarrhea (most often associated with dysbacteriosis) gives a lasting effect. For the period of treatment (an average of 2 weeks), salty, sour foods and alcoholic drinks are excluded from food.
Currently, many combined suppositories are produced ( Gepatrombin G
etc.), which patients can use independently. Anesthetic and sanitizing ointments, produced in bottles, are injected into the anal canal using a special tip. Thus, the drug Hepatrombin G contains anti-inflammatory (heparin and prednisolone) and analgesic (polidocanol) components and is available in the form of suppositories and ointments (a tip for insertion into the anal canal is attached to the tube with the ointment). After stool, before inserting the suppository, a warm (36–38 °C) sitz bath should be prescribed. The same manipulation is performed at night. No antibiotics are prescribed.
The possibility of eliminating spasm of the anal sphincter with the help of drugs containing nitroglycerin or nifedipine in the form of liniments has been proven (Loder P. et al., 1994, etc.). However, the use of these drugs is limited due to their pronounced vasodilating effect and side effects such as headache and weakness.
The described course of treatment, as a rule, leads to significant improvement: the intensity of pain decreases, sphincter spasm decreases. Under all conditions, such a first course of treatment is very important prognostically: its ineffectiveness within 12–15 days is an indication for surgery.
Surgical treatment
Anal fissures should be carried out in case of a chronic course of the disease that is not amenable to conservative therapy. The operation consists of excision along the plane of the crack itself within the healthy mucous membrane. The wound usually heals easily and quickly (within an average of 5–6 days) with a thin scar. The main thing in this operation is to decide whether an additional sphincterotomy needs to be done, and if necessary, then in what way. Without this additional manipulation, in most cases the operation is not successful; a recurrence of the crack occurs due to renewed tonic contractions of the sphincter. A number of patients in whom spasm is not detected before surgery or is only slightly expressed can be permanently cured by only excision of a crack within the healthy mucous membrane. If the spasm is pronounced and it is clear that it needs to be removed (at least temporarily), then in this situation a lateral submucosal sphincterotomy is indicated.
If previously the vast majority of coloproctologists used the technique of open posterior dosed sphincterotomy, now a different trend has emerged. Additional dissection of the anal sphincter through the wound is difficult to accurately dose, if only because the thickness of the dissected wall of the anal canal is different in patients of different sexes and constitutions. These considerations have prompted many coloproctologists around the world to switch to lateral subcutaneous sphincterotomy, proposed by A. Parks (1969). In this case, only the internal sphincter is dissected, since it has been proven that its pathological condition is the source of spasm and pain. A narrow (ophthalmic) scalpel is inserted into the groove separating the external and internal sphincters, and the scalpel blade is turned toward the lumen of the rectum under the control of the doctor’s finger inserted into the anus. Then, in one movement, the internal sphincter is cut from the side, away from the excised fissure, to the wall of the mucous membrane of the anal canal. After the operation, a thin catheter tube and a gauze turunda soaked in water-soluble antiseptic ointment are inserted into the anus.
In the postoperative period, which usually takes place on an outpatient basis, only hygienic measures are necessary. For a week, you need to take daily sitz baths and ointment applications to the anal canal wound. The patient needs to achieve daily soft stools not only in the immediate postoperative period, but also in the future.
Forecast.
Conservative treatment and surgical intervention, carried out taking into account the functional state of the obturator apparatus of the rectum, ensure recovery in 98–100% of patients.
Surgical treatment
Proctologists believe that if drug therapy is ineffective within six weeks, the process has become chronic. In this case, at an early stage of the disease, surgeons at the proctology department use gentle, minimally invasive techniques. In advanced cases, the affected tissue is removed surgically. If the anal fissure does not heal after excision, combined treatment is performed.
Minimally invasive surgical interventions do not require general anesthesia, are well tolerated and make it possible to avoid traumatic surgery. Proctologists use the following procedures:
- laser treatment of altered tissues;
- infrared photocoagulation;
- cryodestruction;
- excision of pathologically changed tissues with a radio wave scalpel.
Laser excision of anal fissure has the following advantages over surgery performed with a surgical scalpel:
- painlessness;
- antiseptic effect;
- no blood loss;
- low likelihood of complications;
- absence of scar changes in the future;
- short rehabilitation period.
The healing process after excision of an anal fissure using a laser scalpel is quick and painless.
Infrared coagulation of anal fissure is a short procedure. Its duration does not exceed 20 minutes. It allows proctologists to effectively treat rectal fissures without hospitalization and complications. The use of infrared coagulation leads to complete cure in 90% of patients.
Cryodestruction of anal fissures is performed using special devices. The proctologist freezes the lesions at a low temperature. The postoperative period is characterized by slight pain. Healing after excision of an anal fissure with cold occurs quickly, and re-formation of an ulcer rarely occurs.
Radio wave excision of an anal fissure using the surgitron apparatus involves a non-traumatic incision and subsequent coagulation of soft tissues, which is carried out without the use of a scalpel. Rehabilitation after excision of an anal fissure with a radio wave scalpel occurs quickly. After the procedure, no scars are formed and no complications arise. Radio wave excision of anal fissure with surgitron has the following advantages:
- high efficiency - in 9 out of 10 cases complete recovery is observed;
- reliability – the effectiveness of the method has been confirmed not only by years of practice, but also by numerous studies;
- speed - the procedure takes less than half an hour.
Proctologists at Yusupov Hospital do not perform radio wave treatment of anal fissure if there are contraindications: diabetes, epilepsy, cancer, inflammatory processes. Excision of anal fissure with surgitron is not performed during pregnancy.
If conservative therapy and minimally invasive procedures are ineffective, proctologists at the Yusupov Hospital use surgical methods to treat anal fissure. Surgeons at the proctology department masterfully perform the following surgical interventions:
- lateral subcutaneous sphincterotomy with dissection of the muscle around the anus;
- pneumodivulsion (balloon expansion) of the sphincter;
- excision of fissure tissue in combination with medications that relax the sphincter.
Relapse after excision of an anal fissure when using these techniques is rare. Surgery is effective in 95–100% of patients. The sooner the patient contacts a proctologist, the higher the chance of a successful outcome without side effects. After excision of an anal fissure, the reviews are positive. Recovery after excision of an anal fissure occurs quickly if the patient follows the recommendations of the proctologist.
Make an appointment
Diet after surgery
Patients are offered a diet of predominantly fermented milk and vegetable origin. Spicy, salty, bitter foods and irritating seasonings, as well as alcoholic drinks, including beer, are excluded from the diet. Fiber is introduced into the diet, which is found in vegetables, fruits, vegetables, whole grain bread, and cereals. Dried apricots and prunes, flax seeds and bran have a good effect on the intestines, preventing constipation.
Patients are advised to drink a sufficient amount of fluid, preferably pure still water - at least two liters per day. It also helps relieve constipation. Doctors also recommend drinking compotes from seasonal low-allergenic fruits and a small amount of natural juices. Diet therapy is an effective method of preventing complications after excision of anal fissure and relapse of the disease.
To regulate intestinal motility, doctors use antispasmodics and prokinetics. The drug is selected individually depending on the clinical situation. In patients with irritable bowel syndrome with a predominance of constipation, proctologists use antispasmodic drugs: dicetemil, meteospasmin, duspatalin, spasmomen, buscopan. Patients with atonic constipation are prescribed prokinetics (coordinax, cisapride). The use of drugs that regulate motor function is combined with the intake of dietary fiber and osmotic laxatives.
Treatment after excision
Treatment after excision of an anal fissure consists of introducing ointments and suppositories, relief, ultraproct, posterizan, and proctosedyl into the anus. In the postoperative period, phlebotropic drugs, analgesics and non-steroidal anti-inflammatory drugs are prescribed. Motility regulators are combined with the intake of dietary fiber and osmotic laxatives. As dietary fiber, products of plant origin are used that contain non-fermentable substances, mainly of a polysaccharide nature: wheat bran, cellulose, hemicellulose, lignin. Their ability to bind water and regulate the consistency of stool, increasing its mass and accelerating the movement of intestinal contents, speeds up the recovery process after excision of anal fissure. At the initial stage of treatment, osmotic laxatives are used that imitate the effect of dietary fiber: Duphalac, Forlax. If there is a tendency to diarrhea after excision of an anal fissure, adsorbents (Smecta, Neointestopan, Polyphepan), enzyme and bacterial preparations that improve absorption (Creon, Festal, Baktisubtil, Hilak-Forte) are used.
Due to the fact that after excision of an anal fissure the fear of stool often persists, patients are delayed from bowel movements on their own for 2-3 days. From the 4th or 5th day of the postoperative period, to reduce postoperative pain and facilitate emptying of the rectum, before each bowel movement a microenema is given in a volume of 70 to 100 ml of warm water with the addition of 30 ml of petroleum jelly. Subsequently, against the background of healing of the postoperative wound, taking osmotic laxatives and dietary fiber, normal bowel movements are restored and pain is relieved.
In order to undergo effective treatment for anal fissure at an affordable price, make an appointment with a proctologist at the Yusupov Hospital by phone. The cost of minimally invasive procedures and anal fissure excision in the proctology department is lower than in other proctology clinics.
Make an appointment